Abdominal Radiograph
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Perforated Ulcers Shaleen Sathe, MS4 Christina Lebedis, MD CASE HISTORY
Perforated Ulcers Shaleen Sathe, MS4 Christina LeBedis, MD CASE HISTORY 54-year-old male with known history of hypertension presents with 2 days of acute onset abdominal pain, nausea, vomiting, and diarrhea, with periumbilical tenderness and abdominal distention on exam, without guarding or rebound tenderness. Labs, including CBC, CMP, and lipase, were unremarkable in the emergency department. Radiograph Perforated Duodenal Ulcer Radiograph of the chest in the AP projection shows large amount of free air under diaphragm (blue arrows), suggestive of intraperitoneal hollow viscus perforation. CT Perforated Duodenal Ulcer CT of the abdomen in the axial projection (I+, O-), at the level of the inferior liver edge, shows large amount of intraperitoneal free air (blue arrows) in lung window (b), and submucosal edema in the gastric antrum and duodenal bulb (red arrows), suggestive of a diagnosis of perforated bowel, most likely in the region of the duodenum. US Perforated Gastric Ulcer US of the abdomen shows perihepatic fluid (blue arrow) and free fluid in the right paracolic gutter (not shown), concerning for intraperitoneal pathology. Radiograph Perforated Gastric Ulcer Supine radiograph of the abdomen shows multiple air- filled dilated loops of large bowel, with air lucencies on both sides of the sigmoid colon wall (green arrows), consistent with Rigler sign and perforation. CT Perforated Gastric Ulcer CT of the abdomen in the axial (a) and sagittal (b) projections (I+, O-) shows diffuse wall thickening of the gastric body and antrum (green arrows) with an ulcerating lesion along the posterior wall of the stomach (red arrows), and free air tracking adjacent to the stomach (blue arrow), concerning for gastric ulcer perforation. -

Clinical Acute Abdominal Pain in Children
Clinical Acute Abdominal Pain in Children Urgent message: This article will guide you through the differential diagnosis, management and disposition of pediatric patients present- ing with acute abdominal pain. KAYLEENE E. PAGÁN CORREA, MD, FAAP Introduction y tummy hurts.” That is a simple statement that shows a common complaint from children who seek “M 1 care in an urgent care or emergency department. But the diagnosis in such patients can be challenging for a clinician because of the diverse etiologies. Acute abdominal pain is commonly caused by self-limiting con- ditions but also may herald serious medical or surgical emergencies, such as appendicitis. Making a timely diag- nosis is important to reduce the rate of complications but it can be challenging, particularly in infants and young children. Excellent history-taking skills accompanied by a careful, thorough physical exam are key to making the diagnosis or at least making a reasonable conclusion about a patient’s care.2 This article discusses the differential diagnosis for acute abdominal pain in children and offers guidance for initial evaluation and management of pediatric patients presenting with this complaint. © Getty Images Contrary to visceral pain, somatoparietal pain is well Pathophysiology localized, intense (sharp), and associated with one side Abdominal pain localization is confounded by the or the other because the nerves associated are numerous, nature of the pain receptors involved and may be clas- myelinated and transmit to a specific dorsal root ganglia. sified as visceral, somatoparietal, or referred pain. Vis- Somatoparietal pain receptors are principally located in ceral pain is not well localized because the afferent the parietal peritoneum, muscle and skin and usually nerves have fewer endings in the gut, are not myeli- respond to stretching, tearing or inflammation. -

