Bowel Problems What to Do If Things Go Wrong
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Anatomy of the Rectum and Anal Canal
BASIC SCIENCE identify the rectosigmoid junction with confidence at operation. The anatomy of the rectum The rectosigmoid junction usually lies approximately 6 cm below the level of the sacral promontory. Approached from the distal and anal canal end, however, as when performing a rigid or flexible sigmoid- oscopy, the rectosigmoid junction is seen to be 14e18 cm from Vishy Mahadevan the anal verge, and 18 cm is usually taken as the measurement for audit purposes. The rectum in the adult measures 10e14 cm in length. Abstract Diseases of the rectum and anal canal, both benign and malignant, Relationship of the peritoneum to the rectum account for a very large part of colorectal surgical practice in the UK. Unlike the transverse colon and sigmoid colon, the rectum lacks This article emphasizes the surgically-relevant aspects of the anatomy a mesentery (Figure 1). The posterior aspect of the rectum is thus of the rectum and anal canal. entirely free of a peritoneal covering. In this respect the rectum resembles the ascending and descending segments of the colon, Keywords Anal cushions; inferior hypogastric plexus; internal and and all of these segments may be therefore be spoken of as external anal sphincters; lymphatic drainage of rectum and anal canal; retroperitoneal. The precise relationship of the peritoneum to the mesorectum; perineum; rectal blood supply rectum is as follows: the upper third of the rectum is covered by peritoneum on its anterior and lateral surfaces; the middle third of the rectum is covered by peritoneum only on its anterior 1 The rectum is the direct continuation of the sigmoid colon and surface while the lower third of the rectum is below the level of commences in front of the body of the third sacral vertebra. -

2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome
MEDICAL POLICY – 2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome BCBSA Ref. Policy: 2.04.26 Effective Date: July 1, 2021 RELATED MEDICAL POLICIES: Last Revised: June 8, 2021 None Replaces: N/A Select a hyperlink below to be directed to that section. POLICY CRITERIA | DOCUMENTATION REQUIREMENTS | CODING RELATED INFORMATION | EVIDENCE REVIEW | REFERENCES | HISTORY ∞ Clicking this icon returns you to the hyperlinks menu above. Introduction Intestinal dysbiosis is a condition that occurs when the microorganisms in the digestive tract are out of balance. This condition is believed to cause diseases of the digestive tract, including poor nutrient absorption, overgrowth of certain bacteria, and irritable bowel syndrome (IBS). Symptoms of these digestive problems are similar and may include: abdominal pain, excess gas, bloating, and changes in bowel movements (constipation or diarrhea, or both). One method of diagnosing digestive disorders is by testing a fecal sample. Using fecal analysis to diagnose intestinal dysbiosis, IBS, malabsorption, or small intestinal overgrowth of bacteria is unproven (investigational). More studies are needed to see if this testing improves health outcomes. Note: The Introduction section is for your general knowledge and is not to be taken as policy coverage criteria. The rest of the policy uses specific words and concepts familiar to medical professionals. It is intended for providers. A provider can be a person, such as a doctor, nurse, psychologist, or dentist. A provider also can be a place where medical care is given, like a hospital, clinic, or lab. This policy informs them about when a service may be covered. -

