Montreal and Boston
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Why Cant I Download Chance the Rapper Old Albums Truth About Chance the Rapper’S Net Worth and Story Behind His Admirable Humility
why cant i download chance the rapper old albums Truth About Chance the Rapper’s Net Worth and Story Behind His Admirable Humility. Chancelor Johnathan Bennett, better known by his stage name Chance the Rapper, is an American rapper, singer, songwriter, record producer, and actor. Bennett gained initial fame in 2012 after releasing his debut mixtape titled ‘10 Day.’ He achieved mainstream success in 2013 following the release of his second mixtape, Acid Rap. Chancelor’s rapping career finally took off in 2016 with the release of his third mixtape titled Coloring Book. The mixtape earned him three Grammy Awards and became the first ever streaming-only album to win a Grammy Award. It peaked at #8 on the US Billboard 200. Chancelor Bennett’s debut studio album ‘The Big Day’ was eventually released on July 26, 2019. The album, which is Bennett’s only studio album to date, is famous for its matrimonial-themed songs. Bennett’s music is versatile, blending uplifting jazz-inspired melodies with gospel influences. He often uses choirs to amplify the gospel undertones in his music. In addition to his solo career, Chancelor Bennett is the vocalist for the music band, The Social Experiment. The band is best known for their album Surf, released in May 2015. Bennett is also a member of the Chicago-based collective Savemoney. Chancelor Bennett has also pursued a fairly successful acting career. He made his television debut in 2013, appearing as himself in The Eric Andre Show and The Arsenio Hall Show. In 2018, Bennett made his cinematic debut in the movie Slice. -
Which Canadian Charities Had the Largest Assets in 2014?
www.canadiancharitylaw.ca Which Canadian charities had the largest assets in 2014? By Mark Blumberg (March 23, 2016) We recently reviewed the T3010 information for 2014. It covers about 84,370 of the 86,000 registered charities that have so far filed their return and that have been entered into the CRA’s database. Canadian registered charities are currently required to disclose on the T3010 their assets. The total assets of all the 84,370 registered charities were about $373,050,327,255.00. Below we have a table of Canadian charities and how much they spent as reported for the 2014 fiscal year. Thank you to Celeste Bonas, an intern at Blumbergs, for helping with this project. The Sean Blumberg Transparency Project is in memory of my youngest brother Sean Blumberg. Sean was a sweet, kind person, a great brother who helped me on a number of occasions with many tasks including the time consuming and arduous task of reviewing T3010 databases and making them into something useful. As part of the Sean Blumberg Transparency Project, Blumbergs has been releasing information on the Canadian charity sector to provide a better understanding of the size, scope, complexity and challenges of the sector. Please review my caveats at the end about the reliability and usage of T3010 information. 1 www.canadiancharitylaw.ca List of Canadian charities with the largest assets in 2014 Line 4200 Name of Canadian Registered Charity largest assets 1. ALBERTA HEALTH SERVICES $9,984,222,000.00 2. THE MASTERCARD FOUNDATION $9,579,790,532.00 3. THE GOVERNING COUNCIL OF THE UNIVERSITY OF TORONTO $7,681,040,000.00 4. -
2015 Annual Report
1 TABLE OF CONTENTS TABLE OF CONTENTS ............................................................................................................................. 2 HISTORY OF THE GAIRDNER FOUNDATION .................................................................................... 3 MISSION ...................................................................................................................................................... 3 NATIONAL AND STUDENT OUTREACH PROGRAMS ....................................................................... 4 MESSAGE FROM THE CHAIR ............................................................................................................... 5 MESSAGE FROM THE PRESIDENT/SCIENTIFIC DIRECTOR ......................................................... 