Complicated Pseudodiverticulosis of Small Intestine: a Rare Case Report
International Surgery Journal Raj MK et al. Int Surg J. 2019 Sep;6(9):3433-3437 http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902 DOI: http://dx.doi.org/10.18203/2349-2902.isj20194096 Case Report Complicated pseudodiverticulosis of small intestine: a rare case report Kamal Raj M., V. Venkatachalam*, Manasa A. Institute of General Surgery, Madras Medical College, Chennai, Tamil Nadu, India Received: 08 July 2019 Revised: 16 August 2019 Accepted: 19 August 2019 *Correspondence: Dr. V. Venkatachalam, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Diverticular disease though being a common entity in large bowel is recently noted to occur more proximally as well. In the jejunum, the mucosal outpouchings, called as pseudo-diverticulae, occurs with an incidence of 0.5-1.5%. Diagnosed incidentally as majority of them remain asymptomatic. When they are symptomatic, dyspepsia and bloating, recurrent abdominal cramping, malabsorption and megaloblastic anemia occurs. On occasions it is not uncommon for patients to present with hemorrhage, infections, obstruction or perforation. Perforation, being a rare presentation occurs in less than 6% of the cases. We present a case of a 70 year old male, who presented as acute abdomen, found to have isolated jejunal diverticular perforation intraoperatively. Keywords: Jejunal diverticula, Perforation, Acute abdomen, Pseudo-diverticulae INTRODUCTION for 2 days. He also gave history of dyspepsia and bloating following food consumption. -

Postpartum Pneumoperitoneum and Peritonitis After Water Birth Brown Et Al
Gastrointestinal Radiology: Postpartum pneumoperitoneum and peritonitis after water birth Brown et al. Postpartum pneumoperitoneum and peritonitis after water birth Vanessa Brown 1, Sascha Dua 1*, Anna Athow 1, Rudi Borgstein 1, Oladapo Fafemi 1 1. Department of General Surgery, North Middlesex University Hospital Trust, London, UK * Correspondence: Miss Sascha Dua, 18 Eton Rise, Eton College Road, London, NW3 2DD, UK ( [email protected] ) Radiology Case. 2009 Apr; 3(4): 1-4 :: DOI: 10.3941/jrcr.v3i4.12 ABSTRACT Pneumoperitoneum (the presence of free gas in the peritoneal cavity) usually indicates gastrointestinal perforation with associated peritoneal contamination. We describe the unusual case of a 28-year-old female, who was 7 days postpartum and presented with features of peritonitis that were www.RadiologyCases.com www.RadiologyCases.com initially missed despite supporting radiological evidence. The causes of pneumoperitoneum are discussed. In the postpartum period the female genital tract provides an alternative route by which gas can enter the abdominal cavity and cause pneumoperitoneum. In the postpartum period it is important to remember that the clinical signs of peritonism, guarding and rebound tenderness may be diminished or subtle due to abdominal wall laxity. CASE REPORT Journalof Radiology Case Reports was performed (Fig. 1) and the patient referred to the CASE REPORT gynaecologist who requested an ultrasound of the abdomen A 28-year-old woman presented to the emergency department and pelvis to rule out retained products of conception (Fig. 2). with a two-day history of generalised abdominal pain. She had The ultrasound showed a bulky uterus with a small amount of given birth to her first child three days previously at home. -

