Superbug Research Summary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Neomycin and Polymyxin B Sulfates Solution for Irrigation, USP Rx Only
NEOMYCIN AND POLYMYXIN B SULFATES- neomycin and polymyxin b sulfates solution X-GEN Pharmaceuticals, Inc. ---------- Neomycin and Polymyxin B Sulfates Solution for Irrigation, USP Rx Only NOT FOR INJECTION DESCRIPTION Neomycin and Polymyxin B Sulfates Solution for Irrigation is a concentrated sterile antibiotic solution to be diluted for urinary bladder irrigation. Each mL contains neomycin sulfate equivalent to 40 mg neomycin base, 200,000 units polymyxin B sulfate, and Water for Injection, inactive ingredient: sulfuric acid. The 20-mL multiple dose vial contains, in addition to the above, 1 mg methylparaben (0.1%) added as a preservative. Neomycin sulfate, an antibiotic of the aminoglycoside group, is the sulfate salt of neomycin B and C produced by Streptomyces fradiae It has a potency equivalent to not less than 600 mcg of neomycin per mg. The structural formulae are: Polymyxin B sulfate, a polypeptide antibiotic, is the sulfate salt of polymyxin B1 and B2 produced by the growth of Bacillus polymyxa. It has a potency of not less than 6,000 polymyxin B units per mg. The structural formulae are: CLINICAL PHARMACOLOGY After prophylactic irrigation of the intact urinary bladder, neomycin and polymyxin B are absorbed in clinically insignificant quantities. A neomycin serum level of 0.1 mcg/mL was observed in three of 33 patients receiving the rinse solution. This level is well below that which has been associated with neomycin-induced toxicity. When used topically, polymyxin B sulfate and neomycin are rarely irritating. Microbiology: The prepared Neomycin and Polymyxin B Sulfates Solution for Irrigation is bactericidal. The aminoglycosides act by inhibiting normal protein synthesis in susceptible microorganisms. -

Consideration of Antibacterial Medicines As Part Of
Consideration of antibacterial medicines as part of the revisions to 2019 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) Section 6.2 Antibacterials including Access, Watch and Reserve Lists of antibiotics This summary has been prepared by the Health Technologies and Pharmaceuticals (HTP) programme at the WHO Regional Office for Europe. It is intended to communicate changes to the 2019 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) to national counterparts involved in the evidence-based selection of medicines for inclusion in national essential medicines lists (NEMLs), lists of medicines for inclusion in reimbursement programs, and medicine formularies for use in primary, secondary and tertiary care. This document does not replace the full report of the WHO Expert Committee on Selection and Use of Essential Medicines (see The selection and use of essential medicines: report of the WHO Expert Committee on Selection and Use of Essential Medicines, 2019 (including the 21st WHO Model List of Essential Medicines and the 7th WHO Model List of Essential Medicines for Children). Geneva: World Health Organization; 2019 (WHO Technical Report Series, No. 1021). Licence: CC BY-NC-SA 3.0 IGO: https://apps.who.int/iris/bitstream/handle/10665/330668/9789241210300-eng.pdf?ua=1) and Corrigenda (March 2020) – TRS1021 (https://www.who.int/medicines/publications/essentialmedicines/TRS1021_corrigenda_March2020. pdf?ua=1). Executive summary of the report: https://apps.who.int/iris/bitstream/handle/10665/325773/WHO- MVP-EMP-IAU-2019.05-eng.pdf?ua=1. -

