Accepted Abstracts
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dissecting Cellulitis
Patient Information Leaflet Dr Paul Farrant FRCP Consultant Dermatologist Janet Dix (Secretary to Dr Paul Farrant) Tel 01444 412273 Fax 01444 657397 Email [email protected] Web drpaulfarrant.co.uk Dissecting Cellulitis What is dissecting cellulitis? Dissecting cellulitis is a type of scarring hair loss that presents with pustules, boggy swellings, and sinuses within the scalp. What causes dissecting cellulitis? The cause of dissecting cellulitis is not known. It is associated with severe cystic acne known as acne conglobata, and hidradenitis suppurativa, which causes cystic swellings in the armpits and groin. In all of these conditions the hair follicle becomes blocked, dilates and ruptures. This causes an inflammatory response in the skin, which leads to pus formation, swellings and sinus formation. It is not uncommon for bacteria to be isolated from the skin but this is likely to be secondary to the inflammatory process. Is dissecting cellulitis inherited? Dissecting cellulitis is most commonly seen in Afro-Caribbean men but the racial predilection is more likely to be due to the shape and structural differences of Afro-Caribbean hair than a genetic predisposition to the condition. Hair care practices, such as clipping, may also play a role. It is not thought to be an inherited condition. What are the symptoms? Patients with dissecting cellulitis often complain of pain, tenderness and fluid discharge from the affected area. It is associated with hair loss. What does dissecting cellulitis look like? Dissecting Cellulitis is characterised by a localised area of hair loss, pustules, boggy swellings and sinus formation. Gentle pressure on the boggy areas may lead to expression of pus or serous fluid. -

Guidelines of Care for the 10 Most Common Dermatologic Diseases
1 Guidelines of Care for the 10 most common dermatologic diseases: Copyright by the American Academy of Dermatology, Inc. Disclaimer Adherence to these guidelines will not ensure successful treatment in every situation. Further, these guidelines should not be deemed inclusive of all proper methods of care or exclusive of other methods of care reasonably directed to obtaining the same results. The ultimate judgment regarding the propriety of any specific procedure must be made by the physician in light of all the circumstances presented by the individual patient. For the benefit of members of the American Academy of Dermatology who practice in countries outside the jurisdiction of the United States, the listed treatments may include agents that not currently approved by the U.S. Food and Drug Administration. 1. Acne Vulgaris 2. Alopecia Areata 3. Atopic Dermatitis 4. Contact Dermatitis 5. Cutaneous Adverse Drug Reactions 6. Nail Disorders 7. Psoriasis 8. Superficial Mycotic Infections of the Skin: Mucocutaneous Candidiasis, Onychomycosis, Piedra, Pityriasis, Tinea Capitis , Tinea Barbae, Tinea Corporis, Tinea Cruris, Tinea Faciei, Tinea Manuum, and Tinea Pedis. 9. Vitiligo 10. Warts: Human Papillomavirus 1 2 1- Guidelines of Care for Acne Vulgaris* Reference: 1990 by the American Academy of Dermatology, Inc. I. Introduction The American Academy of Dermatology’s Committee on Guidelines of Care is developing guidelines of care for our profession. The development of guidelines will promote the continued delivery of quality care and assist those outside our profession in understanding the complexities and boundaries of care provided by dermatologists. II. Definition Acne vulgaris is a follicular disorder that affects susceptible pilosebaceous follicles, primarily of the face, neck, and upper trunk, and is characterized by both noninflammatory and inflammatory lesions. -

