Assisted Living Facilities
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hospice and Assisted Living: Improving Care at the End of Life
Hospice and Assisted Living: Improving Care at the End of Life Cherry Meier, RN, MSN eniors have embraced the concept of “aging in place.” S The challenge that inevitably occurs is the concept of “dying in place.” Seniors do not want to go through another change in living arrangements and do not want to become a burden on their families at the end of their life. Is it realistic to think that an eld- erly resident may be able to die in an assisted living (AL) residence? Depending upon what state you live in, it may or may not be possi- ble. Some states have very strict move-in and discharge require- ments that prohibit a dying resident from staying in their AL residence because they become bedbound, have a foley catheter, or require oxygen. Such requirements are usu- ally in response to concerns for life and safety in the event that a build- ing needs to be evacuated quickly or that the resident has complex 6 months or less if the illness runs equipment, and medical supplies needs that cannot be met by the AL its normal course and elects to re- related to the terminal illness. staff. Other states waive these rules ceive palliative/comfort care instead • On-call services, 24 hours a day. for residents who elect to receive of curative care. The AL residence • Bereavement care to the family/ care from hospice. is considered to be the resident’s loved ones following the death home, where the following services of the resident. The Medicare Hospice Benefit can be provided: The Medicare Hospice Benefit is • Services by an interdisciplinary The goal of care is to control the available to Medicare and Medicaid health care team comprised of resident’s pain and other uncomfort- beneficiaries in all states, except physicians, nurses, home health able symptoms through the dying Oklahoma, New Hampshire, and aides, social workers, chaplains, process. -

Caregiver, CNA, Direct Support Professional
CAREGIVER – DIRECT SUPPORT PROFESSIONAL – CNA Are you looking for a change? We are an active assisted living community located on a tranquil 50-acres ranch setting in Northern Arizona, providing a beautiful work environment where your compassion for others, talent, education, and expertise is encouraged and rewarded! We are currently welcoming detail-oriented, energetic, quick learners interested in assisting adults with autism and other neurodevelopmental disorders. If this sounds like you, we invite you to explore the advantages of joining us, including: • More Time for You! We want your time to count, too—so we provide a full time, condensed work schedule leaving you more time for family and personal interests. • We Pay for What You Know: Our caregiving team enjoys wages proportional to their career accomplishments, education, and certification. • A One-Trip Work Stop: No more travel time to work five or more times a week saves you gas money and time. • Professional Growth: We provide free training, tuition reimbursement, and certification opportunities to help you be at your best today, and in the future. • Newcomers Welcome: We embrace the opportunity to train individuals interested in a career in assisted living and healthcare that want to learn the ‘Rainbow Way.’ • To Your Good Health and Well-being: While on shift, you will enjoy meals from our kitchen and opportunities to participate in healthy choices like free massages or our annual flu clinic. Responsibilities Include: • Provision of personal care. • Providing friendly, caring companionship. • Transportation services for appointments or events. • Assisting residents to, and participating in, on-site classes. • Administering medications as prescribed. -
DON Boot Camp Full Page Book W Boots.Pub
DON Boot Camp Created specifically for Directors of Nursing in Long Term Care Skilled Nursing Facilities Presented by: November 13-16, 2018 Midwest Health Inc. Training Center—Basement Level Inside the Heritage Bank Building 3024 SW Wanamaker Rd. Topeka, KS 66614 Director of Nursing BOOT CAMP You’ve asked and KHCA/KCAL and LICA MedMan have Cancellaons and Refunds: responded! This program has been specifically Cancellaons must be received by 5:00 pm created for Nurses that are new to the Director of November 6, 2018 for an 80% refund. No Nursing Posion in the Long Term Care/Skilled refunds will be made for cancellaons aer this nursing posion or for those who want to brush up to date. Substutes are welcome. Special make sure they are up to date on the most current dispensaon will be given with proof of survey informaon. Seang is limited. Register early to in your building during the dates of the course. assure you have a seat for this first me KHCA/KCAL and LICA MedMan DON Boot Camp! Dress: Please Bring a Sweater or Jacket. Parcipants are encouraged to dress Fees and Registraon: comfortably ‐ casual are is appropriate. We Register at www.khca.org and click on educaon. recommend that parcipants dress in layers, as Please call KHCA/KCAL at 785‐267‐6003 with quesons room temperatures at facilies vary. Provided regarding this class. nametag should be worn for the enre course. KHCA/KCAL and LicaMedman will make Early Bird Registraon available unl reasonable efforts to make our events accessible October 26, 2018: to persons with disabilies. -