Antibiotic Temocillin Be A
P0840 Could the ‘old’ antibiotic temocillin be a ‘new’ treatment for acute bacterial cholangitis? A retrospective study of 156 cases Sylvain Chawki1, Marion Duprilot1, Gary Taieb1, Veronique Leflon1, Marie-Hélène Nicolas-Chanoine1, Bruno Fantin1, Victoire De Lastours*1 1 Hôpital Beaujon, Assistance Publique Hôpitaux de Paris, Clichy, France Background: Acute cholangitis is a potentially severe infection requiring rapid active antimicrobial therapy. Thus, emergence of multidrug resistant strains of Enterobacteriaceae is a rising global public-health issue. To spare carbapenems, alternative therapies are needed. Temocillin is a narrow-spectrum betalactam targeting almost specifically Enterobacteriaceae, including most isolates resistant to third generation cephalosporin (3GC) and some carbapenemase-producers. Temocillin biliary concentrations may reach several times the blood concentrations. We assessed whether temocillin may represent an alternative treatment for bacterial cholangitis. Materials/methods: In this retrospective monocentric study, all patients from November 2015 to December 2017 admitted for acute cholangitis with a positive culture (blood or bile) were included. Demographic characteristics, severity, treatment and outcome of each episode were collected. Susceptibility to antibiotics, including temocillin, was determined phenotypically. Episodes of cholangitis were considered susceptible to temocillin if all pathogens found were temocillin-susceptible. Results: 137 patients (77/137 male; 56%; median age 67 [60-75]) who suffered 156 episodes of bacterial cholangitis were included (19 patients had 2 separate episodes during the study period). The median Charlson score was 4 [2-8]; 66/137 (48%) were immunocompromised, 54/137 (39%) had a history episode of acute cholangitis. 118/156 (75.6%) episodes were healthcare-associated, 28/156 (18%) required intensive care and 12 (7.7%) were fatal. -

Chemistry Classification Pharmacokinetics Clinical Uses And
Available online www.jocpr.com Journal of Chemical and Pharmaceutical Research, 2014, 6(11):28-58 ISSN : 0975-7384 Review Article CODEN(USA) : JCPRC5 Chemistry, classification, pharmacokinetics, clinical uses and analysis of beta lactam antibiotics: A review Mamdouh S. Masoud a, Alaa E. Ali b* and Nessma M. Nasr c aChemistry Department, Faculty of Science, Alexandria University, Alexandria, Egypt bChemistry Department, Faculty of Science, Damanhour University, Damanhour, Egypt cStudents’ Hospital, Alexandria University, Alexandria, Egypt _____________________________________________________________________________________________ ABSTRACT This review attempts to pinpoint the importance of betalactam antibiotics, which encompass penicillins, cephalosporins, cephamycins, carbapenems and monobactams from its chemistry, classification, pharmacokinetics, clinical uses and analysis. β- lactam antibiotics have been used for treatment of bacterial infections. Most antibacterials are chemically semisynthetic modifications of various natural compounds and classified on the basis of chemical /biosynthetic origin into natural, semisynthetic, and synthetic. Also, this classification system is based on biological activity; that antibacterials are divided into two broad groups according to their biological effect on microorganisms, bactericidal agents kill bacteria, and bacteriostatic agents slow down bacterial growth. Keywords: Beta lactam Antibiotics, Classification, Pharmacokinetics, Clinical uses, Analysis. _____________________________________________________________________________________________ -

A Thesis Entitled an Oral Dosage Form of Ceftriaxone Sodium Using Enteric
A Thesis entitled An oral dosage form of ceftriaxone sodium using enteric coated sustained release calcium alginate beads by Darshan Lalwani Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Master of Science Degree in Pharmaceutical Sciences with Industrial Pharmacy Option _________________________________________ Jerry Nesamony, Ph.D., Committee Chair _________________________________________ Sai Hanuman Sagar Boddu, Ph.D, Committee Member _________________________________________ Youssef Sari, Ph.D., Committee Member _________________________________________ Patricia R. Komuniecki, PhD, Dean College of Graduate Studies The University of Toledo May 2015 Copyright 2015, Darshan Narendra Lalwani This document is copyrighted material. Under copyright law, no parts of this document may be reproduced without the expressed permission of the author. An Abstract of An oral dosage form of ceftriaxone sodium using enteric coated sustained release calcium alginate beads by Darshan Lalwani Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Master of Science Degree in Pharmaceutical Sciences with Industrial Pharmacy option The University of Toledo May 2015 Purpose: Ceftriaxone (CTZ) is a broad spectrum semisynthetic, third generation cephalosporin antibiotic. It is an acid labile drug belonging to class III of biopharmaceutical classification system (BCS). It can be solvated quickly but suffers from the drawback of poor oral bioavailability owing to its limited permeability through -