6 2015 YEAR IN REVIEW ............................................................................................................................. 7 REPORT ON 2015 OBJECTIVES ............................................................................................................ 14 THE YEAR AHEAD: OBJECTIVES FOR 2016 ..................................................................................... 16 THE GAIRDNER FOUNDATION VALUES OUR 2015 SPONSORS ................................................... 18 GOVERNANCE ......................................................................................................................................... 20 MEDICAL REVIEW PANEL 2015 ......................................................................................................... -

2015 Annual Summary Corporate Plan
The Gairdner Foundation Corporate Plan 2015 1 TABLE OF CONTENTS PAGE Section I About the Gairdner Foundation 2 Objectives and Achievements to Date 5 Benefits 7 Section II Performance Results for 2014 Activities 7-8 Detailed 2014 Evaluations 9-10 Planned Activities and Anticipated Results 2015 11 Section III Financial Summary 12 Planned Receipts and Disbursements 2015 13-15 Section IV Risk Management 16 Section V Performance Monitoring 17-19 2 THE GAIRDNER FOUNDATION CORPORATE PLAN EXECUTIVE SUMMARY HISTORY The Gairdner Foundation was created by James A. Gairdner to recognize and reward the achievements of medical researchers whose work “contributes significantly to improving the quality of human life”. The Foundation is a Canadian organization that has never lost sight of its primary mission – the recognition of scientists it deemed to have made the most important breakthrough discoveries in biomedical science. It’s recipients are responsible for the discovery of the structure of DNA, the eradication of smallpox, CT scans, MRI machines, the human genome, the cure for ulcers, and the vaccine against HPV, to name a few. Since the first awards were granted in 1959, the Canada Gairdner Awards have become Canada's foremost international award- and one of the most prestigious awards in medical science. Our track record of consistent high quality adjudication and selection by the independent adjudication committees have resulted in global recognition and esteem. The Gairdner was incorporated in December 1957 as a charitable corporation under the laws of the Province of Ontario, Canada. During 2013, the Foundation was continued as a federal corporation under the Canada Not-For-Profit Corporations Act. -

Chapter Xxiv
CHAPTER XXIV. Crown lands management Waste lands in seigniories Government officials Army bills redeemed Banking Political situation, 1816 The two Papineaus Sessions of 1817-1819 Death of George III., 1820 A speech of Louis-Joseph Papineau. To portion out the lands amongst the militia, General Drummond, the administrator of the province (1815), was constrained to have recourse to the officials of a department in which enormous abuses existed. The lands were divided up between favourites. So much territory had been given away that Drummond informed the minister that there was no more room on the River St. Francis for the establishment of the immigrants and the discharged soldiers. Every one had pounced down upon that immense pasture ground. From 1793 to 1811, over three million acres had been granted to a couple of hundred privileged applicants. Some of them secured as much as sixty to eighty thousand acres as, for example, Governor Milnes, who took nearly seventy thousand as his share. These people had no intention of ever improving the land by clearing it of the forest. As it cost them nothing, they purposed leaving the same in a wild state until such time as the development of the neigh- bourhood by colonization would increase the value of the whole. Another vexatious land question arose out of the vast domains granted by the King of France to the so-called seigneurs which were intended, by the letter and spirit of the grants themselves, to be given to the settlers whenever they wished for them. Large tracts of these still remained unoc- cupied and the seigneurs had often expressed the desire to get them as their own property in free and common socage, whilst the country people main- tained that they were to be kept en seigneurie according to the intention of the sovereign who first granted them. -

