Written Responses to the South Wales Programme Engagement
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

City and County of Swansea Scrutiny Programme
CITY AND COUNTY OF SWANSEA NOTICE OF MEETING You are invited to attend a Meeting of the SCRUTINY PROGRAMME COMMITTEE At: Committee Room 2, Civic Centre, Swansea On: Monday, 11 March, 2013 Time: 4.30 pm AGENDA Page No. 1. Apologies for Absence. 2. To receive Disclosures of Personal and Prejudicial Interests. 1 3. To approve the Minutes of the Scrutiny Programme Committee 2 - 11 held on 11 February 2013. 4. Crime & Disorder Scrutiny: Performance of Safer Swansea 12 - 69 Partnership - Presentation followed by Questions to Co-Chairs of the Partnership: • Chief Superintendent Julian Williams (South Wales Police) • Reena Owen (Corporate Director – Environment) 5. Follow Up on Previous Scrutiny Reports: 70 - 82 a) Swansea City Centre (first follow up) (Joint Report of the Cabinet Members for Place and Regeneration) 6. Single Integrated Plan Consultation: a) Report Back from Councillor Consultation Seminar on Swansea's New 83 - 94 Single Integrated Plan. b) Scrutiny Arrangements for Swansea Local Service Board. 95 - 98 7. Annual Self Evaluation - Education Services to Children and 99 - 187 Young People 2012-2013. 8. Scrutiny Work Programme: 188 - 201 a) The Committee Work Plan. b) Progress on Informal Scrutiny Panels and Working Groups. 9. Scrutiny Letters: a) Letter to / from Cabinet Member for Well Being re. Child & Family 202 - 208 Services Performance Panel. b) Letter to / from Cabinet Member for Place re. Local Flood Risk 209 - 215 Management Scrutiny Working Group. 10. Date and Time of Future Meetings for 2012/13 Municipal Year (all on Mondays at 4.30 p.m.) - 8 April 2013. Patrick Arran Head of Legal, Democratic Services & Procurement Monday, 4 March 2013 Contact: Samantha Woon - Tel: (01792) 637292 Agenda Item 2 Disclosures of Personal Interest from Members To receive Disclosures of Personal Interest from Members in accordance with the provisions of the Code of Conduct adopted by the City and County of Swansea. -

Of 5 VALID PLANNING APPLICATIONS
Tredomen House Tŷ Tredomen Tredomen Park Parc Tredomen Tredomen Tredomen Ystrad Mynach Ystrad Mynach Hengoed Hengoed CF82 7WF CF82 7WF VALID PLANNING APPLICATIONS RECEIVED UP TO 15 January 2020 Any comments or enquiries should be addressed to the Development Management Manager Case Ref. 19/0927/FULL Site Area: 224m² Location: 28 Tawelfan Nelson Treharris CF46 6EH (UPRN 000043008282) Proposal: Erect two storey side extension Case Officer: Mr J Cooke 01443 864347 [email protected] Ward: Nelson Map 311109 (E) 196028 (N) Ref : Community Council : Nelson Community Council Expected Delegated Decision Level: Case Ref. 19/0944/FULL Site Area: 215m² Location: 10 Maes Y Pandy Bedwas Caerphilly CF83 8HQ (UPRN 000043077263) Proposal: Replace existing garage door with window and extend on top of existing garage with additional parking and rear conservatory Case Officer: Mr A Pyne 01443 864523 [email protected] Ward: Bedwas, Map 316243 (E) 189222 (N) Trethomas & Ref : Machen Community Council : Bedwas Trethomas & Machen Comm. Expected Delegated Council Decision Level: Page 1 of 5 Case Ref. 20/0002/FULL Site Area: 213m² Location: 18 Gwyn Drive Caerphilly CF83 3FR (UPRN 000043026802) Proposal: Extend and convert existing garage to sitting room. Associated works to create new retained parking areas, a step access and patio Case Officer: Mr A Pyne 01443 864523 [email protected] Ward: Morgan Jones Map 315083 (E) 187741 (N) Ref : Community Council : Caerphilly Town Council Expected Delegated Decision Level: Case Ref. 20/0007/FULL Site Area: 307m² Location: 7 Clos Dwyerw Caerphilly CF83 1TE (UPRN 000043014039) Proposal: Raise ridge height and erect rear dormer roof extension Case Officer: Mr J Cooke 01443 864347 [email protected] Ward: St Martins Map 314512 (E) 186327 (N) Ref : Community Council : Caerphilly Town Council Expected Delegated Decision Level: Case Ref. -

The Glamorgan-Gwent Archaeological Trust Half