Review Article UDC: 615.281.015.8:616.9 Doi:10.5633/Amm.2019.0412
Review article UDC: 615.281.015.8:616.9 doi:10.5633/amm.2019.0412 THE IMPORTANCE OF OLD ANTIBIOTICS IN OVERCOMING RESISTANCE TO ANTIBIOTICS Zorica Jović1, Lidija Ristić2,3, Dane Krtinić1,4, Gorana Nedin-Ranković1, Ana Cvetanović4,5, Dušan Simić6 Antibiotics are medications used to prevent or cure infections caused by bacteria. Discovery and introduction of antibiotics into medical practice brought about revolutionary changes in therapy and eradication of infectious diseases. There is a rise of interest for usage of old antibiotics. These drugs could be invaluable in the treatment of certain infections and, in order for them to remain effective, it is necessary to conduct certain measures which would prove their worth. The aim of antibiotic therapy is to deliver the antibiotic to the place of infection and to retain it in the place of infection for a long period of time. Most of all, it is of utmost importance to educate about this all medical personnel in health care system, especially physicians. The fact that the availability of these drugs remains low in comparison to the efforts made in attempt of discovering new antibiotics, imposes the need for national regulatory agencies to get involved in regulating the usage of these drugs. Acta Medica Medianae 2019;58(4):80-84. Key words: antibiotics, resistance, infections 1University of Niš, Faculty of Medicine, Department of pletely different from contemporary industrially pro- Pharmacology and Toxicology, Niš, Serbia duced ones. Nevertheless, this does not diminish the 2 University of Niš, Faculty of Medicine, Department of Internal fact that certain herbal medicines which have anti- Medicine, Niš, Serbia 3Clinic of Pulmonary Diseases, Clinical center Niš, Niš, Serbia biotic properties were known to ancient Greeks and 4Clinic of Oncology, Clinical center Niš, Niš, Serbia Romans and that they constituted an important part 5University of Niš, Faculty of Medicine, Department of of their medical practices (1). -
Antibiotics in Livestock Farming What Can Be Done to Reduce Environmental Threats and Avoid the Development of Antibiotic Resistance?
Antibiotic resistance threatens human and animal health! Antibiotics in Livestock Farming What can be done to reduce environmental threats and avoid the development of antibiotic resistance? The use of antibiotics in intensive livestock farming pro- motes the development of antibiotic resistance and the spread of resistant bacterial strains. This is a serious problem for both public health and the environment. Today, 700,000 people worldwide die from bacterial infections each year because antibiotics are no longer effective. If decisive action is not taken to combat increasing antibiotic resistance, the number of deaths is expected to increase steadily and reach 10 million annually by 20501. Efforts to counter this development are being undertaken at international2, European,3 and national4 levels. It is clear that measures aimed at solving this problem will only be effec- tive if all parties involved – legislators, the pharmaceutical industry, doctors, patients, livestock farmers, and consum- For decades, treatment with antibiotics of diseases caused ers – play their part. The livestock industry has a special re- by bacterial infections such as diarrhoea, pneumonia, tuber- sponsibility in the fight against antibiotic resistance and the culosis, and certain skin diseases has been highly success- environmental impacts of veterinary pharmaceuticals. ful. In recent years, however, serious infections in humans This background paper is the English translation of the PAN Germany and livestock have again been on the rise. One reason for publication “Antibiotika in der Tierhaltung. Wie lassen sich Umweltbelas- this is the spread of antibiotic-resistant microorganisms. tungen reduzieren und Resistenzen vermeiden”4a. In most cases where What is antibiotic resistance and why does the “national level” is mentioned, this refers to the situation in Germany. -
Shortage of Aztreonam Guidance Document.Pdf
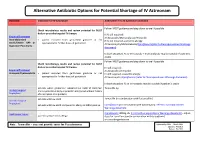
Alternative Antibiotic Options for Potential Shortage of IV Aztreonam Guidance Indication for IV Aztreonam Alternative if no IV Aztreonam available Follow IVOST guidance and step down to oral if possible. Check microbiology results and review potential for IVOST daily or prescribe targeted IV therapy If IV still required: Empirical Treatment IV Amoxicillin/Metronidazole/Temocillin Intra-abdominal • patient excluded from gentamicin guidance or not If IV still required + pencillin allergy: sepsis/Severe HAP or appropriate for further doses of gentamicin IV Vancomycin/Metronidazole/Ciprofloxacin(refer to Fluoroquinolones Warnings Aspiration Pneumonia document) In both situations IV co-trimoxazole + metronidazole may be suitable if patient is stable Follow IVOST guidance and step down to oral if possible. Check microbiology results and review potential for IVOST daily or prescribe targeted IV therapy IV still required: Empirical Treatment IV Amoxicillin /Temocillin Urosepsis/Pyelonephritis • patient excluded from gentamicin guidance or not IV still required + pencillin allergy: appropriate for further doses of gentamicin IV Vancomycin /Ciprofloxacin (refer to Fluoroquinolones Warnings document) In both situations IV co-trimoxazole may be suitable if patient is stable patients where gentamicin indicated but eGFR 15-30ml/min Temocillin 1g Urology Surgical and no penicillin allergy or penicillin allergy but without history Prophylaxis of anaphylaxis or angiodema patients with low eGFR Temocillin (in combination with flucloxacillin) Vascular Surgical Prophylaxis patients with low eGFR and penicillin allergy or MRSA positive Ciprofloxacin (in combination with vancomycin): refer to Fluoroquinolones Warnings document Neutropenic Sepsis Ciprofloxacin 400mg tds (refer to Fluoroquinolones Warnings document)– adjust patients with pencillin allergy dose for renal function (in combination with teicoplanin) or consider gentamicin Note: Temocillin – does not provide cover for Pseudomonas Approved by AMG: March 2016 Updated: Feb 2019 Review: Feb 2022 . -

