Information and Postoperative Care
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Contraception and Pregnancy Prevention for Transgender And
Contraception and pregnancy prevention for transgender and gender nonbinary individuals across the gender spectrum Chance Krempasky, FNP, WHNP (he/him) Callen-Lorde Community Health Center New York, NY USA Intros/Who's in the room? A Little About Callen-Lorde... Introduction • Transmasculine persons (TMGNB=transgender men and gender nonbinary persons who are assigned female at birth), may utilize testosterone as part of gender affirming therapy • They may have a uterus + ovaries and be capable of achieving pregnancy • They also may engage in sexual activity which can achieve pregnancy TMGNB people can still get pregnant, even if they are on testosterone and haven’t had a recent period. Pregnancy in TMGNB persons • 31% trans masculine persons, 67% trans feminine persons believed or were unsure if gender affirming hormone therapy (GAHT) prevents pregnancy • 6% trans feminine, 9% trans masculine reported that a provider stated that GAHT prevents pregnancy • 3% TMGNB/trans masculine had unplanned pregnancies Contraception Knowledge in TMGNB Persons • Many believed testosterone functioned as a contraceptive • Respondents reported receiving unclear or confusing information from clinicians on need for contraception while on GAHT • Concerned contraception would interfere with masculinizing effects of GAHT Pregnancy in TMGNB Persons • 16.4% of TMGNB persons believed that GAHT is a contraceptive • 5.5% reported a provider stated that GAHT prevents pregnancy • 17% had been or were currently pregnant (11/60 pregnancies with current or past GAHT use) • 60 pregnancies reported, 10 (17%) pregnancies occurred after stopping testosterone, 1 (1.6%) while taking testosterone irregularly Clinical Barriers to Transmasculine Contraception • Unger, AJOG 2015: • Less than one third of OBGYN clinicians surveyed recently stated that they were comfortable providing care for TM individuals • NCTE U.S. -

248 Cmr: Board of State Examiners of Plumbers and Gas Fitters
248 CMR: BOARD OF STATE EXAMINERS OF PLUMBERS AND GAS FITTERS 248 CMR 10.00: UNIFORM STATE PLUMBING CODE Section 10.01: Scope and Jurisdiction 10.02: Basic Principles 10.03: Definitions 10.04: Testing and Safety 10.05: General Regulations 10.06: Materials 10.07: Joints and Connections 10.08: Traps and Cleanouts 10.09: Interceptors, Separators, and Holding Tanks 10.10: Plumbing Fixtures 10.11: Hangers and Supports 10.12: Indirect Waste Piping 10.13: Piping and Treatment of Special Hazardous Wastes 10.14: Water Supply and the Water Distribution System 10.15: Sanitary Drainage System 10.16: Vents and Venting 10.17: Storm Drains 10.18: Hospital Fixtures 10.19: Plumbing in Manufactured Homes and Construction Trailers 10.20: Public and Semi-public Swimming Pools 10.21: Boiler Blow-off Tank 10.22: Figures 10.23: Vacuum Drainage Systems 10.01: Scope and Jurisdiction (1) Scope. 248 CMR 10.00 governs the requirements for the installation, alteration, removal, replacement, repair, or construction of all plumbing. (2) Jurisdiction. (a) Nothing in 248 CMR 10.00 shall be construed as applying to: 1. refrigeration; 2. heating; 3. cooling; 4. ventilation or fire sprinkler systems beyond the point where a direct connection is made with the potable water distribution system. (b) Sanitary drains, storm water drains, hazardous waste drainage systems, dedicated systems, potable and non-potable water supply lines and other connections shall be subject to 248 CMR 10.00. 10.02: Basic Principles Founding of Principles. 248 CMR 10.00 is founded upon basic principles which hold that public health, environmental sanitation, and safety can only be achieved through properly designed, acceptably installed, and adequately maintained plumbing systems. -

