2017 Final Booklet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Physiology H Digestive
2/28/18 Introduction • Provides processes to break down molecules into a state easily used by cells - A disassembly line: Starts at the mouth and ends Digestive System at the anus • Digestive functions are initiated by the parasympathetic division Chapter 29 - Digestion occurs during periods of low activity - Produces more energy than it uses Copyright © 2016 by Elsevier Inc. All rights reserved. 1 Copyright © 2016 by Elsevier Inc. All rights reserved. 2 Anatomy The Digestive System • Oral cavity • Pharynx • Esophagus • Stomach • Small intestine and large intestine • Accessory organs: Pancreas, liver, and gallbladder From Herlihy B: The human body in health and illness, ed 4, St. Louis, 2011, Saunders. Copyright © 2016 by Elsevier Inc. All rights reserved. 3 Copyright © 2016 by Elsevier Inc. All rights reserved. 4 Physiology Gastrointestinal Tract • Ingestion: Taking materials into mouth by • Muscular tube throughout digestive system eating/drinking • Accessory organs and glands secrete • Digestion: Breaking down food into molecules substance to aid in digestion that can be used by the body • GI tract wall has four layers: - Includes mechanical and enzymatic action - Mucosa • Absorption: Simple molecules from the - Submucosa gastrointestinal (GI) tract move into the - Muscle layer: Responsible for peristalsis bloodstream or lymph vessels and then into - Serosa body cells • Defecation: Eliminating indigestible or unabsorbed material from the body Copyright © 2016 by Elsevier Inc. All rights reserved. 5 Copyright © 2016 by Elsevier Inc. All rights reserved. 6 1 2/28/18 Peristalsis Oral Cavity • First portion of GI tract • Contains: - Teeth - Tongue - Openings for salivary glands From Thibodeau GA, Patton KT: Anatomy & physiology, ed 6, St. -

Severe Gastroparesis Following Radiofrequency Catheter Ablation for Atrial Fibrillation: Suggestion for Diagnosis, Treatment, and Device for Gastroparesis After RFCA
Hindawi Publishing Corporation Case Reports in Gastrointestinal Medicine Volume 2014, Article ID 923637, 6 pages http://dx.doi.org/10.1155/2014/923637 Case Report Severe Gastroparesis following Radiofrequency Catheter Ablation for Atrial Fibrillation: Suggestion for Diagnosis, Treatment, and Device for Gastroparesis after RFCA Dong Seok Lee1 and Sang Jin Lee1,2 1 Department of Internal Medicine, Gangneung Asan Medical Center, University of Ulsan College of Medicine, Gangneung, Republic of Korea 2Department of Internal Medicine, Gangneung Asan Medical Center, Sacheon-myeon, Gangneung, Gangwon-do 210-711, Republic of Korea Correspondence should be addressed to Sang Jin Lee; [email protected] Received 18 October 2014; Accepted 11 December 2014; Published 30 December 2014 Academic Editor: Wen-xie Xu Copyright © 2014 D. S. Lee and S. J. Lee. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Gastroparesis following radiofrequency catheter ablation (RFCA) is a very rare complication, as only two cases have been reported in the English literature. A 42-year-old man underwent RFCA due to recurrent drug-resistant symptomatic atrial fibrillation. The patient complained of indigestion and early satiety 2 days after the procedure. Contrast-enhanced computed tomography and an upper gastrointestinal series of the abdomen showed a large amount of material remaining in the stomach area. All food material was removed by endoscopy, and the patient received medical treatment. We suggest a flow chart for diagnosis and treatment of AFGS based on the present case and previous cases. -