Non-Traumatic Abdominal Emergency Imaging Hepatobiliary Emergency
บทความวชาการิ Non-Traumatic Abdominal Emergency Imaging Hepatobiliary Emergency จฬาลุ กษณั ์ พรหมศร ภาควิชารังสีวิทยา คณะแพทยศาสตร์ มหาวิทยาลัยขอนแก่น Non Traumatic Abdominal Emergency Imaging invasive amebiasis Hepatobiliary Emergency o Antibody to Entamoeba rising - Liver abscess o trophosoites ascend via portal vein then - Cholangitis invaded parenchyma - Acute cholecystitis o chocolate-colored, pasty material (anchovy - Gall stone ileus paste) - Mirizzi syndrome o single/multipe Periperheral near capsule Pancreatitis - Fungal liver abscess Appendicitis o Pts hematologic malignancy or compromised Small bowel obstruction o Microabcess involving liver, spleen and Peptic Ulcer perforation kidneys Mid gut volvulous o Leukemia/ most common Candia albicans Sigmoid volvulous o Other; Cryptococcus, histoplasmosis, Mesenteric vascular ischemia mucormycosis, Aspergillus Diverticulitis o Size 2-20 mm Imaging tools Acute abdomen series Imaging; Chest upright - Plain film; hepatomegaly, intrahepatic gas/an Abdomen upright fluid level Abdomen supine - US: Left lateral decubitus o variable in shape and echo (hypoechoic, Ultrasound hyperechoic, anechoic) with septation, fluid level CT without and with posterior enhancement MRI o Amebic; round/oval hypoechoic mass abuts liver capsule Liver abscess o Fungal; multiple tiny small echoic lesions - Pyogenic liver abscess scattered through liver parenchyma o(K pneumonia, E coli, Enterococcus, o US, CT 4 patterns of hepatosplenic Burkholderia, Streptococcus, and Staphylococcus spe- candidiasis cies) 1. wheel-within-a wheel; central hypoechic of o Solitary necrosis containing fungal, surrounded echogenic o Multiple inflammatory cells o Few mm- cm 2. Bull’s-eye of central echogenic nidus surrounded - Amebic liver abscess by hypoechoic rim( pts active fungal infection with nor- o Amebic liver abscess; E.Histolytica mal white cell) o most common extraintestinal from of 3. -

Acute Abdomen
Acute abdomen CASE 1: 46Y♀VOMITING 新光吳火獅紀念醫院 VS 許瓅文 103.09.09 46Y♀vomiting • Chief complaint •Past Hx – Abdominal pain, vomiting and no appetite for 2 – Ectopic pregnancy s/p OP 20yrs ago days – Pregnancy: denied • Present illness •PE – Intermittent abdominal pain – Abdomen: – Abdominal distention(+) diffuse tender(+) – Vomitus: yellowish/ greenish fluid no rebound pain – No flatus bowel sound: hypoactive – Similar episode before percussion: tympanic Impression?/ Order KUB (EIA: negative) • CBD/DC/Plt Hx • Standing abdomen • Panel Ⅰ/ T-bil/ Lipase Site of tender • PT/aPTT OP? •KUB (待EIA) Anticoagulant use? • Urine EIA •NPO • D5S run 60mL/hr Adhesion ileus Order Clinical feature •2nd KUB: ileus improved •2nd KUB: fixed bowel loop • Flatus(+), abdominal • Fever(+) • Promeran 1amp iv q6h & st Severe distension pain and distension vomiting • Persisted abd.pain • On NG with decompression improved • Rebound pain(+) • D5S run 120mL/hr Try water and soft diet Fluid resuscitation • NG decompression: 量多, • 排GI床/ 待轉EC Dry mouth/ UOP No discomfort greenish AKI? Prerenal azotemia? • f/u KUB 8hrs later MBD =>what’s next? Order Ileus • Abdominal CT with/without contrast • Abd OP Hx + ileus ≒ adhesion ileus =>empiric • B/C xⅡ Tx Bowel obstruction: • Be ware of mechanical bowel obstruction!!! • Cefmetazole 1g iv q8h & st bezoar => OP => CT indication/ OP indicated • Be ware of medication ↓ bowel motility for Abd OP Hx Pt Terminal ileitis 78y♂ Abdominal pain • Chief complaint – Abdominal pain since 6 hrs ago • Present illness – 看護:一陣一陣喊肚子痛 – Vomiting once, food content CASE 2: 78Y♂ ABDOMINAL PAIN – Diarrhea for 2 times, watery, brownish/ yellowish – No fever •Past Hx – Old CVA with bed-ridden/ DM/ HTN/ CAD Hx Impression?