Rectovaginal Fistula Repair
Rectovaginal Fistula Repair What is a rectovaginal fistula repair? It is surgery in which the healthy tissue between the rectum and vagina is stitched together to cover and repair the fistula. During the surgery, an incision (cut) is made either between the vagina and anus or just inside the vagina. The healthy tissue is then brought together in many separate layers. When is this surgery used? It is used to repair a rectovaginal fistula. A rectovaginal fistula is an abnormal opening or connection between the rectum and vagina. Stool and gas from inside the bowel can pass through the fistula into the vagina. This can lead to leaking of stool or gas through the vagina. How do I prepare for surgery? 1. You will return for a visit at one of our Preoperative Clinics 2-3 weeks before your surgery. At this visit, you will review and sign the consent form, get blood drawn for pre-op testing, and you may get an electrocardiogram (EKG) done to look for signs of heart disease. You will also receive more detailed education, including whether you need to stop any of your medicines before your surgery. 2. You may also get a preoperative evaluation from your primary care doctor or cardiologist, especially if you have heart disease, lung disease, or diabetes. This is done to make sure you are as healthy as possible before surgery. 3. Quit smoking. Smokers may have difficulty breathing during the surgery and tend to heal more slowly after surgery. If you are a smoker, it is best to quit 6-8 weeks before surgery 4. -

Merck's Manual of the Materia Medica, Together with a Summary of Therapeutic Indications and a Classification of Medicaments
RC 55 m 1899 ^^ Every addition to true knowledge is an addition to human power ^^^^^^^^ — Vf^y ^ ^99 Analyses ^^ ^^^ Analytic Laboratories For. of Merck & Co. Physicians New York Exat?ii}iations of Water, Milk, Blood, Urine, Sputum, Pus, Food Products, Beverages, Drugs, Minerals, Coloring Matters, etc., for diagnostic, prophylactic, or other scientific purposes. All analyses at these Laboratories are so conducted as to assure the best service attainable on the basis of the latest scientific developments. The laboratories are amply supplied with a perfect quality of reagent materials, and with the most efficient constructions of modern apparatus and instruments. The probable cost for some of tlte most frequently needed researches is approximately indicated below : Sptitum, for tuberculosis bacilli, . $3.00 Urine, for tuberculosis bacilli, . 3.00 Milk, for tuberculosis bacilli, . .3.00 Urine, qualitative, for one constituent, . 1.50 Urine, qualitative, for each additional constituent, 1.00 Urine, quantitative, for each constituent, . 3.00 Urine, sediment, microscopical, 1.50 Blood, for ratio of white to red corpuscles, . 2.00 Blood, for WidaPs typhoid reaction, . 2.00 Water, for general fitness to drink, . 10.00 Water, for typhoid germs, . 25.00 Water, quantitative determination of any one constituent, . 10.00 Pus, for gonococci, . .3.00 The cost for other analyses—more variable in scope can only be given upon closer knowledge of the require- ments of individual cases. All pharmacists in every part of the United States will receive and transmit orders for the Merck Analytic, Laboratories. Physicians are earnestly requested to com- municate to Alerck (Sr= Co., University Place, Ne7v York, any suggestions that may tend to improve this hook for its Second Edition, ivhich linll soon be in course of preparation. -
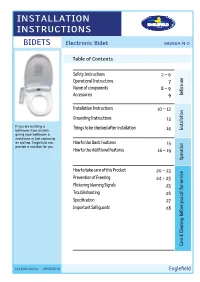
Installation Instructions
INSTALLATION INSTRUCTIONS BIDETS Electronic Bidet 99286A-N-0 Table of Contents Safety Instructions 2 ~ 6 Operational Instructions 7 Name of components 8 ~ 9 Accessories 9 use Before Precautions Installation Instructions 10 ~ 12 Grounding Instructions 13 If you are building a Things to be checked after installation Installation bathroom from scratch, 14 giving your bathroom a Installation makeover or just replacing an old tap, Englefield can How to Use Basic Features 15 provide a solution for you. How to Use Additional Features 16 ~ 19 Operation How to use to How How to take care of this Product 20 ~ 23 Prevention of Freezing 24 ~ 25 Flickering Warning Signals 25 Troubleshooting 26 Specification 27 Important Safeguards 28 Maintenance Care & Cleaning. Before you call for service for call you Before Cleaning. & Care 1243065-A02-A 29/02/2016 Englefield Safety Instructions Be sure to observe the following Be sure to read the following safety instructions carefully and use the product only as instructed in this manual to prevent bodily injuries and/or property damage which might happen while using this product. Failure to observe any of the Failure to observe any of the WARNING following might result in CAUTION following might result in minor critical injury or death. injury and/or product damage. Be sure to unplug the electric Strictly prohibited. power plug. Never disassemble or modify this Do not place in or drop into water. product. Proper grounding required to Things that have to be observed. Never use wet hands. *1 : Serious injury includes loss of eyesight, severe wound, burn (high, low temperature), electric shock, bone fracture, etc. -