Dr. Adolfo J. De BOLD
Dr. Adolfo J. de BOLD September 2015 Page 1 of 40 HOME ADDRESS: OFFICE ADDRESS: 5503 South Island Park Drive Department of Pathology and Laboratory Manotick, Ontario K4M 1J2 Medicine Phone: (613) 692-6194 University of Ottawa, Faculty of Medicine 4155-451 Smyth Road Ottawa, Ontario K1H 8M5 Phone: (613) 562-5422 [email protected] EDUCATION 1961 - 1967 National University of Córdoba, Argentina 1968 Professional Degree: Clinical Biochemist 1968 - 1973 School of Graduate Studies, Queens University, Kingston, Ontario, Canada 1971 M.Sc. (Experimental Pathology) "Studies on the Relationship between the Catecholamine Distribution in the Atrium and the Specific Granules Present in Atrial Muscle Cells" 1973 Ph.D. (Experimental Pathology) "The Relationship Between Morphology and Function in the Atrial Cardiocyte. A study With Emphasis on the Secretory Characteristics of the Mammalian Atrium" PROFESSIONAL APPOINTMENTS 1974 Laboratory Scientist, Pathology Laboratory, Hotel Dieu Hospital, Kingston, Ontario, Canada. 1974 Assistant Professor of Pathology, Department of Pathology, Faculty of Medicine, Queen's University, Kingston, Ontario, Canada (Tenured, 1981). 1982 Associate Professor of Pathology, Faculty of Medicine, Queen's University, Kingston, Ontario, Canada. 1985 Professor of Pathology, Faculty of Medicine, Queen's University, Kingston, Ontario, Canada. 1986-1993 Director of Research, University of Ottawa Heart Institute Research Centre, Ottawa Civic Hospital. 1989-1995 Distinguished Research Professor, Heart and Stroke Foundation of Ontario. 1986-1995 Adjunct Professor of Pathology, Queen's University, Kingston, Ontario, Canada. 1986-2013 Professor of Pathology and Laboratory Medicine Faculty of Medicine, University of Ottawa, Ottawa, Ontario, Canada 1986-2013 Cross-appointment, Department of Cellular and Molecular Medicine, Faculty of Dr. Adolfo J. -
(B.Sc.) - Freshman Program (30 Credits) , Page 34
Faculty of Science, including School of Computer Science Programs, Courses and University Regulations 2011-2012 This PDF excerpt of Programs, Courses and University Regulations is an archived snapshot of the web content on the date that appears in the footer of the PDF. Archival copies are available at www.mcgill.ca/study. This publication provides guidance to prospects, applicants, students, faculty and staff. 1 . McGill University reserves the right to make changes to the information contained in this online publication - including correcting errors, altering fees, schedules of admission, and credit requirements, and revising or cancelling particular courses or programs - without prior notice. 2 . In the interpretation of academic regulations, the Senate is the final authority. 3 . Students are responsible for informing themselves of the University's procedures, policies and regulations, and the specific requirements associated with the degree, diploma, or certificate sought. 4 . All students registered at McGill University are considered to have agreed to act in accordance with the University procedures, policies and regulations. 5 . Although advice is readily available on request, the responsibility of selecting the appropriate courses for graduation must ultimately rest with the student. 6 . Not all courses are offered every year and changes can be made after publication. Always check the Minerva Class Schedule link at https://banweb.mcgill.ca/pban1/bwckschd.p_disp_dyn_sched for the most up-to-date information on whether a course is offered. 7 . The academic publication year begins at the start of the Fall semester and extends through to the end of the Winter semester of any given year. Students who begin study at any point within this period are governed by the regulations in the publication which came into effect at the start of the Fall semester. -
How Suburbia Happened in Toronto