THE GLAMORGAN-GWENT ARCHAEOLOGICAL TRUST High Street Presumed layout of burgage plots Outer Ditch High Street Excavated section of outer Bailey ditch Presumed line of medieval town wall Ditch awe Goat Street Goat Medieval course Old of River Tawe Castle River T New Castle Cross Street Wind Street St Mary's Church 14th century St David's hospital preserved as part of Fisher Street the Cross Keys public house Areas of 13th and 14th Century pits Line of medieval boundary ditch GRID for Swansea's N 0 100metres lower suburb HALF-YEARLY REVIEW 2010 & ANNUAL REVIEW OF PROJECTS 2009-2010 STE GI RE E D The Glamorgan-Gwent Archaeological Trust Ltd R O I A R N Heathfield House Heathfield Swansea SA1 6EL G IO A N ISAT Cover images from top: The ‘wandering wall’ on Cefn Car. Part of a stone inscription, probably a tombstone, referring to an ‘unjust fate’. It was found in the debris of the tower building shown below it. Aerial close-up of the herring-bone stone foundations of the tower building discovered during the building of a new coach park near Celtic Manor. Plan showing the ‘old’ and ‘new’ Swansea Castle and the probable medieval town layout. The reverse (tail side) of an extremely rare Henry 1 silver penny, struck in Pembroke probably between 1115 and 1120. This is the earliest coin yet found in Swansea. A 19th century worker’s house in a small settlement of at least five houses and a barn at Ffos-y-fran near Merthyr Tydfil. The settlement is thought to date back to the mid- 18th century when the Dowlais Ironworks was established. -

Managing Online Communications and Feedback Relating to the Welsh Visitor Attraction Experience: Apathy and Inflexibility in Tourism Marketing Practice?
Managing online communications and feedback relating to the Welsh visitor attraction experience: apathy and inflexibility in tourism marketing practice? David Huw Thomas, BA, PGCE, PGDIP, MPhil Supervised by: Prof Jill Venus, Dr Conny Matera-Rogers and Dr Nicola Palmer Submitted in partial fulfilment for the award of the degree of PhD University of Wales Trinity Saint David. 2018 i ii DECLARATION This work has not previously been accepted in substance for any degree and is not being concurrently submitted in candidature for any degree. Signed (candidate) Date 15.02.2018 STATEMENT 1 This thesis is the result of my own investigations, except where otherwise stated. Where correction services have been used, the extent and nature of the correction is clearly marked in a footnote(s). Other sources are acknowledged by footnotes giving explicit references. A bibliography is appended. Signed (candidate) Date 15.02.2018 STATEMENT 2 I hereby give consent for my thesis, if accepted, to be available for photocopying and for inter- library loan, and for the title and summary to be made available to outside organisations. Signed (candidate) Date 15.02.2018 STATEMENT 3 I hereby give consent for my thesis, if accepted, to be available for deposit in the University’s digital repository. Signed (candidate) Date 15.02.2018 iii iv Abstract Understanding of what constitutes a tourism experience has been the focus of increasing attention in academic literature in recent years. For tourism businesses operating in an ever more competitive marketplace, identifying and responding to the needs and wants of their customers, and understanding how the product or consumer experience is created is arguably essential. -
Bedwas, Trethomas & Machen Community Council Register Of
Bedwas, Trethomas & Machen Community Council Register of Interests 2020-2021 Name Employment/ Election/other Corporate Contracts Land in area of LA Corporate Licenses Other interests business expenses bodies with LA tenancies to occupy land Amanda None None None None 37 Graig View, None None • Councillor for BTM Community Mcconnell Machen Council Caerphilly • Chair of Machen Community CF83 8SD- home Road Watch • Member of Welsh Labour Party • Governor at Machen Primary School • Committee Member of Bedwas Workmen’s Hall • Chair of Bedwas Workmen’s Hall Restoration Group • Chair of Land & Buildings Committee for BTM Community Council • Chair of Police & Road Safety Committee for BTM Community Council Chris Morgan GE Aviation None None None 32 St David’s Drive, None None • Chair – BTM CC LTD Machen • Unite – Secretary GE Aviation Cardiff Road Caerphilly Branch Nantgarw CF83 8RH – home • Chair – Lower GYR Community CF15 7YJ & Association Ty Mawr • Machen RFC – Committee Pandymawr Road member Bedwas • Bedwas High School – Governor CF83 8EQ • Labour Party - Member Page 1 of 5 Bedwas, Trethomas & Machen Community Council Register of Interests 2020-2021 Daniel None All expenses None None 32 Bevan Close, None None • Member of Paid Cymru Llewellyn paid by Plaid Trethomas • Councillor for Bedwas Ward Cymru Caerphilly • Member of YES Cymru CF83 8GR - home • Chair of Plaid Cymru (Caerphilly Constituency) • Member of Machen Top Club •Committee Member – Machen Workingman’s Club David J Davies Derek None Elected None None None 75Ridgeway None None • -