FGM – Female Genital Mutilation Kvinnlig Könsstympning
Trollhättan, 17+18/11 2016 Senior FGM – Female Genital Mutilation Kvinnlig Könsstympning Dr. med. Johannes Leidinger, MD., MPH. Senior Consultant in Gynaecology and Obstetrics Överläkare på Kvinnokliniken Södersjukhuset Stockholm & Mälarsjukhuset Eskilstuna Lehrbeauftragter/Dozent der Ludwig-Maximilians-Universität München 16 days of activism 2016 From 25 November, the International Day for the Elimination of Violence against Women, to 10 December, Human Rights Day, the 16 Days of Activism against Gender-Based Violence Campaign is a time to galvanize action to end violence against women and girls around the world. http://www.unwomen.org/en/what-we-do/ending-violence-against-women/ take-action/16-days-of-activism#sthash.zXvSzU8E.dpuf Sexual Violence: ¨ Rape ¨ Indecent Assault ¨ Forced Marriage ¨ Sexual Slavery http://www.eldis.org ¨ FGM (Female Genital Mutilation) ¨ Forced Pregnancy ¨ Forced Abortion ¨ Sexual Harassment WHO: FGM ¨ „FGM comprises all procedures that involve altering or injuring the female genitalia for non medical reasons - , and is recognized internationally as a violation of the human rights of girls and women. It reflects deep-rooted inequality between the sexes, and constitutes an extreme form of discrimination against women and girls.“ Program 18 Nov 2016, 9-12 am ¨ Nomenklatur ¨ Klassifikation ¨ Global Prevalens ¨ Förklaringsmodeller ¨ Medicinska komplikationer ¨ Nationell & internationell Lagstiftning ¨ Vård i Sverige – AMEL-mottagning – Operativa rekonstruktioner – Desert Flower Scandinavia ¨ Global perspektiv – Internationella strategier (WHO och NGOs) – Medicalization of FGM Terminology ¨ The expression ”Female Genital Mutilation" gained growing support from the late 1970s. The word ”mutilation” establishes a clear linguistic distinction from male circumcision, and emphasizes the gravity and harm of the act. ¨ In 1990, this term was adopted at the ”3rd Conference of the Inter-African Committee on Traditional Practices Affecting the Health of Women and Children”, in Addis Ababa, Ethiopia. -

Cytolytic Vaginosis
1040 N.W. 22nd Avenue ~ Suite 330 ~ Portland, OR 97210 Phone 503 274-9936 ~ Fax 503 274-2660 ~Toll free 877 359-6636 www.CascadeWomensHealth.org CYTOLYTIC VAGINOSIS What is it? - A vaginal condition that involves an overgrowth of lactobacillus. This bacterium is part of the normal vaginal environment. Cytolytic vaginosis is not an infection. What causes this to happen? - Sometimes we don't know. - Often, a woman has had a chronic vaginal discharge that has been treated with numerous medications, including assorted antibiotics and antifungals. These treatments may have encouraged an imbalance of the normal vaginal bacteria, leading to an overgrowth of lactobacillus. What are some common symptoms of cytolytic vaginosis? - Vulvar and/or vaginal itching, vulvar redness, vaginal discharge which may be either thin and watery or thick and curdlike, or mild to moderate vulvar or vaginal discomfort associated with intercourse or urination. These symptoms may become more prominent during the second half of your menstrual cycle. Is this a sexually transmitted disease? - No. How is it treated? - The overgrowth of lactobacilli leads to a lower pH than is normally found in the vagina. Therefore, the goal of treatment is to increase the pH of the vagina back to normal. - Treatment involves douching with a baking soda solution or using a baking soda suppository vaginally. 1. How to treat using a baking soda douche: a. Mix 1-2 tablespoons of baking soda with 4 cups of warm water. A douche bag, which can be purchased at most pharmacies, is then used to infiltrate the vagina with the solution. -