/ Order – Abd OP Hx: nil •NPO • PE: • D5S run 60mL/hr – Chest: clear BS, IRHB • CBD/DC/Plt – Abdomen: soft, no tender point •F/S DKA? no rebound pain • VBG G6 檢查項目避免重複開立 – Ext: warm, no pitting edema • Cr, AST, lipase, T-bil •KUB •ECG Previous ECG: Af OPD drug: warfarin 3mg qd • PT/aPTT Lab data/ Image Impression?/ Order • WBC: 22000/ seg. -
![Pdf Talk [Compatibility Mode]](https://docslib.b-cdn.net/cover/4561/pdf-talk-compatibility-mode-1964561.webp)
Pdf Talk [Compatibility Mode]
13/11/55 IMAGING MODALITIES Improve reading skill of abdominal imaging • PLAIN FILM • ULTRASONOGRAPHY • BARIUM EXAMINATION ผศ นพ สิทธิพงศ ศรีสัจจากุล BODY IMAGING • CT Department of Radiology, SirirajHospital, • MRI MahidolUniversity • PET @ King ChulalongkornMemorial Hospital, 25 november12 PLAIN FILM • ACUTE ABDOMINAL SERIES -CXR upright PLAIN FILM -Plain abdomen supine and upright Density in Plain Film Plain Abdomen: Upright View 3 Liver 4 2 3 1 1 = air Properitoneal 2 = fat fat line 4 Abdominal 3 = soft tissue wall 5 4 = bone Small bowel loops 5 = metallic 1 PDF created with pdfFactory Pro trial version www.pdffactory.com 13/11/55 Plain Abdomen: Supine View Plain Abdomen vs Plain KUB Transverse Stomach colon Descending colon Supine Plain KUB PLAIN ABDOMEN How to read plain abdomen 1 Abdominal wall and properitonealfat line 2 Distance between bowel wall and abdominal Peripheral to central approach or vice versa wall 3 Gas distribution in GI tract ( stomach, small bowel and large bowel) 4 Soft tissue density in abdomen such as solid organs, fluid-filled bowel loops PLAIN ABDOMEN 5 Bony structures 6 Detection of abnormalities -Abnormal gas -free air , bowel dilatation, pneumatosis -Abnormal mass -intraperitoneumor retroperitoneum -Organomegaly -Abnormal calcification -Foreign bodies 2 PDF created with pdfFactory Pro trial version www.pdffactory.com 13/11/55 ABNORMAL PLAIN FILM CXR upright moderate to marked pneumoperitoneum Plain abdomen upright triangular sign • ICU admission • Sick patient • No upright film liver diaphragm ascites -

The Survey Film in Acute Abdominal Disorders
Gratitude is expressed to Dr. Price E. Thomas, determine some of factors controlling rate of action of curare. J. Physiol. 106:20P, 1947. Department of Physiology, Kirksville College of 10. Kalow, W.: Hydrolysis of local anesthetics by human serum Osteopathy and Surgery, for his guidance in the cholinesterase. J. Pharmacol. Exper. Therap. 104:122-134, Feb. 1952. writing of this paper, and to Mrs. Kathryn Balder- 11. Beecher, H. K., and Murphy, A. J.: Acidosis during thoracic son for preparation of the diagrams. surgery. J. Thoracic Surg. 19:50-70, Jan. 1950. 12. Lehmann, H., and Silk, E.: Succinylrnonocholine. Brit. M. J. 1:767-768, April 4, 1953. 13. Frumin, J. M.: Hepatic inactivation of succinylcholine in dog. Fed. Proc. 17:368, 1958. 1. Boba, A., et al.: Effects of apnea, endotracheal suction, and 14. Barnes, J. M., and Davies, D. R.: Blood cholinesterase levels oxygen insufflation, alone and in combination, upon arterial oxygen in workers exposed to organo-phosphorous insecticides. Brit. M. J. saturation in anesthetized patients. J. Lab. Clin. Med. 53:680-685, 2:816-819, Oct. 6, 1951. May 1959. 15. Lehmann, H., and Ryan, E.: Familial incidence of low pseudo- 2. Bard, P.: Medical physiology. Ed. 10. C. V. Mosby Co., St. cholinesterase level. Lancet 2:124, July 21, 1956. Louis, 1956. 16. Lehmann, H., and Simmons, P. H.: Sensitivity to suxame- 3. Ruch, T. C., and Fulton, J. F.: Medical physiology and bio- thonium; apnoea in two brothers. Lancet 2:981-982, Nov. 8, 1958. physics. Ed. 18. W. B. Saunders Co., Philadelphia, 1960. 17. -