Pediatric and Adolescent Dermatology
Pediatric and adolescent dermatology Management and referral guidelines ICD-10 guide • Acne: L70.0 acne vulgaris; L70.1 acne conglobata; • Molluscum contagiosum: B08.1 L70.4 infantile acne; L70.5 acne excoriae; L70.8 • Nevi (moles): Start with D22 and rest depends other acne; or L70.9 acne unspecified on site • Alopecia areata: L63 alopecia; L63.0 alopecia • Onychomycosis (nail fungus): B35.1 (capitis) totalis; L63.1 alopecia universalis; L63.8 other alopecia areata; or L63.9 alopecia areata • Psoriasis: L40.0 plaque; L40.1 generalized unspecified pustular psoriasis; L40.3 palmoplantar pustulosis; L40.4 guttate; L40.54 psoriatic juvenile • Atopic dermatitis (eczema): L20.82 flexural; arthropathy; L40.8 other psoriasis; or L40.9 L20.83 infantile; L20.89 other atopic dermatitis; or psoriasis unspecified L20.9 atopic dermatitis unspecified • Scabies: B86 • Hemangioma of infancy: D18 hemangioma and lymphangioma any site; D18.0 hemangioma; • Seborrheic dermatitis: L21.0 capitis; L21.1 infantile; D18.00 hemangioma unspecified site; D18.01 L21.8 other seborrheic dermatitis; or L21.9 hemangioma of skin and subcutaneous tissue; seborrheic dermatitis unspecified D18.02 hemangioma of intracranial structures; • Tinea capitis: B35.0 D18.03 hemangioma of intraabdominal structures; or D18.09 hemangioma of other sites • Tinea versicolor: B36.0 • Hyperhidrosis: R61 generalized hyperhidrosis; • Vitiligo: L80 L74.5 focal hyperhidrosis; L74.51 primary focal • Warts: B07.0 verruca plantaris; B07.8 verruca hyperhidrosis, rest depends on site; L74.52 vulgaris (common warts); B07.9 viral wart secondary focal hyperhidrosis unspecified; or A63.0 anogenital warts • Keratosis pilaris: L85.8 other specified epidermal thickening 1 Acne Treatment basics • Tretinoin 0.025% or 0.05% cream • Education: Medications often take weeks to work AND and the patient’s skin may get “worse” (dry and red) • Clindamycin-benzoyl peroxide 1%-5% gel in the before it gets better. -

Early Diagnosis and Treatment of Discoid Lupus Erythematosus
J Am Board Fam Med: first published as 10.3122/jabfm.2009.02.080075 on 5 March 2009. Downloaded from BRIEF REPORT Early Diagnosis and Treatment of Discoid Lupus Erythematosus Suresh Panjwani, MD, MSc, FRACGP Discoid lupus erythematosus is a chronic dermatological disease that can lead to scarring, hair loss, and hyperpigmentation changes in skin if it is not treated early and promptly. It has a prolonged course and can have a considerable effect on quality of life. Early recognition and treatment improves the prog- nosis. The diagnosis is usually made by clinical examination. In some cases histopathology may be re- quired to confirm the diagnosis. The histology is that of an inflammatory interface dermatosis. There is insufficient evidence for which treatment is most effective. Because lesions are induced or exacerbated by ultraviolet exposure, photoprotective measures are important. Potent topical steroids and antima- larials are the mainstay of treatment. Some cases of discoid lupus erythematosus can be refractory to standard therapy; in these cases retinoids, thalidomide, and topical tacrolimus offer alternatives, as do immunosuppressives like azathioprine, cyclosporine, mycophenolate mofetil, and methotrexate. (J Am Board Fam Med 2009;22:206–213.) Lupus erythematosus (LE) is thought to be an 5% of patients with discoid lupus may develop autoimmune disease among other connective tissue SLE1 and 25% of patients with SLE may develop diseases like scleroderma, rheumatoid arthritis, typical chronic discoid lesions at some time during copyright. -