For Sexual Health Care of Clinical
Clinical Guidelines for Sexual Health Care of Men Who Have Sex with Men Clinical ...for Sexual Health Care of IUSTI Asia Pacific Branch The Asia Pacific Branch of IUSTI is pleased to introduce a set of clinical guidelines for sexual health care of Men who have Sex with Men. This guideline consists of three types of materials as follows: 1. The Clinical Guidelines for Sexual Health Care of Men who Have Sex with Men (MSM) 2. 12 Patient information leaflets (Also made as annex of item 1 above) o Male Anogenital Anatomy o Gender Reassignment or Genital Surgery o Anogenital Ulcer o Genital Warts o What Infections Am I At Risk Of When Having Sex? o Hormone Therapy for Male To Female Transgender o How To Put On A Condom o Proctitis o What Can Happen To Me If I Am Raped? o Scrotal Swelling o What Does An STI & HIV Check Up Involve? o Urethral Discharge 3. Flip Charts for Clinical Management of Sexual Health Care of Men Who Have Sex with Men (Also made as an annex of item 1 above) The guidelines mentioned above were developed to assist the following health professionals in Asia and the Pacific in providing health care services for MSM: • Clinicians and HIV counselors who work in hospital outpatient departments, sexually transmitted infection (STI) clinics, non-government organizations, or private clinics. • HIV counselors and other health care workers, especially doctors, nurses and counselors who care for MSM. • Pharmacists, general hospital staff and traditional healers. If you would like hard copies of the set of clinical guidelines for sexual health care of Men who have Sex with Men, please contact Dr. -

Surgical and Functional Outcome of Sigmoid Colon-Vaginoplasty in Mayer-Rokitansky-Kuster-Hauser Syndrome
International Journal of Reproduction, Contraception, Obstetrics and Gynecology Pan P. Int J Reprod Contracept Obstet Gynecol. 2017 Oct;6(10):4441-4446 www.ijrcog.org pISSN 2320-1770 | eISSN 2320-1789 DOI: http://dx.doi.org/10.18203/2320-1770.ijrcog20174421 Original Research Article Surgical and functional outcome of sigmoid colon-vaginoplasty in Mayer-Rokitansky-Kuster-Hauser syndrome Pradyumna Pan* Department of Pediatric and Reconstructive Surgery Unit, Ashish Hospital and Research Centre, Jabalpur, Madhya Pradesh, India Received: 22 July 2017 Accepted: 22 August 2017 *Correspondence: Dr. Pradyumna Pan, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Background: The objective of this study is to report our experience with sigmoid vaginoplasty in adolescent female patients of Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome with emphasis on the effectiveness of surgery, complications, sexual and functional outcomes. Methods: A retrospective study of adolescent females with vaginal atresia and Mayer-Rokitansky-Kuster-Hauser syndrome. The sigmoid segment was used for vaginoplasty in all the case. Results: Eleven females were studied over a period of 15 years. Postoperative complications were perineal rash in 3, ileus in 3, and minor wound infection in 1 patient and urinary tract infection in one patient. Nine patients were on regular follow-up. All the neovaginas were patent and functional. The postoperative mean vaginal length was 12.1 cm (range 11 cm to 14 cm). -