High Yield Points
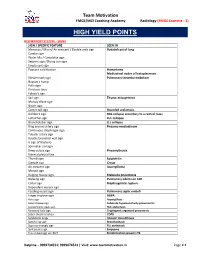
Team Motivation FMGE/MCI Coaching Academy Radiology (FMGE Essentia - 3) HIGH YIELD POINTS RESPIRATORY SYSTEM – SIGNS SIGN / SPECIFIC FEATURE SEEN IN Meniscus / Moon/ Air crescent / Double arch sign Hydatid cyst of lung Cumbo sign Water lilly / Camalotte sign Serpent sign / Rising sun sign Empty cyst sign Popcorn calcification Hamartoma Mediastinal nodes of histoplasmosis Westermark sign Pulmonary thrombo-embolism Hapton’s hump Palla sign Fleishner lines Felson’s sign Sail sign Thymic enlargement Mulvay Wave sign Notch sign Comet tail sign Rounded atelectasis Golden S sign RUL collapse secondary to a central mass Luftsichel sign LUL collapse Broncholobar sign LLL collapse Ring around artery sign Pneumo-mediastinum Continuous diaphragm sign Tubular artery sign Double bronchial wall sign V sign of Naclerio Spinnaker sail sign Deep sulcus sign Pneumothorax Visceral pleural line Thumb sign Epiglottitis Steeple sign Croup Air crescent sign Aspergilloma Monod sign Bulging fissure sign Klebsiella pneumonia Batwing sign Pulmonary edema on CXR Collar sign Diaphragmatic rupture Dependant viscera sign Feeding vessel sign Pulmonary septic emboli Finger in glove sign ABPA Halo sign Aspergillosis Head cheese sign Subacute hypersensitivity pneumonitis Juxtaphrenic peak sign RUL atelectasis Reversed halo sign Cryptogenic organized pneumonia Saber sheath trachea COPD Sandstorm lungs Alveolar microlithiasis Signet ring sign Bronchiectasis Superior triangle sign RLL atelectasis Split pleura sign Empyema Tree in bud sign on HRCT Endobronchial spread in TB -

Common Surgical Concerns Dr. Metzgar
COMMON SURGICAL Martha Metzgar, DO, CONCERNS FAAFP SURGERY ON AOBFP EXAM ¡EENT – 5% - Just the first E ¡General Surgery – 3% - some ¡Orthopedics – 3% - NOPE A 45-year-old female has ultrasonography of her kidneys as part of an evaluation for uncontrolled hypertension. The report notes an incidental finding of stones in the gallbladder, confirmed on right upper quadrant ultrasonography. She has no CASE 1 symptoms you can relate to the gallstones. Other than hypertension she has no chronic medical problems. Which one of the following should you recommend to her at this time regarding the gallstones? A) Expectant management B) Oral dissolution therapy C) Extracorporeal lithotripsy D) Endoscopic retrograde cholangiopancreatography(ERCP) E) Laparoscopic cholecystectomy BILIARY CONDITIONS ¡Cholecystitis §inflammation and infection of the gallbladder caused by blockage of the cystic duct ¡Cholelithiasis – Cause Biliary colic §Transient obstruction of the cystic duct with gallstone. ¡Choledocholithiasis § stone in the common bile duct – often causes increases in LFTs ¡Cholangitis §Inflammation of the bile ducts CHOLELITHIASIS ¡ Risk factors ¡ Asymptomatic - Obesity § 10% will be symptomatic - Rapid/Cyclic weight loss in 5 years § Childbearing § 25% in 10 years § Female § Expectant management § First degree relative ¡ Oral dissolution therapy § Native American or not helpful Scandinavian descent ¡ Symptomatic – surgery § Drugs - Ceftriaxone, estrogen, TPN ¡ Imaging of choice is § Increasing age ultrasound. § Ileal disease, resection, or bypass -