Bread and Butter Actions to Solve Poverty Listening to People 2Nd
Spring 2019 Wales’ best policy and politics magazine Bread and butter actions to solve poverty Mark Drakeford AM Listening to people Suzy Davies AM 2nd home tax loophole Siân Gwenllian AM ISSN 2059-8416 Print ISSN 2398-2063 Online CONTENTS: SPRING 2019 Wales’ best policy and politics magazine 50.open.ac.uk A unique space in the heart of Cardiff for everything connected with your wellbeing. 50 MLYNEDD O 50 YEARS OF Created by Gofal, the charity thinking differently about YSBRYDOLIAETH INSPIRATION mental health. Wedi’i seilio ar ei chred gadarn sef y dylai addysg fod yn Dedicated Workplace Wellbeing Programmes agored i bawb, mae’r Brifysgol Agored wedi treulio’r hanner A team of professional counsellors with a range of approaches canrif ddiwethaf yn helpu dysgwyr ledled Cymru a’r byd i droi’r Employee Assistant Programmes offering quality support amhosibl yn bosibl. Yn ystod carreg filltir ein pen-blwydd yn 50 oed, rydym yn creu rhaglen o ddigwyddiadau a gweithgareddau cyrous a fydd yn All profits will be reinvested into Gofal - amlygu’r myfyrwyr, sta, partneriaid a theulu’r Brifysgol sustainable wellbeing for all Agored sydd wedi gwneud ein sefydliad yr hyn ydyw heddiw. Mark Drakeford AM Alicja Zalesinska Alun Michael Company Number: 2546880 2 Solving poverty in Wales 10 Housing is a human right 18 The challenge of austerity Registered in England and Wales Registered Charity Number: 1000889 Founded on the firm belief that education should be open to to policing all, The Open University has spent the past fifty years helping learners from all over Wales and the world to make the impossible possible. -
Cwm Taf Morgannwg University Health Board Job Description
CWM TAF MORGANNWG UNIVERSITY HEALTH BOARD JOB DESCRIPTION POST: Consultant Physician in Geriatric & General Medicine SALARY: £72,927 - £94,679 per annum DIRECTORATE: Medicine and A&E BASE: Royal Glamorgan Hospital The post holder will also be required to provide services at other hospital sites. Introduction This is a new post, which is being created to develop and improve the Geriatric Medicine services in Cwm Taf Morgannwg University Health Board. The post will be subject to the terms and conditions of service governing the appointment of Medical and Dental Staff in Wales, and to the Health Board's terms and conditions as appropriate. The candidate to be appointed will be required to be fully registered with the General Medical Council, to hold, or to be within 6 months of gaining, a Certificate of Completion of Training in both Geriatric Medicine and General Internal Medicine, and to be on the Specialist Register. The post holder will be joining a dynamic, forward looking and innovative Geriatric Medicine team. The post holder will be based at Royal Glamorgan Hospital in Llantrisant, where the Health Board has acute hospital beds covering a range of medical and surgical specialities. The post holder will be expected to help and develop Geriatric Medicine services provided by the Health Board at the Royal Glamorgan Hospital and in the community setting. A sub-speciality interest will be encouraged but there is flexibility to support personal development in this regard. Key to the development of services will be to develop clinical relationships with the colleagues in the Directorate and Local Health Board as well as strengthening working relationships with Primary Care colleagues in order to develop services locally. -
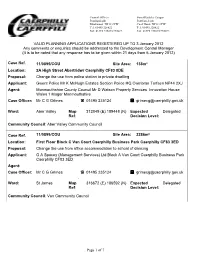
Page 1 of 7 VALID PLANNING APPLICATIONS REGISTERED UP