Digital Commons @ Touro Law Center Scholarly Works Faculty Scholarship 2011 How Suburbia Happened In Toronto Michael Lewyn Touro Law Center, [email protected] Follow this and additional works at: https://digitalcommons.tourolaw.edu/scholarlyworks Part of the Land Use Law Commons, Transportation Law Commons, and the Water Law Commons Recommended Citation 6 Fla. A & M U. L. Rev. 299 (2010-2011) This Book Review is brought to you for free and open access by the Faculty Scholarship at Digital Commons @ Touro Law Center. It has been accepted for inclusion in Scholarly Works by an authorized administrator of Digital Commons @ Touro Law Center. For more information, please contact [email protected]. How SUBURBIA HAPPENED IN TORONTO by Michael Lewyn* Review, John Sewell, The Shape of the Suburbs: Understanding To- ronto's Sprawl (University of Toronto Press 2009) TABLE OF CONTENTS I. INTRODUCTION ............................................ 299 II. SPRAWL IN TORONTO ...................................... 301 A. Highways and Transit ................................ 301 1. Creating Sprawl Through Highways .............. 301 2. Transit Responds to Sprawl....................... 303 B. Sewer and Water ..................................... 304 C. Not Just Sprawl, But Low-Density Sprawl............ 305 D. The Future of Sprawl................................. 308 III. A COMPARATIVE PERSPECTIVE ............................. 309 IV . SuMMARY ................................................. 311 I. INTRODUCTION From an American perspective, Toronto may seem like the kind of walkable, transit-oriented city beloved by critics of automobile-de- pendent suburbia. Toronto has extensive subways- and commuter train 2 services, and therefore higher transit ridership than most other Canadian and American cities. 3 While some North American down- * Associate Professor, Florida Coastal School of Law. B.A., Wesleyan University; J.D., University of Pennsylvania; L.L.M., University of Toronto. -

Canadian Association for Irish Studies 2019 Conference
CANADIAN ASSOCIATION FOR IRISH STUDIES 2019 CONFERENCE IRISH BODIES AND IRISH WORLDS May 29 – June 1 CONFERENCE PROGRAMME John Molson School of Business Conference Centre, 9TH Floor Concordia University 1450 Guy Street, Montreal, Quebec, H3G 1M8 We acknowledge that Concordia University is located on unceded Indigenous lands. The Kanien’kehá:ka Nation is recognized as the custodians of the lands and waters on which we gather today. Tiohtiá:ke/Montreal is historically known as a gathering place for many First Nations. Today, it is home to a diverse population of Indigenous and other peoples. We respect the continued connections with the past, present and future in our ongoing relationships with Indigenous and other peoples within the Montreal community. MAY 29, 2019 Graduate Student Master-Class with Kevin Barry and Olivia Smith 3:00 p.m. to 4:00 p.m. School of Irish Studies, McEntee Reading Room (1455 boul. De Maisonneuve West, H 1001) Registration & Opening Reception 5:00 p.m. to 6:15 p.m. School of Irish Studies, McEntee Reading Room & Engineering Lab (1455 boul. De Maisonneuve West, H 1001 & H 1067) Exclusive Preview – Lost Children of the Carricks A documentary by Dr. Gearóid Ó hAllmhuráin Opening words by His Excellency Jim Kelly Ireland’s Ambassador to Canada and Dr. André Roy Dean of the Faculty of the Arts and Science 6:45 p.m. to 8:30 p.m. (De Sève Cinema, 1400 Boulevard de Maisonneuve West, Ground Floor) MAY 30, 2019 Registration – 9:00 to 9:30 a.m. PANEL 1 – MORNING SESSION – 9:30 a.m. -
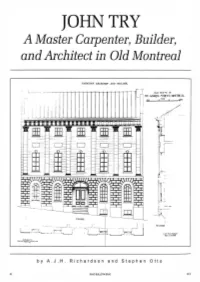
JOHN TRY a Master Carpenter, Builder, and Architect in Old Montreal
JOHN TRY A Master Carpenter, Builder, and Architect in Old Montreal CANADIAN ARCHITEC" AND BUILUER. OUl ltU\ '~1 ·: IS ST. G.\I JI-<!f:l. Sll{l'.t-:T. MON1l{I ':.\L ......____..__''"-"'......__?r-e. _/ ~..,.- ... : ... · ~- . , I I C fril .""'-"" t liunt.'~ M.. \.