Choices for Living 2013 - 2014
Choices for Living MARIN COUNTY 2013-2014 AGING & ADULT SERVICES 9 Independent Living Options 18 Care Home Evaluation Checklist 28 Skilled Nursing Facilities Evaluation Checklist 29 Skilled Nursing Facilities 30 Useful Websites & Resources C hoices for Living (Choices) is a resource to help families and older adults explore the many housing options available in Marin County. Individuals’ housing needs vary greatly, and needs may change over time. The process of exploring housing options can be very confusing. We urge anyone considering a housing change to be as clear as possible about the lifestyle and location they seek, their current health and level of independence, and the financial means by which they will support their housing needs. Choices begins with information on housing assistance and independent living options, and progresses to assisted living, board and care facilities and skilled nursing facilities. Often, waiting lists are encountered when obtaining housing in Marin County; we urge you to place your name on these lists if applications are being accepted. The information provided in this resource guide may not be current after July 2013. Listings are provided for information only and are not meant to endorse any particular agency or service. 1 Choices for Living 2013 - 2014 Getting Connected to Services is as Easy as 1-2-3 STEP 1. Call (415) 457-INFO (457-4636) STEP 2. Pick a language STEP 3. Pick a program or choose the “General Information and Assistance” option to speak to staff The Network of Care for Older Adults & Individuals is provided by the Marin County Aging and Adult Services. -

Residential Care/Assisted Living Compendium: Pennsylvania
Compendium of Residential Care and Assisted Living Regulations and Policy: 2015 Edition PENNSYLVANIA Licensure Terms Assisted Living Residence, Personal Care Home General Approach Assisted living residences (ALRs) are licensed by the Department of Aging, Office of Long Term Living, Division of Licensing, and personal care homes are licensed by the Department of Public Welfare, Adult Residential Licensing. The two licensure types differ in concept, the type of units provided, and the level of care provided. Personal care homes may not serve individuals who need a nursing home level of care but ALRs can serve such individuals. ALRs must support aging in place, are constructed with private living units that include kitchen capacity, and provide a level of care higher than personal care homes. A personal care home and ALR may be co-located within a building under a dual license. This profile includes the regulations for both types, as well as the provisions for special care units (SCUs) for residents with Alzheimer’s disease or other dementias for the two types. Adult Foster Care. The state licenses domiciliary care for up to three residents, which provides a supervised living arrangement in a home-like setting to adult clients placed there by Area Agencies on Aging (AAAs). The AAAs screen providers to ensure that both they and their homes pass safety and background checks. The majority of providers serve only one resident. Regulatory provisions for domiciliary care are not included in this profile but a link to the provisions can found at the end. This profile includes summaries of selected regulatory provisions for ALRs and personal care homes. -

Assisted Living Policy and Procedure
Assisted Living Policy and Procedure Subject/Title: Motorized Mobility Aids: Wheelchairs, Carts, and Scooters Pendulum, 4600B Montgomery Blvd. NE, Suite 204, Albuquerque, NM 87109 Reference: (888) 815-8250 • www.WeArePendulum.com I. POLICY GUIDELINES The facility promotes that residents with disabilities and physical limitations have access to devices that improve their independence. Motorized mobility aids may improve access to the facility and services. In order to provide a safe environment for residents, employees, and visitors, the facility maintains a policy for use of motorized mobility aids, whether they are wheelchairs, carts, or scooters. Orientation for safe use of motorized mobility aids augments safety for the resident using these devices as well as other residents, visitors, and employees. Routine inspection of motorized mobility aids promotes the maintenance of equipment that remains in good working order. II. DEFINITION A motorized mobility aid or device is a wheelchair, cart, or scooter that serves as an assistive device to allow an individual to be more independent and/or enables an individual to accomplish a task. In accordance with the Americans with Disabilities Act, Title II, Part 35, Nondiscrimination on the Basis of Disability in State and Local Government Services, Use of other power-driven mobility devices: A public entity shall make reasonable modifications in its policies, practices, or procedures to permit the use of other power-driven mobility devices by individuals with mobility disabilities, unless the public entity can demonstrate that the class of other power-driven mobility devices cannot be operated in accordance with legitimate safety requirements that the public entity has adopted pursuant to § 35.130(h). -