Council Offices Swyddfeydd y Cyngor Pontllanfraith Pontllan-fraith Blackwood NP12 2YW Coed Duon. NP12 2YW Tel: 01495 226622 Tel: 01495 226622 Fax: 01495 235013/235022 Fax: 01495 235013/235022 VALID PLANNING APPLICATIONS REGISTERED UP TO 3 January 2012 Any comments or enquiries should be addressed to the Development Control Manager (It is to be noted that any response has to be given within 21 days from 6 January 2012) Case Ref. 11/0895/COU Site Area: 138m² Location: 2A High Street Abertridwr Caerphilly CF83 8DE Proposal: Change the use from police station to private dwelling Applicant: Gwent Police Mr K McHugh Estates Section Police HQ Cwmbran Torfaen NP44 2XJ Agent: Monmouthshire County Council Mr D Watson Property Services Innovation House Wales 1 Magor Monmouthshire Case Officer: Mr C G Grimes 01495 235124 [email protected] 6 Ward: Aber Valley Map 312049 (E) 189448 (N) Expected Delegated Ref: Decision Level: Community Council: Aber Valley Community Council Case Ref. 11/0899/COU Site Area: 2286m² Location: First Floor Block C Van Court Caerphilly Business Park Caerphilly CF83 3ED Proposal: Change the use from office accommodation to school of dancing Applicant: GA Spacey (Management Services) Ltd Block A Van Court Caerphilly Business Park Caerphilly CF83 3ED Agent: Case Officer: Mr C G Grimes 01495 235124 [email protected] 6 Ward: St James Map 316672 (E) 186592 (N) Expected Delegated Ref: Decision Level: Community Council: Van Community Council Page 1 of 7 Case Ref. 11/0909/FULL Site Area: 2009m² Location: 5 Oak Tree Rise Homeleigh Newbridge Newport NP11 4RH Proposal: Erect a four bedroom family dwelling Applicant: Mr G Jones 5-9 Fern Close Penyfan Industrial Estate Crumlin Newport NP11 3EH Agent: Hurley & Davies Ltd Mr D Meek 1 Axis Court Riverside Business Park Swansea SA7 0AJ Case Officer: Mrs S Hockaday 01495 235163 [email protected] 6 Ward: Newbridge Map 320268 (E) 197029 (N) Expected Delegated Ref: Decision Level: Community Council: Not Applicable Case Ref. -
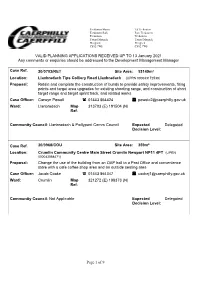
Page 1 of 9 VALID PLANNING APPLICATIONS RECEIVED up to 13 January 2021 Any Comments Or Enquiries Should Be Addressed to the Deve
Tredomen House Tŷ Tredomen Tredomen Park Parc Tredomen Tredomen Tredomen Ystrad Mynach Ystrad Mynach Hengoed Hengoed CF82 7WF CF82 7WF VALID PLANNING APPLICATIONS RECEIVED UP TO 13 January 2021 Any comments or enquiries should be addressed to the Development Management Manager Case Ref. 20/0703/RET Site Area: 53149m² Location: Llanbradach Tips Colliery Road Llanbradach (UPRN 000043172539) Proposal: Retain and complete the construction of bunds to provide safety improvements, firing points and target area upgrades for existing shooting range, and construction of short target range and target sprint track, and related works Case Officer: Carwyn Powell 01443 864424 [email protected] Ward: Llanbradach Map 313703 (E) 191504 (N) Ref: Community Council: Llanbradach & Pwllypant Comm Council Expected Delegated Decision Level: Case Ref. 20/0968/COU Site Area: 359m² Location: Crumlin Community Centre Main Street Crumlin Newport NP11 4PT (UPRN 000043068471) Proposal: Change the use of the building from an OAP hall to a Post Office and convenience store with a cafe coffee shop area and an outside seating area Case Officer: Jacob Cooke 01443 864347 [email protected] Ward: Crumlin Map 321272 (E) 198373 (N) Ref: Community Council: Not Applicable Expected Delegated Decision Level: Page 1 of 9 Case Ref. 20/1004/FULL Site Area: 339m² Location: 26 Heol Isaf Nelson Treharris CF46 6NS (UPRN 000043007925) Proposal: Erect single storey extension to rear and side of property Case Officer: Jacob Cooke 01443 864347 [email protected] -

HEFCW Circular W20/09HE: Annex B 1 Research Wales Innovation Fund
HEFCW circular W20/09HE: Annex B Research Wales Innovation Fund Strategy 2020/21 – 2022/23 Institution: Swansea University RWIF strategy lead: Prof. Marcus Doel, Deputy PVC – Research & Innovation Prof. Martin Stringer, PVC – Student Experience & Civic Mission Emma Dunbar- Head of Engagement, Innovation, Employability & Enterprise, REIS Email: [email protected] [email protected] [email protected] Telephone : 07860736047 (Emma Dunbar) Section A: Overview 1. Strategic ambitions Please provide an overview of your institution’s 3 year [and beyond if longer term plans are available] approach to research and innovation activity which will be supported by RWIF. You may wish to highlight broad areas which you are targeting, and describe how RWIF funding will align with your