\oC\., U . ~ by A. J.H. Richardson and Stephen Otto 32 SSAC BULLETIN SEAC 22:2 Figure 1 (previous page). House on St Gabriel Street, Montreal, measured and drawn by Cecil Scott Burgess in 1904 and reproduced in the supplement to Csnsdisn Archit1ct snd Buildsr 18, no. 211 (July 1905). This is the house built for David Ross in 1813-.15. (Metropolitan Toronto Reference Library) Figure 2 (left). Watercolour of the interior of Christ Church Cathedral, Montreal, 1852; James Duncan (1806·1881), artist. (McCord Museum of Canadian History, M6015) ohn Try was likely born in 1779 or 1780; when he died suddenly on 14 August 1855, on holiday at Saco near Portland, Maine, he was said to be seventy-five years Jold and a native of England.1 His exact birthplace has not been identified. Nor is it known where he was trained in his trade as a carpenter, although his rapid success in Canada suggests he arrived here well qualified. Try appears to have emigrated to Montreal in 1807. Confirmation for this year is found in a statement he made in 1841: "I have resided in this City thirty-four years."2 More circumstantial evidence exists in an application that David Ross, a lawyer, made in 1814 to the Governor-in-Chief to allow either "Daniel Reynard Architect and Stucco worker," or "--Roots Plasterer and Stucco worker," both of Boston, to enter the province to work on a large house Ross was building in Montreal (figure 1) .3 Vice-regal consent was needed because a state of war still existed between Britain and the United States. -

By the Numbers Excellence, Innovation, Leadership: Research at the University of Toronto a Powerful Partnership
BY THE NUMBERS EXCELLENCE, INNOVATION, LEADERSHIP: RESEARCH AT THE UNIVERSITY OF TORONTO A POWERFUL PARTNERSHIP The combination of U of T and the 10 partner hospitals affiliated with the university creates one of the world’s largest and most innovative health research forces. More than 1,900 researchers and over 4,000 graduate students and postdoctoral fellows pursue the next vital steps in every area of health research imaginable. UNIVERSITY OF TORONTO Sunnybrook Health St. Michaelʼs Sciences Centre Hospital Womenʼs College Bloorview Kids Hospital Rehab A POWERFUL PARTNERSHIP Baycrest Mount Sinai Hospital The Hospital University Health for Sick Children Network* Centre for Toronto Addiction and Rehabilitation Mental Health Institute *Composed of Toronto General, Toronto Western and Princess Margaret Hospitals 1 UNIVERSITY OF TORONTO FACULTY EXCELLENCE U of T researchers consistently win more prestigious awards than any other Canadian university. See the end of this booklet for a detailed list of awards and honours received by our faculty in the last three years. Faculty Honours (1980-2009) University of Toronto compared to awards held at other Canadian universities International American Academy of Arts & Sciences* Gairdner International Award Guggenheim Fellows National Academies** Royal Society Fellows Sloan Research Fellows American Association for the Advancement of Science* ISI Highly-Cited Researchers*** 0 20 40 60 801 00 Percentage National Steacie Prize Molson Prize Federal Granting Councilsʼ Highest Awards**** Killam Prize Steacie -

Printable List of Laureates
Laureates of the Canadian Medical Hall of Fame A E Maude Abbott MD* (1994) Connie J. Eaves PhD (2019) Albert Aguayo MD(2011) John Evans MD* (2000) Oswald Avery MD (2004) F B Ray Farquharson MD* (1998) Elizabeth Bagshaw MD* (2007) Hon. Sylvia Fedoruk MA* (2009) Sir Frederick Banting MD* (1994) William Feindel MD PhD* (2003) Henry Barnett MD* (1995) B. Brett Finlay PhD (2018) Murray Barr MD* (1998) C. Miller Fisher MD* (1998) Charles Beer PhD* (1997) James FitzGerald MD PhD* (2004) Bernard Belleau PhD* (2000) Claude Fortier MD* (1998) Philip B. Berger MD (2018) Terry Fox* (2012) Michel G. Bergeron MD (2017) Armand Frappier MD* (2012) Alan Bernstein PhD (2015) Clarke Fraser MD PhD* (2012) Charles H. Best MD PhD* (1994) Henry Friesen MD (2001) Norman Bethune MD* (1998) John Bienenstock MD (2011) G Wilfred G. Bigelow MD* (1997) William Gallie MD* (2001) Michael Bliss PhD* (2016) Jacques Genest MD* (1994) Roberta Bondar MD PhD (1998) Gustave Gingras MD* (1998) John Bradley MD* (2001) Phil Gold MD PhD (2010) Henri Breault MD* (1997) Richard G. Goldbloom MD (2017) G. Malcolm Brown PhD* (2000) Jean Gray MD (2020) John Symonds Lyon Browne MD PhD* (1994) Wilfred Grenfell MD* (1997) Alan Burton PhD* (2010) Gordon Guyatt MD (2016) C H G. Brock Chisholm MD (2019) Vladimir Hachinski MD (2018) Harvey Max Chochnov, MD PhD (2020) Antoine Hakim MD PhD (2013) Bruce Chown MD* (1995) Justice Emmett Hall* (2017) Michel Chrétien MD (2017) Judith G. Hall MD (2015) William A. Cochrane MD* (2010) Michael R. Hayden MD PhD (2017) May Cohen MD (2016) Donald O.