Case of Persistent Regrowth of Blond Hair in a Previously Brunette Alopecia Areata Totalis Patient
Case of Persistent Regrowth of Blond Hair in a Previously Brunette Alopecia Areata Totalis Patient Karla Snider, DO,* John Young, MD** *PGYIII, Silver Falls Dermatology/Western University, Salem, OR **Program Director, Dermatology Residency Program, Silver Falls Dermatology, Salem, OR Abstract We present a case of a brunette, 64-year-old female with no previous history of alopecia areata who presented to our clinic with diffuse hair loss over the scalp. She was treated with triamcinolone acetonide intralesional injections and experienced hair re-growth of initially white hair that then partially re-pigmented to blond at the vertex. Two years following initiation of therapy, she continued to have blond hair growth on her scalp with no dark hair re-growth and no recurrence of alopecia areata. Introduction (CBC), comprehensive metabolic panel (CMP), along the periphery of the occipital, parietal and Alopecia areata (AA) is a fairly common thyroid stimulating hormone (TSH) test and temporal scalp), sisaipho pattern (loss of hair in autoimmune disorder of non-scarring hair loss. antinuclear antibody (ANA) test. All values were the frontal parietotemporal scalp), patchy hair unremarkable, and the ANA was negative. The loss (reticular variant) and a diffuse thinning The disease commonly presents as hair loss from 2 any hair-bearing area of the body. Following patient declined a biopsy. variant. Often, “exclamation point hairs” can be hair loss, it is not rare to see initial growth of A clinical diagnosis of alopecia areata was seen in and around the margins of the hair loss. depigmented or hypopigmented hair in areas made. The patient was treated with 5.0 mg/mL The distal ends of these hairs are thicker than the proximal ends, and they are a marker of active of regrowth in the first anagen cycle. -
A Practical Approach to the Diagnosis and Management of Hair Loss in Children and Adolescents
A Practical Approach to the Diagnosis and Management of Hair Loss in Children and Adolescents The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Xu, Liwen, Kevin X. Liu, and Maryanne M. Senna. 2017. “A Practical Approach to the Diagnosis and Management of Hair Loss in Children and Adolescents.” Frontiers in Medicine 4 (1): 112. doi:10.3389/ fmed.2017.00112. http://dx.doi.org/10.3389/fmed.2017.00112. Published Version doi:10.3389/fmed.2017.00112 Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:34375289 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA REVIEW published: 24 July 2017 doi: 10.3389/fmed.2017.00112 A Practical Approach to the Diagnosis and Management of Hair Loss in Children and Adolescents Liwen Xu1†, Kevin X. Liu1† and Maryanne M. Senna2* 1 Harvard Medical School, Boston, MA, United States, 2 Department of Dermatology, Massachusetts General Hospital, Boston, MA, United States Hair loss or alopecia is a common and distressing clinical complaint in the primary care setting and can arise from heterogeneous etiologies. In the pediatric population, hair loss often presents with patterns that are different from that of their adult counterparts. Given the psychosocial complications that may arise from pediatric alopecia, prompt diagnosis and management is particularly important. Common causes of alopecia in children and adolescents include alopecia areata, tinea capitis, androgenetic alopecia, traction Edited by: alopecia, trichotillomania, hair cycle disturbances, and congenital alopecia conditions. -
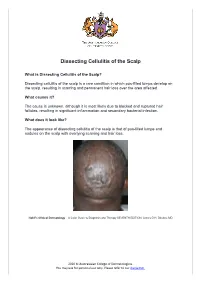
Dissecting Cellulitis of the Scalp
Dissecting Cellulitis of the Scalp What is Dissecting Cellulitis of the Scalp? Dissecting cellulitis of the scalp is a rare condition in which pus-filled lumps develop on the scalp, resulting in scarring and permanent hair loss over the area affected. What causes it? The cause is unknown, although it is most likely due to blocked and ruptured hair follicles, resulting in significant inflammation and secondary bacterial infection. What does it look like? The appearance of dissecting cellulitis of the scalp is that of pus-filled lumps and nodules on the scalp with overlying scarring and hair loss. Habif’s Clinical Dermatology – A Color Guide to Diagnosis and Therapy SEVENTH EDITION, James G.H. Dinulos, MD 2020 © Australasian College of Dermatologists. You may use for personal use only. Please refer to our disclaimer. Habif’s Clinical Dermatology – A Color Guide to Diagnosis and Therapy SEVENTH EDITION, James G.H. Dinulos, MD What other problems can occur with the condition? Other conditions related to hair follicle blockage, rupture and inflammation can occur with dissecting cellulitis of the scalp. They are known as the “follicular occlusion tetrad” and include acne conglobata (a severe form of acne), hidradenitis suppurativa (boils and cysts in the body folds) and pilonidal sinus (an infected cyst at the base of the spine). In addition, inflammation of the joints (arthritis) and bones can rarely occur in association with these conditions. How is it diagnosed? The condition can usually be diagnosed by clinical appearance by a dermatologist examining the scalp. Swabs of pus and plucked hairs can be analysed to rule out infections. -