E Pleura and Lungs
Bailey & Love · Essential Clinical Anatomy · Bailey & Love · Essential Clinical Anatomy Essential Clinical Anatomy · Bailey & Love · Essential Clinical Anatomy · Bailey & Love Bailey & Love · Essential Clinical Anatomy · Bailey & Love · EssentialChapter Clinical4 Anatomy e pleura and lungs • The pleura ............................................................................63 • MCQs .....................................................................................75 • The lungs .............................................................................64 • USMLE MCQs ....................................................................77 • Lymphatic drainage of the thorax ..............................70 • EMQs ......................................................................................77 • Autonomic nervous system ...........................................71 • Applied questions .............................................................78 THE PLEURA reections pass laterally behind the costal margin to reach the 8th rib in the midclavicular line and the 10th rib in the The pleura is a broelastic serous membrane lined by squa- midaxillary line, and along the 12th rib and the paravertebral mous epithelium forming a sac on each side of the chest. Each line (lying over the tips of the transverse processes, about 3 pleural sac is a closed cavity invaginated by a lung. Parietal cm from the midline). pleura lines the chest wall, and visceral (pulmonary) pleura Visceral pleura has no pain bres, but the parietal pleura covers -

Department of Medicine Lewis Katz School of Medicine at Temple University
Department of Medicine Lewis Katz School of Medicine at Temple University 2017 Annual Fellows, Residents and Medical Students Research Symposium Sol Sherry Awards for Excellence in Research Wednesday, June 7, 2017 Medical Education and Research Building Luo Commons The Fellows and Residents Research Forum was initiated over 35 years ago to provide the Fellows and the Residents in the Department of Medicine with an opportunity to present their research effort. The Forum is a reflection of the ongoing research activities in the Department, and a year-end summation of the projects carried out by the Fellows and Residents. Dedication Dr. Sol Sherry 1916-1993 Sol Sherry, M.D., joined Temple University School of Medicine as professor and chairman of the Department of Medicine in 1968. In 1970, Dr. Sherry founded and served as director of the University's Specialized Center for Thrombosis Research, the largest of its kind in the United States, which was later named in his honor. He served as dean of the School of Medicine from 1984-86. He was a recipient of an honorary doctor of science degree, the University's first Distinguished Professor and was honored with the establishment of the Sol Sherry Chair in Medicine. For his contributions to medical research, teaching and patient care, Dr. Sherry was the recipient of other numerous awards and honors. He was Master of the American College of Physicians and The John Phillips Memorial Medalist of the American College of Physicians; a Fellow of the Royal College of Physicians (London), and recipient of the Robert P. Grant Medal of the International Society on Thrombosis and Hemostasis--a society which he founded in 1977. -

Preparation Instructions for Nuclear Medicine Scans
NUCLEAR MEDICINE UNM HEALTH SCIENCES CENTER 2211 LOMAS NE ALBUQUERQUE, NM 87106 505-272-2421 (M-F 8:00AM – 4:30PM) Preparation Instructions for Nuclear Medicine Scans (Schedulers/Technologists: Please consult with Protocol sheets for additional important details) Procedure Preparation Duration of Exam Bone Scan No Prep Injection (15 minutes), then return 3 hours later for scan (45 minutes - 1 hour) Brain SPECT No Prep 1-1½ hours Cardiac perfusion – Technetium Agents See special instructions under Cardiac 3-5 hours preparation instructions Cisternogram and Cisternogram for Leak No Prep 2-3 days, 1-2 hours each day, morning and afternoon CSF Shunt Study No Prep Depending on each individual case Gallium Scan No Prep Depending on each individual case, usually requires multiple images over several days Gastric Emptying Scan (adults and Nothing by mouth for 6 hours except small 4-5 hours children approximately 4-5 yrs old and amount of water as needed for medications. up, with standardized meal of Egg Beaters, jam, and toast Diabetic patients should bring their usual diabetes medications (insulin and/or pills). Call Nuclear Medicine if you cannot eat Egg Beaters (egg whites), jam, or toast. Gastric Emptying Scan – Liquid – with Nothing by mouth for 4 hours 1-5 hours depending on protocol or without reflux (typically children Less time (2 hours) may be OK for infants and under 2-3 years old) very small children. Call Nuclear Medicine with questions. Gastrointestinal (GI) Bleeding Study No Prep 2-3 hours Glomerular Filtration Rate -- GFR (Gates Drink lots of fluids before the exam 15 minutes Method) Hemangioma No Prep 2-3 hours Hepatobiliary (HIDA) Scan For acute or chronic cholecystitis: 2 hours; may have to return for additional 1. -