institutional mission and internal strategies. [max 300 words] This 3 year strategy comes at a particular moment in our history, when celebrating our centenary, we have had to come together as a community in response to the Covid-19 pandemic. We will use this opportunity to reflect on what we might achieve over the next few years that will resonate for our second century. We are proud to belong to the City of Swansea and the wider Swansea Bay City Region (SBCR) and we celebrate that heritage. We will strengthen our position within the SBCR, as the region’s major university, with the quality and scale of research and innovation to facilitate powerful strategic collaborations between universities, government funding bodies, our extensive SME network, large companies, and their supply chains; and to deliver transformational economic and social benefits both within Wales, the UK and across the rest of the world. -

CONFERENCE VENUE Swansea University Wallace Building
CONFERENCE VENUE Swansea University Wallace Building The Wallace Building, Swansea University The conference venue for the UKIRSC 2019 is the Wallace Building on Singleton Campus, Swansea University, SA2 8PP. The Wallace Building is home to the Bioscience and Geography departments and is named after the “father of biogeography”, Alfred Russel Wallace, Welsh evolutionary biologist best known for having independently conceived the theory of evolution through natural selection, alongside Charles Darwin. Swansea University is situated in Singleton Park, a mature parkland and botanical gardens overlooking Swansea Bay beach. The Wallace Building is in the South West corner of Singleton Campus. It is approximately 15 minutes’ walk from the Uplands or Brynmill areas, 40 minutes’ walk from Swansea City Centre and 3 minutes from the beach (see map on page 5). 1 Registration will be held in the entrance foyer of the Wallace building. From there you can head directly upstairs to the Science Central for refreshments. Scientific posters will be displayed here. All guest lectures and student talks will take place in the Wallace Lecture Theatre, directly ahead on entering the Wallace Building and located down a short flight of stairs. Tea and coffee will be provided on arrival and during breaks, but please bring your own re-usable cup. Lunch is not provided. There are plenty of options for lunch on campus and in the Uplands and Brynmill area just short walk away. The Wallace Building Foyer. Down the stairs and ahead to the Wallace Lecture Theatre or up the stairs to Science Central. 2 ACCOMODATION Staying with Students There should be a limited number of beds/sofas available with students based in Swansea. -

Notices and Proceedings for Wales
OFFICE OF THE TRAFFIC COMMISSIONER (WALES) (CYMRU) NOTICES AND PROCEEDINGS PUBLICATION NUMBER: 2011 PUBLICATION DATE: 14 August 2014 OBJECTION DEADLINE DATE: 04 September 2014 Correspondence should be addressed to: Office of the Traffic Commissioner (Wales) (Cymru) Hillcrest House 386 Harehills Lane Leeds LS9 6NF Telephone: 0300 123 9000 Fax: 0113 249 8142 Website: www.gov.uk The public counter at the above office is open from 9.30am to 4pm Monday to Friday The next edition of Notices and Proceedings will be published on: 28/08/2014 Publication Price £3.50 (post free) This publication can be viewed by visiting our website at the above address. It is also available, free of charge, via e-mail. To use this service please send an e-mail with your details to: [email protected] The Welsh Traffic Area Office welcomes correspondence in Welsh or English. Ardal Drafnidiaeth Cymru yn croesawu gohebiaeth yn Gymraeg neu yn Saesneg. Remember to keep your bus registrations up to date - check yours on https://www.gov.uk/manage-commercial-vehicle-operator-licence-online NOTICES AND PROCEEDINGS Important Information All correspondence relating to public inquiries should be sent to: Office of the Traffic Commissioner (Wales) (Cymru) 38 George Road Edgbaston Birmingham B15 1PL The public counter at the Birmingham office is open for the receipt of documents between 9.30am and 4pm Monday Friday. There is no facility to make payments of any sort at the counter. General Notes Layout and presentation – Entries in each section (other than in section 5) are listed in alphabetical order.