Mouth Esophagus Stomach Rectum and Anus Large Intestine Small
1 Liver The liver produces bile, which aids in digestion of fats through a dissolving process known as emulsification. In this process, bile secreted into the small intestine 4 combines with large drops of liquid fat to form Healthy tiny molecular-sized spheres. Within these spheres (micelles), pancreatic enzymes can break down fat (triglycerides) into free fatty acids. Pancreas Digestion The pancreas not only regulates blood glucose 2 levels through production of insulin, but it also manufactures enzymes necessary to break complex The digestive system consists of a long tube (alimen- 5 carbohydrates down into simple sugars (sucrases), tary canal) that varies in shape and purpose as it winds proteins into individual amino acids (proteases), and its way through the body from the mouth to the anus fats into free fatty acids (lipase). These enzymes are (see diagram). The size and shape of the digestive tract secreted into the small intestine. varies in each individual (e.g., age, size, gender, and disease state). The upper part of the GI tract includes the mouth, throat (pharynx), esophagus, and stomach. The lower Gallbladder part includes the small intestine, large intestine, The gallbladder stores bile produced in the liver appendix, and rectum. While not part of the alimentary 6 and releases it into the duodenum in varying canal, the liver, pancreas, and gallbladder are all organs concentrations. that are vital to healthy digestion. 3 Small Intestine Mouth Within the small intestine, millions of tiny finger-like When food enters the mouth, chewing breaks it 4 protrusions called villi, which are covered in hair-like down and mixes it with saliva, thus beginning the first 5 protrusions called microvilli, aid in absorption of of many steps in the digestive process. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

An Osteopathic Approach to Reduction of Readmissions for Neonatal Jaundice
Osteopathic Family Physician (2013) 5, 17–23 REVIEW ARTICLE An osteopathic approach to reduction of readmissions for neonatal jaundice Rachel Click, DO,a Julie Dahl-Smith, DO,a Lindsay Fowler, DO,a Jacqueline DuBose, MD,a Margi Deneau-Saxton, RN, CCCE, CIMI, CLC, CPD,b Jennifer Herbert, MDc From aGeorgia Health Sciences University, Medical College of Georgia, Department of Family Medicine, GA; bGeorgia Health System, OB Labor and Delivery, GA; and cUniversity Primary Care, Evans, GA. KEYWORDS: Jaundice is a potentially life-threatening condition that continues to affect at-risk newborns, accounting Breastfeeding; for continued hospital readmissions. As family physicians, we should be cognizant of neonates who may Jaundice; be at risk for jaundice, including those with pathologic jaundice as well as newborns of breastfeeding Prevention; mothers, and ensure sufficient intervention is taken to help prevent further elevations in bilirubin levels. Hyperbilirubinemia; Interventions are likely to include evaluation for sepsis, education regarding feeding frequencies for both Neonatal massage breast- and bottle-fed neonates, reviewing maternal and hematologic risk factors for neonatal jaundice, and considering inborn errors of metabolism. An additional measure family physicians may consider is that of neonatal massage for those with elevated bilirubin levels. Neonatal massage, though not widely used, has been proven to promote excess bilirubin excretion, thus decreasing length of hospital stay; all the while, providing an intervention that allows parents to take an active role. r 2013 Elsevier Inc. All rights reserved. Introduction morbidity rate with bilirubin 4 20 mg/dL. “It has been estimated that the risk of kernicterus in infants with total Jaundice is a product of excess bilirubin (a product of serum bilirubin (TSB) greater than 30 mg/dL is about 1 in broken down red blood cells), which manifests as a 7 infants”.1 Less serious complications of hyperbilirubine- yellowing of the skin and eyes. -

INFORMED CARING JAUNDICE Neonatal Jaundice BILIARY
1 INFORMED CARING Situations with Adults and Children with Gallbladder, Liver and Pancreatic Disorders 2 JAUNDICE ä Does NOT mean hepatitis ä Increased breakdown of RBCs ä Altered bilirubin breakdown ä Impeded flow through liver or bile duct ä First seen in sclera, then skin 3 Neonatal Jaundice ä Not liver failure ä RBC breakdown ä Phototherapy 4 BILIARY ATRESIA ä Jaundice 2-3 weeks after birth ä Easy bruising ä Stools putty like ä Tea colored urine ä Abdominal/organ distension 5 4 F’s of Gallbladder ä Fair ä Fat X size of person X amount in diet ä Fertile X BCP X Multiparity ä Forty 6 Cholelithiasis ä Calculi within the duct or gallbladder ä Severe colicky, cramp-like pain X radiates to shoulder blade X Murphy's sign ä Cholecystitis: inflammation X Can be caused by trauma, fasting, TPN or abdominal surgery 7 Diagnostic Studies ä Ultrasound of abdomen 1 X not for the obese ä HIDA scan X nuclear medicine ä Cholangiograms X endoscopic X transvenous X intraoperative 8 Post-op Care ä High abdominal incision X respiratory compromise ä T-tube X patients need to know how to empty it X may clamp it prior to removal X caution not dislodged with movements ä NO Morphine X spasms of sphincter of Oddi 9 Post-op Nutrition ä Limited fat in diet X can have rapid transit times ä Potential fat soluble vitamin deficit X A, D, E and K ä Weight loss diet 10 LIVER FAILURE ä Cirrhosis ä Drug toxicity X acetaminophen, anesthetics, HCTZ, chemotherapy ä Infection ä Cancer ä ETOH is single most linked cause 11 LIVER FAILURE S/S ä Don’t show up until 80-90% failed -