Current Diagnosis and Treatment of Gastroparesis: a Systematic Literature Review
DOI: https://doi.org/10.22516/25007440.561 Review article Current diagnosis and treatment of gastroparesis: A systematic literature review Viviana Mayor,1* Diego Aponte,2 Robin Prieto,3 Emmanuel Orjuela.4 Abstract OPEN ACCESS Normal gastric emptying reflects a coordinated effort between different Citation: regions of the stomach and the duodenum, and also an extrinsic modu- Mayor V, Aponte D, Prieto R, Orjuela E. Current diagnosis and treatment of gastroparesis: lation by the central nervous system and distal bowel factors. The main A systematic literature review . Rev Colomb Gastroenterol. 2020;35(4):471-484. https://doi. org/10.22516/25007440.561 events related to normal gastric emptying include relaxation of the fundus to accommodate food, antral contractions to triturate large food particles, ............................................................................ the opening of the pyloric sphincter to allow the release of food from the 1 Internist and professor, Clínica Versailles, Universidad Javeriana. Cali, Colombia. stomach, and anthropyloroduodenal coordination for motor relaxation. 2 Gastroenterology Service, Area Coordinator, Clínica Universitaria Colombia. Bogotá, Colombia. Gastric dysmotility includes delayed emptying of the stomach (gastropare- 3 Gastroenterologist, Clínica Universitaria Colombia. Bogotá, Colombia. sis), accelerated gastric emptying (dumping syndrome), and other motor 4 Medical doctor. Universidad Javeriana. Clínica Versalles. Cali, Colombia. dysfunctions, e.g., deterioration of the distending fundus, -

Insurances, Precertification Requirements, Services Offered, As Well As Guidelines, Fees, and Education Information
This resource book is presented to provide you and your staff with basic information regarding: Insurances, precertification requirements, services offered, as well as guidelines, fees, and education information. This does not intend to be all encompassing, and some information does have limitations as well and expirations. Radiology Associates intends to keep you abreast of the newest and most up-to-date fees, guidelines, and regulations as we can. Please contact us if you have any further questions or we can be of further service to you. 887-7000 Radiology Associates, LLP Toll Free Phone 887-626-8678 General Correspondence and Billing Address: P.O. Box 5608 Corpus Christi, TX 78465 Patient Payment Address: P.O. Box 6010 Corpus Christi, TX 78466-6010 Business Office Physical Address: 1812 S. Alameda Corpus Christi, TX 78404 Mammogram Payment Guidelines Medicare Age 35–39 Baseline Mammogram Age 40+ Mammogram every year – (eleven full months must have elapsed following the month of the last mammogram) Note: Count months between mammographies beginning the month after the date of the examination. For example, screening mammogram received January 20, 2004; begin counting next month (February 2004) until 11 months have elapsed. Payment can be made for another screening mammogram beginning January 1, 2005. Medicaid (See Medicaid Guide) Age 35-39 Baseline Mammogram Age 45+ Mammogram every year (must be one full year) Tricare (Champus) (See Attached) Age 39+ Mammogram every year Age 35 High Risk and annually thereafter Note: women at high risk (family history of breast cancer in a first degree relative) baseline mammogram is payable at age 35 and then annually. -