Assisted Living
Coverage and Reimbursement Policy Assisted Living Policy Overview This policy documents Neighborhood Health Plan of Rhode Island’s (Neighborhood’s) coverage and reimbursement requirements for Assisted Living services provided by participating and non- participating providers. These services maximize continued independence for members that live in a residential community care facility by providing supervision, security, and safety through personalized assistance with activities of daily living. Scope This policy applies to Neighborhood’s UNITY and INTEGRITY lines of business, for services provided within scope of licensure pursuant to R.I.G.L. §23-17.4.i Coverage Neighborhood’s benefit includes the following levels of care: Base Level assisted living; Enhanced level, non-skilled assisted living; Enhanced level , skilled assisted living; Dementia care assisted living. Activities of Daily Living (ADLs) are defined as: Bathing: Direct care or constant supervision and cueing during the entire activity of a shower, bath, or sponge bath for the purpose of maintaining adequate hygiene. Dressing: Direct care of constant supervision and cueing during the entire activity of dressing and undressing, and taking prostheses, braces, anti-embolism garments, or assisted devices on or off. Eating: Direct care or constant supervision and cueing, or physical assistance provided by staff for a portion of or entirety of meals to consume food or drink through the mouth using routine or adapted utensils, inclusive of the ability to cut, chew, and swallow food. Personal Hygiene/Grooming: Direct care or constant supervision and cueing during the entirety of combing hair, brushing teeth, shave, application of make-up, nail care, eyeglasses, and jewelry application. -
2020 Rate Sheet the Basics
Wesley Meadows Retirement Community 2020 RATE SHEET THE BASICS: Care & Housing Location Year Founded Independent & assisted Hernando, MS Non-profit Organization living apartments (1325 McIngvale Road) founding in 1996 CONTACT: Marsha Brasher, Executive Director or Jamie Cliett, Community Director of Marketing and Public Relations at (662)429-2070 or [email protected] or [email protected] ABOUT US: Set in the middle of a sprawling meadow backed by woods, Wesley Meadows is a beautiful campus offering both independent living and assisted living options to older adults. Featuring a flowered courtyard and a large porch with rockers for the residents to relax on, esleyW Meadows offers a welcome change of pace. At Wesley Meadows when a resident reaches the stage of life that requires additional help, we can offer individualized assisted living services in all apartments located on our campus, allowing them to stay in their home and be independent as long as possible. CARE & HOUSING: SERVICES FOR ALL RESIDENTS: INDEPENDENT LIVING APARTMENTS • Services • Unfurnished 1 and 2 bedroom apartments with private ~ 24 hour emergency response entrances system • Free laundry facilities ~ Basic utilities including • Emergency call system cable, lights and water in all apartments ~ Maintenance staff available • Noon meal 6 days a week ~ Pets are welcomed (In accordance with established policies. Market Rent: 1 fur bearing 30 lbs. or less.) 1 Bedroom (529 sq ft) $1,854 per month* • Activities ~ Worship services and Bible 2 Bedroom (729 sq ft) $2,360 per month* studies ~ Scheduled outings 2 Bedroom with Split Bathroom $2,476 per month* (736 sq ft) • Other Services ~ Barber & Beauty Salon Double Occupancy $321 add. -

SONAR: Proposed Rules Governing Assisted Living Licensure
STATEMENT OF NEED AND REASONABLENESS FOR ASSISTED LIVING LICENSURE Proposed Rules Governing Assisted Living Licensure and Consumer Protections for Assisted Living Residents Minnesota Rules, Chapter 4659 Revisor’s ID Number 4605 OAH Docket Number 65-9000-3715 December 2020 Minnesota Department of Health Health Regulation Division PO Box 64900 St. Paul, MN 55164-0900 651-539-3049 or 844-926-1061 [email protected] www.health.state.mn.us/assistedliving To obtain this information in a different format, call: 651-539-3049 or 1-844-926-1061. TABLE OF CONTENTS STATUTORY AUTHORITY ........................................................................................................................ 3 ADVISORY COMMITTEE .......................................................................................................................... 3 INTRODUCTION ...................................................................................................................................... 4 REGULARTORY ANALYSIS ....................................................................................................................... 8 PERFORMANCE BASED RULES .............................................................................................................. 19 ADDITIONAL SONAR REQUIREMENTS .................................................................................................. 20 ADDITIONAL NOTICE PLAN ................................................................................................................. -