Hair Loss in Women
T h e new england journal o f medicine clinical practice Hair Loss in Women Jerry Shapiro, M.D. This Journal feature begins with a case vignette highlighting a common clinical problem. Evidence supporting various strategies is then presented, followed by a review of formal guidelines, when they exist. The article ends with the author’s clinical recommendations. A 45-year-old white woman presents with a 1-year history of scalp-hair loss. She was hospitalized with appendicitis 14 months ago. She has been a vegetarian for 20 years. She takes no medications. Her father was bald. On physical examination, she has dif- fuse, nonscarring hair thinning with a widened part over the central portion of the scalp. How should this problem be evaluated and treated? The Clinical Problem From the Department of Dermatology Hair loss, or alopecia, is a very common presenting symptom, and more than one and Skin Science, University of British third of women have clinically significant hair loss during their lifetime. The effect Columbia, and Vancouver Coastal Health Research Institute — both in Vancouver, of hair loss on patients’ emotions is often greatly underestimated by physicians. Canada; and the Department of Derma- After bone marrow, hair is the second fastest growing tissue of the body. As a re- tology, New York University, New York. sult, many metabolic derangements can be manifested with alopecia, and hair loss Address reprint requests to Dr. Shapiro at the Department of Dermatology and may be the first clinical sign of systemic disease. Skin Science, University of British Co- lumbia, 835 W. -

Phototherapy, Photochemotherapy, and Excimer Laser Therapy for Dermatologic Conditions
Medical Coverage Policy Effective Date ............................................. 9/15/2021 Next Review Date ....................................... 9/15/2022 Coverage Policy Number .................................. 0031 Phototherapy, Photochemotherapy, and Excimer Laser Therapy for Dermatologic Conditions Table of Contents Related Coverage Resources Overview .............................................................. 1 Extracorporeal Photopheresis Coverage Policy ................................................... 1 General Background ............................................ 4 Medicare Coverage Determinations .................. 17 Coding/Billing Information .................................. 17 References ........................................................ 18 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage -

Alopecias in Lupus Erythematosus
Review Lupus Sci Med: first published as 10.1136/lupus-2018-000291 on 25 October 2018. Downloaded from Alopecias in lupus erythematosus Josef Symon Salgado Concha,1,2 Victoria P Werth1,2 To cite: Concha JSS, ABSTRACT of the hair in the absence of other causes.1 Werth VP. Alopecias in Several patterns of hair loss can occur in lupus Several processes that result in non-scarring lupus erythematosus. erythematosus (LE). Alopecias which show histological alopecia must therefore be ruled out before Lupus Science & Medicine characteristics of LE are LE-specific, and include discoid 2018;5:e000291. doi:10.1136/ attributing hair loss to LE (boxes 1 and 2). LE (DLE), diffuse or patchy hair loss in acute LE, subacute lupus-2018-000291 In this paper, we discuss an approach to cutaneous LE, and rarely tumid LE. Lupus hair in SLE is a recognising the different causes of hair loss poorly characterised entity and may be a form of telogen that occur in LE and their differential diag- Received 4 July 2018 effluvium. Alopecia areata can coexist with LE and may Revised 15 August 2018 mimic DLE. Non-lupus alopecias such as telogen effluvium noses. The categorisation we employ is largely Accepted 2 September 2018 and anagen effluvium have a myriad of causes which based on how scalp biopsy features are consis- include disease flares, drugs and stress in the setting tent with the diagnosis of LE. We also expand of LE. The latest validated Systemic Lupus International on the alternate diagnoses of non-scarring Collaborating Clinics classification criteria for SLE includes alopecia in LE. -