Study 1: Effect of Saliva on B2T
Stability of b2-transferrin and b-trace protein Lyn Boscato Chemical Pathology, St Vincent’s Hospital, Sydney, Australia. [email protected]; Introduction and Aim Study 1: Effect of saliva on B2T b2-transferrin (B2T) and b-trace protein (BTP) are useful markers for SUSPECTED SAMPLE PROBLEM the diagnosis of CSF leakage. A sample received for routine investigation of a suspected CSF Specimens received for analysis are often heavily contaminated with leak was negative for BTP but the transferrin isoform pattern other substances (eg blood, serous fluid, saliva, bacteria, mucus) and suggested CSF presence. Sample was an oral fluid collection so stored under non-ideal conditions (not frozen, large container, very small sample volume, on swabs). sialidase presence was suspected as the oral cavity can have a high bacterial load The aim of this study was to investigate the stability of B2T and BTP in 1 2 3 4 5 the presence of potential contaminants. 1 - CSF 4 - serum+ saliva STUDY 2 - CSF + saliva 5 - serum To determine if saliva contains sialidase 3 - saliva • • Saliva collected by passive drooling and microfuged to remove Figure 1. Transferrin isoforms detected following particulates. Methods IEF- western blotting for CSF and serum incubated • Equal volumes of saliva and serum or CSF were incubated with and without saliva. overnight at RT • Transferrin isoforms detected STUDIES Investigation of the stability of B2T and BTP incubated in the presence of a. saliva as a source of sialidase (enzyme which removes sialic acid from glycoproteins. Normally arises from bacterial or viral Study 2: Stability of B2T and BTP sources). -

Current Models of Ovarian Cancer
Iowa State University Capstones, Theses and Creative Components Dissertations Fall 2018 Current Models of Ovarian Cancer Ruth Hines Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/creativecomponents Part of the Investigative Techniques Commons, Obstetrics and Gynecology Commons, Oncology Commons, and the Women's Health Commons Recommended Citation Hines, Ruth, "Current Models of Ovarian Cancer" (2018). Creative Components. 65. https://lib.dr.iastate.edu/creativecomponents/65 This Creative Component is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Creative Components by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. Ruth Hines Creative Component Dr. Gunnar Mair Current Models of Ovarian Cancer ABSTRACT Ovarian cancer has proved to be one of the most difficult cancers to treat. It is often diagnosed in the late stages. When it is detected early, the 5-year survival rate is 93%. However, it is only detected early 15% of the time. For this reason, there is an emphasis on finding better tumor markers that can identify cancerous cells early. Ovarian cancers come from 3 different cell types. There are a variety of cancer subtypes from each type of cell. A one- size fits all treatment method isn’t feasible with so much variation. Models of ovarian cancer help understand the pathway of cancer development, find tumor markers for early detection, improve imagining techniques, and test drug therapies. Current models include transgenic mice, xenograft mice, chick chorioallantoic membrane, the laying hen, and 3-D human tissue cultures. -
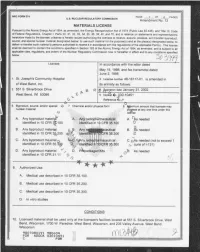
Matls Licensing Package for Amend 12 to License 48-16117-01 for St
_ _---____ -___ _ - _ _ _ _ _ _ _ _ - - _ _ _ _ _ _ - _ _ _ _ - _ _ - - - - _ _ - - - - _ _ - - - - - _ _ _ _ _ - - - - - - - - - - - - - - - - - - - - - - - - - - . u.S. NUCLEAR REGULATORY Commission g g MATERIALS LICENSE Pursuant to the Atomic Energy Act of 1954, as amended, the Energy Reorganization Act of 1974 (Public Law 93-438), and Title 10 Code of Fed:ral Regulations, Chapter I, Parts 30,31,32,33,34,35,36,39,40, and 70, and in reliance on statements and representations heretofore made by the licensee, a license is hereby issued authorizing the licensee to receive, acquire, possess, and transfer byproduct, source, and special nuclear material designated below; to use such material for the purpose (s) and at the place (s) designated below; to deliver or transfer such material to persons authorized to receive it in accordance with the regulations of the applicable Part(s). This license , sh:ll be deemed to contain the conditions specified in Section 183 of the Atomic Energy Act of 1954, as amended, and is subject to all I applicable rules, regulations, and orders of the Nuclear Regulatory Commission now or hereafter in effect and to any conditions specif'e d c. Ucensee In accordance with the letter dated May 19,1998, and fax transmittal dated June 2,1998 1. St. Joseph's Community Hospital 3. Ucense number 48-16117-01 is amended in of West Bend, Inc. Its entirety as follows: 2. 551 S. Silverbrook Drive g R le. gpiration date January 31,2002 W st Bend, WI 53095 Y- b 5. -