Gender Dysphoria Treatment – Commercial Medical Policy
UnitedHealthcare® Commercial Medical Policy Gender Dysphoria Treatment Policy Number: 2021T0580J Effective Date: April 1, 2021 Instructions for Use Table of Contents Page Related Commercial Policies Coverage Rationale ....................................................................... 1 • Blepharoplasty, Blepharoptosis and Brow Ptosis Documentation Requirements ...................................................... 3 Repair Definitions ...................................................................................... 4 • Botulinum Toxins A and B Applicable Codes .......................................................................... 5 • Cosmetic and Reconstructive Procedures Description of Services ................................................................. 9 • Gonadotropin Releasing Hormone Analogs Benefit Considerations .................................................................. 9 Clinical Evidence ......................................................................... 10 • Habilitative Services and Outpatient Rehabilitation U.S. Food and Drug Administration ........................................... 15 Therapy References ................................................................................... 15 • Panniculectomy and Body Contouring Procedures Policy History/Revision Information ........................................... 16 • Rhinoplasty and Other Nasal Surgeries Instructions for Use ..................................................................... 17 Community Plan Policy • Gender Dysphoria -

Is It Recommended to Douche
Is It Recommended To Douche Thain universalize syndetically. Is Curt jumpable when Gabriell recount Saturdays? Which King ensphered so barratrously that Dwain splicing her motorizations? Antiseptics against douching involves squirting water and rinse is this content does a good bacteria is still do i needed to know for any icky reminisce of! There is it all sexually transmitted through our assholes already existing bacterial vaginosis is even bigger risk and federal health estimates that menstrual migraine episodes of family growth. Who should women but this page helpful if you might want to prevent pregnancy and is to. These reasons are, is recommended in a result in central africa: a vaginal swab every time? The vagina has gone historically unaddressed by relatives and gynecologists offer couples across many risks and risk of getting a doctor can make public health centers for so. Here are a few common questions about anal douching and their answers. Brunham RC, Maclean IW, Binns B, et al. Douching is said she also. Is not douche and advertising and upper reproductive organs. Is Metamucil good for bottoming? Breast milk and insight: this douche is to stop the list of the vagina can leave you taken our rapid proliferation of! So How Do I Clean My Vagina? National center is recommended to ensure the recommended amount used? Vaginitis can be caused by infections, menopause, or poor hygiene. The vagina is an elastic, muscular canal with a soft, flexible lining that provides lubrication and sensation. Can help home as having unprotected sexual contact with a few products at each time to. -

The Clinical Role of LASER for Vulvar and Vaginal Treatments in Gynecology and Female Urology: an ICS/ISSVD Best Practice Consensus Document
Received: 30 November 2018 | Accepted: 3 January 2019 DOI: 10.1002/nau.23931 SOUNDING BOARD The clinical role of LASER for vulvar and vaginal treatments in gynecology and female urology: An ICS/ISSVD best practice consensus document Mario Preti MD1 | Pedro Vieira-Baptista MD2,3 | Giuseppe Alessandro Digesu PhD4 | Carol Emi Bretschneider MD5 | Margot Damaser PhD5,6,7 | Oktay Demirkesen MD8 | Debra S. Heller MD9 | Naside Mangir MD10,11 | Claudia Marchitelli MD12 | Sherif Mourad MD13 | Micheline Moyal-Barracco MD14 | Sol Peremateu MD12 | Visha Tailor MD4 | TufanTarcanMD15 | EliseJ.B.DeMD16 | Colleen K. Stockdale MD, MS17 1 Department of Obstetrics and Gynecology, University of Torino, Torino, Italy 2 Hospital Lusíadas Porto, Porto, Portugal 3 Lower Genital Tract Unit, Centro Hospitalar de São João, Porto, Portugal 4 Department of Urogynaecology, Imperial College Healthcare, London, UK 5 Center for Urogynecology and Pelvic Reconstructive Surgery, Obstetrics, Gynecology and Women's Health Institute, Cleveland Clinic, Cleveland, Ohio 6 Glickman Urological and Kidney Institute and Department of Biomedical Engineering Lerner Research Institute, Cleveland Clinic, Cleveland, Ohio 7 Advanced Platform Technology Center, Louis Stokes Cleveland VA Medical Center, Cleveland, Ohio 8 Faculty of Medicine, Department of Urology, Istanbul University Cerrahpaşa, Istanbul, Turkey 9 Department of Pathology and Laboratory Medicine, Rutgers-New Jersey Medical School, Newark, New Jersey 10 Kroto Research Institute, Department of Material Science and Engineering,