(12) Patent Application Publication (10) Pub. No.: US 2010/0028334 A1 Cottarel Et Al
US 20100028334A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2010/0028334 A1 Cottarel et al. (43) Pub. Date: Feb. 4, 2010 (54) COMPOSITIONS AND METHODS TO Publication Classification POTENTIATE COLISTIN ACTIVITY (51) Int. Cl. A638/12 (2006.01) (75) Inventors: Guillaume Cottarel, Mountain AOIN 37/00 (2006.01) View, CA (US); Jamey A 6LX 39/395 (2006.01) Wierzbowski, Stoneham, MA (US) A6IP3L/04 (2006.01) Correspondence Address: CI2O I/68 (2006.01) RONALDI. EISENSTEIN (52) U.S. Cl. ................... 424/130.1: 514/2: 514/9: 435/6 100 SUMMER STREET, NIXON PEABODY LLP BOSTON, MA 02110 (US) (57) ABSTRACT A pharmaceutical composition comprising an antimicrobial (73) Assignee: TRUSTEES OF BOSTON agent and an enhancer of an antimicrobial agent, wherein the UNIVERSITY, Boston, MA (US) enhancer of an antimicrobial agent is an inhibitor of gene, that by inactivating the gene product potentiates the effectiveness (21) Appl. No.: 12/519,336 of the antimicrobial agent. In some embodiments, the phar maceutical composition further comprises a pharmaceuti (22) PCT Filed: Dec. 13, 2007 cally acceptable carrier. In some embodiments, the antimi crobial agent is an antimicrobial peptide Such as a polymyxin, (86). PCT No.: PCT/US07/87397 for example but not limited to colistin. In some embodiments of the present invention provides methods to treat and/or S371 (c)(1), prevent infection of a Subject with a microorganism by (2), (4) Date: Jun. 15, 2009 administering a pharmaceutical composition comprising an antimicrobial agent and an enhancer of an antimicrobial Related U.S. Application Data agent. In some embodiments, the present invention provides (60) Provisional application No. -

Hap-Vap-Guidelines-2016.Pdf
Clinical Infectious Diseases IDSA GUIDELINE Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society 1,a 2,a 3,4 5 6 7 8 9 Andre C. Kalil, Mark L. Metersky, Michael Klompas, John Muscedere, Daniel A. Sweeney, Lucy B. Palmer, Lena M. Napolitano, Naomi P. O’Grady, Downloaded from https://academic.oup.com/cid/article-abstract/63/5/e61/2237650 by IDSA user on 16 October 2018 John G. Bartlett,10 Jordi Carratalà,11 Ali A. El Solh,12 Santiago Ewig,13 Paul D. Fey,14 Thomas M. File Jr,15 Marcos I. Restrepo,16 Jason A. Roberts,17,18 Grant W. Waterer,19 Peggy Cruse,20 Shandra L. Knight,20 and Jan L. Brozek21 1Department of Internal Medicine, Division of Infectious Diseases, University of Nebraska Medical Center, Omaha; 2Division of Pulmonary and Critical Care Medicine, University of Connecticut School of Medicine, Farmington; 3Brigham and Women’s Hospital and Harvard Medical School, and 4Harvard Pilgrim Health Care Institute, Boston, Massachusetts; 5Department of Medicine, Critical Care Program, Queens University, Kingston, Ontario, Canada; 6Division of Pulmonary, Critical Care and Sleep Medicine, University of California, San Diego; 7Department of Medicine, Division of Pulmonary Critical Care and Sleep Medicine, State University of New York at Stony Brook; 8Department of Surgery, Division of Trauma, Critical Care and Emergency Surgery, University of Michigan, Ann Arbor; 9Department of Critical Care Medicine, National -