Society of Nuclear Medicine
SNMMI Board of Directors Meeting Saturday, April 25, 2020 REMOTE – Virtual Meeting via Web-Ex Minutes – APPROVED Members in Attendance: Vasken Dilsizian, MD; Alan Packard, PhD; Richard Wahl, MD, FACNM; Cathy S. Cutler, PhD; Satoshi Minoshima, MD, PhD; Mark Crosthwaite, CNMT, FSNMMI-TS; Twyla Bartel, DO, MBA, FACNM; Norman E. Bolus, MSPH, MPH, CNMT, FSNMMI-TS; Tina Buehner, MS, CNMT, NMTCB(CT)(RS), RT(N)(CT), FSNMMI-TS; Ryan Niederkohr, MD; Giuseppe Esposito, MD, MBA; Sarah Frye, MBA, CNMT, PET, CCRP; Suzanne E. Lapi, PhD; Dusty M. York, CNMT, PET, RT(N)(CT); Munir Ghesani, MD, FACNM, FACR; Frederick Grant, MD; Frances K. Keech, DHSc, RT(N), FSNMTS; Umar Mahmood, MD, PhD; Michael L. Middleton, MD, CPE, FACNM; Virginia Pappas, CAE; Todd E. Peterson, PhD Staff in attendance: Sukhjeet Ahuja, MD; Angela Boyd; Linda Budzinski; Bonnie Clarke; Sharon Gleason; Ali Haidar; Paul Hamel; Ann Latham; Rebecca Maxey; Vince Pistilli, CPA; Amy Schull; Nikki Wenzel Lamb, MBA, CAE 1. Welcome and Call to Order Vasken Dilsizian, MD, SNMMI President, called the meeting to order at 10:01am (ET). Dr. Dilsizian thanked the board members for participating on the weekend calls as it is important that we continue to make progress. a. Establishment of a Quorum Cathy S. Cutler, PhD, Secretary/Treasurer, reported that a quorum was present. b. Approval of Agenda and Standing Rules Dr. Dilsizian reviewed the agenda and asked the members to approve the agenda. It was moved, seconded and voted to approve the April 25, 2020 SNMMI Board of Directors virtual meeting agenda. c. Approval of Meeting Minutes Cathy S. -

Biomedical Terminology
Biomedical Terminology Respiratory System Terminology Respiratory Structure • Nose • Pharynx • Larynx • Trachea • Bronchi • Bronchioles • Alveoli The Pharynx (pharyng/o) • The pharynx is a common passageway for air and food The Larynx (laryng/o) • The larynx is an enlargement in the airway superior to the trachea and inferior to the pharynx • It helps keep particles from entering the trachea and also houses the vocal cords • Consists of the vocal cords and the epiglottis (epiglott/o) – During normal breathing, the vocal cords are relaxed and the glottis is a triangular slit. – During swallowing, the false vocal cords and epiglottis close off the glottis The Trachea (trache/o) • The trachea extends downward anterior to the esophagus and into the thoracic cavity, where it splits into right and left bronchi • The inner wall of the trachea is lined with ciliated mucous membrane with many goblet cells that serve to trap incoming particles • The tracheal wall is supported by 20 incomplete cartilaginous rings The Bronchial Tree • The bronchial tree consists of branched tubes leading from the trachea to the alveoli – The bronchial tree begins with the two primary bronchi, each leading to a lung – The branches of the bronchial tree from the trachea are right and left primary bronchi; these further subdivide until bronchioles give rise to alveolar ducts which terminate in alveoli – It is through the thin epithelial cells of the alveoli that gas exchange between the blood and air occurs – Combining forms • Alveolus – alveol/o • Bronchus – bronch/o,