Scholars Journal of Medical Case Reports Alopecia Due to Demodexis
Akbarijo M et al.; Sch J Med Case Rep, September 2015; 3(9A):806-808 Scholars Journal of Medical Case Reports ISSN 2347-6559 (Online) Sch J Med Case Rep 2015; 3(9A):806-808 ISSN 2347-9507 (Print) ©Scholars Academic and Scientific Publishers (SAS Publishers) (An International Publisher for Academic and Scientific Resources) Alopecia due to demodexis M Akbarijo1, F Hashemi2, R Daie3, SJ Hashemi4* 1MSC microbiology, Tonekabon Branch, Tonekabon, Iran 2Student of school of pharmacy, Tehran University of Medical Sciences, Tehran, Iran 3,4Department of Medical Mycology, School of Public Health Research, Tehran University of Medical Sciences, Tehran, Iran *Corresponding author SJ Hashemi Email: [email protected] Abstract: Demodex is a common commensal mite of the pilosebaceous unit in human and animal (mammals). Alopecia is a loss of hair from the head or body and there are many type of hair loss with different symptoms and causes. This is a case report of a 30-year-old woman with hairless area in head. She had no families’ history of alopecia or autoimmune disease. There was no significant improvement after 1 year routine treatment for her alopecia. She had a domestic pet (Hamster) and she announced that her hamster has slept in her bedroom (her bed). We taken scales from hairless area and examined it under microscope and the hamster skin was also examined. In microscopic direct examination of her scalp observed many demodex in two species D. folliculorum and D. cricetuli and only D. cricetuli in her hamster. She was treated for demodexis and after about 2 months her hair re grown. -

ICD-10-CM TABULAR LIST of DISEASES and INJURIES
K95.09 Other complications of gastric band procedure Use additional code, if applicable, to further specify complication K95.8 Complications of other bariatric procedure Excludes1: complications of gastric band surgery (K95.0-) K95.81 Infection due to other bariatric procedure Use additional code to specify type of infection or organism, such as: bacterial and viral infectious agents (B95.-, B96.-) cellulitis of abdominal wall (L03.311) sepsis (A40.-, A41.-) K95.89 Other complications of other bariatric procedure Use additional code, if applicable, to further specify complication Chapter 12 Diseases of the skin and subcutaneous tissue (L00-L99) Excludes2: certain conditions originating in the perinatal period (P04-P96) certain infectious and parasitic diseases (A00-B99) complications of pregnancy, childbirth and the puerperium (O00-O9A) congenital malformations, deformations, and chromosomal abnormalities (Q00-Q99) endocrine, nutritional and metabolic diseases (E00-E88) lipomelanotic reticulosis (I89.8) neoplasms (C00-D49) symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (R00-R94) systemic connective tissue disorders (M30-M36) viral warts (B07.-) This chapter contains the following blocks: L00-L08 Infections of the skin and subcutaneous tissue L10-L14 Bullous disorders L20-L30 Dermatitis and eczema L40-L45 Papulosquamous disorders L49-L54 Urticaria and erythema L55-L59 Radiation-related disorders of the skin and subcutaneous tissue L60-L75 Disorders of skin appendages L76 Intraoperative and postprocedural