Transposition of the Anus
TRANSPOSITION OF THE ANUS Report of a Case WM. E. LOWER, M.D. The case which is herewith reported was that of a girl, aged 4 who was first seen in September, 1939 with a chief complaint of con- genital absence of the rectal opening in the perineum; however, she had an opening into the vagina (Fig. 1) which in appearance was not unlike a normal anus. The only repair had been a slight enlargement of the opening into the vagina to permit freer bowel movements. The patient had an almost constant fecal drainage unless she was constipated; then she had formed stools. There was no history of blad- der difficulty nor nocturia, although there had been some frequency; 16 Downloaded from www.ccjm.org on September 30, 2021. For personal use only. All other uses require permission. TRANSPOSITION OF THE ANUS and the child had good bladder control. Some voluntary control oi bowel movements also had been observed. In June, 1941 the patient was admitted to the Cleveland Clinic Hospital for operation. Under general anesthesia a loop sigmoid FIGURE 2. Separation of the opening in the vagina and the perineal incision. colostomy was performed, after which the lower bowel was thoroughly cleansed. When the colostomy was functioning well, an opening was made in the perineum, and the opening in the vagina dissected free 17 Downloaded from www.ccjm.org on September 30, 2021. For personal use only. All other uses require permission. WM. E. LOWER FIGURE 3. Freeing the opening into the vagina. (Figs. 2 and 3). With a long forceps this part of the gut was transposed to the new opening in the perineum (Fig. -