2000 Dialysis of Drugs
2000 Dialysis of Drugs PROVIDED AS AN EDUCATIONAL SERVICE BY AMGEN INC. I 2000 DIAL Dialysis of Drugs YSIS OF DRUGS Curtis A. Johnson, PharmD Member, Board of Directors Nephrology Pharmacy Associates Ann Arbor, Michigan and Professor of Pharmacy and Medicine University of Wisconsin-Madison Madison, Wisconsin William D. Simmons, RPh Senior Clinical Pharmacist Department of Pharmacy University of Wisconsin Hospital and Clinics Madison, Wisconsin SEE DISCLAIMER REGARDING USE OF THIS POCKET BOOK DISCLAIMER—These Dialysis of Drugs guidelines are offered as a general summary of information for pharmacists and other medical professionals. Inappropriate administration of drugs may involve serious medical risks to the patient which can only be identified by medical professionals. Depending on the circumstances, the risks can be serious and can include severe injury, including death. These guidelines cannot identify medical risks specific to an individual patient or recommend patient treatment. These guidelines are not to be used as a substitute for professional training. The absence of typographical errors is not guaranteed. Use of these guidelines indicates acknowledgement that neither Nephrology Pharmacy Associates, Inc. nor Amgen Inc. will be responsible for any loss or injury, including death, sustained in connection with or as a result of the use of these guidelines. Readers should consult the complete information available in the package insert for each agent indicated before prescribing medications. Guides such as this one can only draw from information available as of the date of publication. Neither Nephrology Pharmacy Associates, Inc. nor Amgen Inc. is under any obligation to update information contained herein. Future medical advances or product information may affect or change the information provided. -

The Bacitracin Biosynthesis Operon of Bacillus Licheniformis ATCC 10716
Research Paper 927 The bacitracin biosynthesis operon of Bacillus licheniformis ATCC 10716: molecular characterization of three multi-modular peptide synthetases Dirk Konzl, Andrea Klensl, Kurt Schbrgendorfer* and Mohamed A Marahiell Background: The branched cyclic dodecylpeptide antibiotic bacitracin, Addresses: ‘Philipps-Universittit Marburg, produced by special strains of Bacillus, is synthesized nonribosomally by a Fachbereich ChemielBiochemie, Hans-Meerwein- StraOe, 35032 Marburg, Germany. *Biochemie large multienzyme complex composed of the three bacitracin synthetases BAl , GmbH, 6330 Kufstein/Schaftenau, Austria. BA2 and BA3. These enzymes activate and incorporate the constituent amino acids of bacitracin by a thiotemplate mechanism in a pathway driven by a Correspondence: Mohamed A Marahiel protein template. The biochemical features of these enzymes have been studied E-mail: [email protected] intensively but little is known about the molecular organization of their genes. Key words: Bacillus licheniformus, bacitracin, DNA sequence, peptide antibiotics, peptide Results: The entire bacitracin synthetase operon containing the genes synthetases, thiazoline ring bacA-bacC was cloned and sequenced, identifying a modular structure typical of peptide synthetases. The bacA gene product (BAI , 598 kDa) contains five Received: 30 September 1997 Accepted: 28 October 1997 modules, with an internal epimerization domain attached to the fourth; bacB encodes BA2 (297 kDa), and has two modules and a carboxy-terminal Chemistry & Biology December 1997,4:927-937 epimerization domain; bacC encodes BA3, five modules (723 kDa) with http://biomednet.comlelecref/1074552100400927 additional internal epimerization domains attached to the second and fourth. A 0 Current Biology Ltd ISSN 1074-5521 carboxy-terminal putative thioesterase domain was also detected in BA3.