Perforated Duodenal Diverticulum with Subtle Pneumoretroperitoneum on Abdominal X-Ray
Hindawi Case Reports in Emergency Medicine Volume 2017, Article ID 7089573, 4 pages https://doi.org/10.1155/2017/7089573 Case Report Perforated Duodenal Diverticulum with Subtle Pneumoretroperitoneum on Abdominal X-Ray Yuzeng Shen and Mark Kwok Fai Leong Department of Emergency Medicine, Singapore General Hospital, Singapore Correspondence should be addressed to Yuzeng Shen; [email protected] Received 18 May 2017; Revised 25 August 2017; Accepted 17 September 2017; Published 19 October 2017 Academic Editor: Kalpesh Jani Copyright © 2017 Yuzeng Shen and Mark Kwok Fai Leong. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abdominal pain is one of the most common presenting complaints at the Emergency Department (ED). Given the myriad of possible differential diagnoses for abdominal pain, it becomes more important to diagnose conditions requiring emergent surgical intervention early. We present a case of an elderly male patient with abdominal pain secondary to perforated hollow viscus, subtle evidence of pneumoretroperitoneum on the initial supine abdominal X-ray, and review the signs of pneumoperitoneum and pneumoretroperitoneum on plain abdominal X-rays. 1. Introduction constipation, and vomiting episode may have been associated with consumption of tramadol tablets. There were no prior Perforated hollow viscus may result in pneumoperitoneum episodes of similar symptoms and no identified relieving or pneumoretroperitoneum, depending on the location of factors. He did not have any other associated symptoms perforation along the gastrointestinal tract [1, 2], and may such as fever, change in bowel habits, or history suggesting lead to significant mortality and morbidity. -

Abdominal X-Ray Radiological Signs
Abdominal X-ray Radiological Signs Suzanne O’Hagan Lightbulb moment a moment of sudden inspiration, revelation, or recognition Approach to AXR • Bowel gas pattern • Extraluminal air • Soft tissue masses • Calcifications Normal AXR Liver Gas in stomach Splenic flexure 11th rib T12 Psoas margin Left kidney Hepatic flexure Transverse colon Iliac crest Gas in sigmoid Sacrum Gas in caecum SI joint Bladder Femoral head Gas pattern What is normal? • Stomach – Almost always air in stomach • Small bowel – Usually small amount of air in 2 or 3 loops • Large bowel – Almost always air in rectum and sigmoid – Varying amount of gas in rest of large bowel Normal fluid levels • Stomach – Always (upright, decub) • Small bowel – Two or three levels acceptable (upright, decub) • Large bowel – None normally (functions to remove fluid) Large vs small bowel • Large bowel – Peripheral (except RUQ occupied by liver) – Haustral markings don’t extend from wall to wall • Small bowel – Central – Valvulae conniventes extend across lumen and are spaced closer together Radiographic principles Series of films for acute abdomen • Obstruction series/ Acute abdominal series/ Complete abdominal series – Supine (almost always) – Upright or left decubitus (almost always) – Prone or lateral rectum (variable) – Chest, upright or supine (variable) Acute abdominal series What to look for VIEW LOOK FOR SUPINE ABDOMEN Bowel gas pattern Calcifications Masses PRONE ABDOMEN Gas in rectosigmoid Gas in ascending and descending colon UPRIGHT ABDOMEN Free air, air-fluid levels UPRIGHT