RN Delegation 2018
8/13/2018 MEDICATION ASSISTANCE, ADMINISTRATION AND RN DELEGATION Texas Assisted Living Association April, 2015 Objectives • Understand the BON rule for RN delegation in AL— rule 225. • State the requirements for RN delegation, including assessment, training, documentation, and supervision. • Understand the AL regulations for medication assistance, supervision, and administration in AL. • Understand the process for delegation of medication administration in assisted living. The essence of delegation... “But in both (hospitals and private houses), let whoever is in charge keep this simple question in her head, (not, how can I always do this right thing myself, but) how can I provide for this right thing to be always done? Florence Nightingale 1 8/13/2018 Definitions • Client—term to indicate who will receive care—our resident • Client’s Responsible Adult—CRA, an individual chosen by the client who is willing and able to participate in decisions about the overall management of the client’s healthcare • Unlicensed Assistive Personnel—UAP, an individual not licensed as a healthcare provider Rule 225.4 • Delegation—a registered nurse authorizes an unlicensed person to perform tasks of nursing care in selected situations and indicates that authorization in writing. • Delegation is a process that includes the nursing assessment of a client in a specific situation, evaluation of the ability of the unlicensed persons, teaching the task, ensuring supervision of the unlicensed persons and re-evaluating the task at regular intervals. Rule 225.4 (6) • Supervision—a process of directing, guiding, and influencing the outcome of an individual’s performance of an activity. • Assign—describes the distribution of work that each staff member is responsible for during a given shift or work period. -
Wheelchair Self-Release Seatbelt Rules
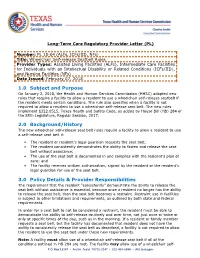
Long-Term Care Regulatory Provider Letter (PL) Number: PL 18-04 (ALFs, ICFs/IID, NFs) Title: Wheelchair Self-release Seatbelt Rules Provider Types: Assisted Living Facilities (ALFs), Intermediate Care Facilities for Individuals with an Intellectual Disability or Related Conditions (ICFs/IID), and Nursing Facilities (NFs) Date Issued: February 07, 2018 1.0 Subject and Purpose On January 2, 2018, the Health and Human Services Commission (HHSC) adopted new rules that require a facility to allow a resident to use a wheelchair self-release seatbelt if the resident meets certain conditions. The rule also specifies when a facility is not required to allow a resident to use a wheelchair self-release seat belt. The new rules implement §322.0515, Texas Health and Safety Code, as added by House Bill (HB) 284 of the 85th Legislature, Regular Session, 2017. 2.0 Background/History The new wheelchair self-release seat belt rules require a facility to allow a resident to use a self-release seat belt if: • The resident or resident’s legal guardian requests the seat belt; • The resident consistently demonstrates the ability to fasten and release the seat belt without assistance; • The use of the seat belt is documented in and complies with the resident’s plan of care; and • The facility receives written authorization, signed by the resident or the resident’s legal guardian for use of the seat belt. 3.0 Policy Details & Provider Responsibilities The requirement that the resident “consistently” demonstrate the ability to release the seat belt without assistance is essential, because once a resident no longer has the ability to release the seat belt, then the seat belt becomes a restraint. -
Long-Term Care for the Elderly with Disabilities: Current Policy, Emerging Trends, and Implications for the Twenty-First Century
Long-Term Care for the Elderly with Disabilities: Current Policy, Emerging Trends, and Implications for the Twenty-First Century By Robyn I. Stone Long-Term Care for the Elderly with Disabilities: Current Policy, Emerging Trends, and Implications for the Twenty-First Century By Robyn I. Stone Milbank Memorial Fund TABLE OF CONTENTS Foreword . iv Acknowledgments . v Introduction . 1 Defining Long-Term Health Care . 2 Relationship between Acute and Long-Term Care . 2 The Role of Residence in Long-Term Care . 3 Care Settings . 4 Who Needs and Uses Long-Term Care? . 5 Who Provides Care? . 9 Informal Care . 9 Formal Care Providers . 10 Long-Term Care Financing . 13 Medicaid . 13 Medicare . 14 Private Long-Term Care Insurance . 17 Long-Term Care Delivery . 21 Integration of Acute and Long-Term Care Services . 21 Federal Demonstrations . 22 State Initiatives . 23 Provider Initiatives . 24 Assisted Living . 25 Consumer-Directed Care . 28 Workforce Preparation . 31 The Future of Long-Term Care Demand . 34 The Aging Population . 34 Increased Longevity: Quantity vs. Quality . .35 Geographic Diversity . 36 The Future of Informal Caregiving . 40 The Economic Status of the Future Elderly . 42 The Future Supply of Long-Term Care Services . .47 The Future Supply of Alternative Settings . 47 The Future of the Long-Term Care Workforce . 48 (Continued) Sinking or Swimming into the Future? . 50 Implications for Long-Term Care Financing . 50 Implications for Service Delivery . 54 Impact on Workforce Development and Training . .57 Conclusion . 60 References . 61 The Author . 72 FOREWORD This report arrays evidence and analysis to assist decision makers in the private and public sectors to address three important and perplexing questions about long-term care for the increasing number of Americans who are elderly and frail.