Symptomatic Approach to Gas, Belching and Bloating 21
20 Osteopathic Family Physician (2019) 20 - 25 Osteopathic Family Physician | Volume 11, No. 2 | March/April, 2019 Gennaro, Larsen Symptomatic Approach to Gas, Belching and Bloating 21 Review ARTICLE to escape. This mechanism prevents the stomach from becoming IRRITABLE BOWEL SYNDROME (IBS) Symptomatic Approach to Gas, Belching and Bloating damaged by excessive dilation.2 IBS is abdominal pain or discomfort associated with altered with OMT Treatment Options Many patients with GERD report increased belching. Transient bowel habits. It is the most commonly diagnosed GI disorder lower esophageal sphincter (LES) relaxation is the major and accounts for about 30% of all GI referrals.7 Criteria for IBS is recurrent abdominal pain at least one day per week in the Carly Gennaro, DO1; Helaine Larsen, DO1 mechanism for both belching and GERD. Recent studies have shown that the number of belches is related to the number of last three months associated with at least two of the following: times someone swallows air. These studies have concluded that 1) association with defecation, 2) change in stool frequency, 1 Good Samaritan Hospital Medical Center, West Islip, NY patients with GERD swallow more air in response to heartburn and 3) change in stool form. Diagnosis should be made using these therefore belch more frequently.3 There is no specific treatment clinical criteria and limited testing. Common symptoms are for belching in GERD patients, so for now, physicians continue to abdominal pain, bloating, alternating diarrhea and constipation, treat GERD with proton pump inhibitors (PPIs) and histamine-2 and pain relief after defecation. Pain can be present anywhere receptor antagonists with the goal of suppressing heartburn and in the abdomen, but the lower abdomen is the most common KEYWORDS: ABSTRACT: Intestinal gas production is a normal physiologic progress. -
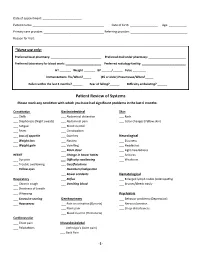
Patient Review of Systems Please Mark Any Condition with Which You Have Had Significant Problems in the Last 6 Months
Date of appointment: ________________________ Patient name: ____________________________________________ Date of birth: _________________ Age: ___________ Primary care provider: _____________________________________ Referring provider: ___________________________________ Reason for Visit: _____________________________________________________________________________________________ *Nurse use only: Preferred local pharmacy: _______________________________ Preferred mail order pharmacy: _______________________ Preferred laboratory for blood work: ______________________ Preferred radiology facility: ___________________________ HT _______ Weight _______ BP ______/______ Pulse ________ Immunizations: Flu/When?_____ (65 or older) Pneumovax/When?_____ Fallen within the last 3 months? ______ Fear of falling?______ Difficulty ambulating? ______ Patient Review of Systems Please mark any condition with which you have had significant problems in the last 6 months: Constitution Gastrointestinal Skin ___ Chills ___ Abdominal distention ___ Rash ___ Diaphoresis (Night sweats) ___ Abdominal pain ___ Color changes (Yellow skin) ___ Fatigue ___ Blood in stool ___ Fever ___ Constipation ___ Loss of appetite ___ Diarrhea Neurological ___ Weight loss ___ Nausea ___ Dizziness ___ Weight gain ___ Vomiting ___ Headaches ___ Black stool ___ Light-headedness HEENT ___ Change in bowel habits ___ Seizures ___ Eye pain ___ Difficulty swallowing ___ Weakness ___ Trouble swallowing ___ Gas/flatulence ___ Yellow eyes ___ Heartburn/indigestion ___ Bowel accidents Hematological -

A Case of Solitary Rectal Diverticulum Presenting with a Large Retrorectal Abscess T
Annals of Medicine and Surgery 49 (2020) 57–60 Contents lists available at ScienceDirect Annals of Medicine and Surgery journal homepage: www.elsevier.com/locate/amsu Case report A case of solitary rectal diverticulum presenting with a large retrorectal abscess T ∗ Stefanos Gorgoraptisa,Sofia Xenakia, ,1, Elias Athanasakisa, Anna Daskalakia, Konstantinos Lasithiotakisa, Evangelia Chrysoub, Emmanuel Chrysosa a Department of General Surgery, University Hospital of Heraklion Crete, Greece b Department of Radiology, University Hospital of Heraklion Crete, Greece ARTICLE INFO ABSTRACT Keywords: Colonic diverticular disease is a common condition, affecting 50% of the population aged above 80. In contrast, Rectal diverticulum rectal diverticular disease is a rare condition with very few cases reported, while symptomatic rectal diverticular Abscess disease is even rarer. We present a case of a symptomatic large rectal diverticulum presenting with a retrorectal Diverticulitis abscess. A 49-year-old Caucasian female was brought to the emergency department complaining of abdominal Complications pain and weakness in the lower limbs. She was found to have obstructive uropathy and unilateral sciatic neu- ropathy. She rapidly developed acute abdomen and emergency laparotomy revealed a giant purulent rectal diverticulum. The patient underwent exploratory laparotomy and a loop colostomy was made to decompress the colon. 1. Introduction Neurologic examination revealed asymmetric paraparesis and hy- poesthesia in the lower limbs, affecting hip extension, knee flexion, Despite the high incidence of colonic diverticular disease, the oc- ankle dorsiflexion, plantarflexion, eversion and big toe extension, with currence of rectal diverticula is extremely unusual, with only few, brisk tendon reflexes in the knees but absent in the ankle, in keeping sporadic published reports since 1911 [11]. -

Ulcerative Proctitis, Rectal Prolapse, and Intestinal Pseudo-Obstruction
0023-6837/01/8103-297$03.00/0 LABORATORY INVESTIGATION Vol. 81, No. 3, p. 297, 2001 Copyright © 2001 by The United States and Canadian Academy of Pathology, Inc. Printed in U.S.A. Ulcerative Proctitis, Rectal Prolapse, and Intestinal Pseudo-Obstruction in Transgenic Mice Overexpressing Hepatocyte Growth Factor/Scatter Factor Hisashi Takayama, Hitoshi Takagi, William J. LaRochelle, Raj P. Kapur, and Glenn Merlino First Department of Internal Medicine (HT, HT), Gunma University School of Medicine, Maebashi, Gunma, Japan; Laboratory of Molecular Biology (GM) and Laboratory of Cellular and Molecular Biology (WJL), National Cancer Institute, Bethesda, Maryland; and Department of Pathology (RPK), University of Washington Medical Center, Seattle, Washington SUMMARY: Hepatocyte growth factor/scatter factor (HGF/SF) can stimulate growth of gastrointestinal epithelial cells in vitro; however, the physiological role of HGF/SF in the digestive tract is poorly understood. To elucidate this in vivo function, mice were analyzed in which an HGF/SF transgene was overexpressed throughout the digestive tract. Nearly a third of all HGF/SF transgenic mice in this study (28 of 87) died by 6 months of age as a result of sporadic intestinal obstruction of unknown etiology. Enteric ganglia were not overtly affected, indicating that the pathogenesis of this intestinal lesion was different from that operating in Hirschsprung’s disease. Transgenic mice also exhibited a rectal inflammatory bowel disease (IBD) with a high incidence of anorectal prolapse. Expression of interleukin-2 was decreased in the transgenic colon, indicating that HGF/SF may influence regulation of the local intestinal immune system within the colon. These results suggest that HGF/SF plays an important role in the development of gastrointestinal paresis and chronic intestinal inflammation. -

Management of Rectal Prolapse –The State of the Art
Central JSM General Surgery: Cases and Images Bringing Excellence in Open Access Review Article *Corresponding author Adrian E. Ortega, Division of Colorectal Surgery, Keck School of Medicine at the University of Southern California, Los Angeles Clinic Tower, Room 6A231-A, Management of Rectal Prolapse LAC+USC Medical Center, 1200 N. State Street, Los Angeles, CA 90033, USA, Email: sccowboy78@gmail. – The State of the Art com Submitted: 22 November 2016 Ortega AE*, Cologne KG, and Lee SW Accepted: 20 December 2016 Division of Colorectal Surgery, Keck School of Medicine at the University of Southern Published: 04 January 2017 California, USA Copyright © 2017 Ortega et al. Abstract OPEN ACCESS This manuscript reviews the current understanding of the condition known as rectal prolapse. It highlights the underlying patho physiology, anatomic pathology Keywords and clinical evaluation. Past and present treatment options are discussed including • Rectal prolapsed important surgical anatomic concepts. Complications and outcomes are addressed. • Incarcerated rectal prolapse INTRODUCTION Rectal prolapse has existed in the human experience since the time of antiquities. References to falling down of the rectum are known to appear in the Ebers Papyrus as early as 1500 B.C., as well as in the Bible and in the writings of Hippocrates (Figure 1) [1]. Etiology • The precise causation of rectal prolapse is ill defined. Clearly, five anatomic pathologic elements may be observed in association with this condition:Diastasis of Figure 1 surrounded by circular folds of rectal mucosa. the levator ani A classic full-thickness rectal prolapse with the central “rosette” • A deep cul-de-sac • Ano-recto-colonic redundancy • A patulous anus • Loss of fixation of the rectum to its sacral attachments.