Jugular Phlebectasia Presenting As Globus Pharyngeus J
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Neck Dissection Using the Fascial Planes Technique
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY NECK DISSECTION USING THE FASCIAL PLANE TECHNIQUE Patrick J Bradley & Javier Gavilán The importance of identifying the presence larised in the English world in the mid-20th of metastatic neck disease with head and century by Etore Bocca, an Italian otola- neck cancer is recognised as a prominent ryngologist, and his colleagues 5. factor determining patients’ prognosis. The current available techniques to identify Fascial compartments allow the removal disease in the neck all have limitations in of cervical lymphatic tissue by separating terms of accuracy; thus, elective neck dis- and removing the fascial walls of these section is the usual choice for management “containers” along with their contents of the clinically N0 neck (cN0) when the from the underlying vascular, glandular, risk of harbouring occult regional metasta- neural, and muscular structures. sis is significant (≥20%) 1. Methods availa- ble to identify the N+ (cN+) neck include Anatomical basis imaging (CT, MRI, PET), ultrasound- guided fine needle aspiration cytology The basic understanding of fascial planes (USGFNAC), and sentinel node biopsy, in the neck is that there are two distinct and are used depending on resource fascial layers, the superficial cervical fas- availability, for the patient as well as the cia, and the deep cervical fascia (Figures local health service. In many countries, 1A-C). certainly in Africa and Asia, these facilities are not available or affordable. In such Superficial cervical fascia circumstances patients with head and neck cancer whose primary disease is being The superficial cervical fascia is a connec- treated surgically should also have the tive tissue layer lying just below the der- neck treated surgically. -

Variant Anatomy of the External Jugular Vein
ORIGINAL COMMUNICATION Anatomy Journal of Africa. 2015. 4(1): 518 – 527 VARIANT ANATOMY OF THE EXTERNAL JUGULAR VEIN Beda O. Olabu, Poonamjeet K. Loyal, Bethleen W. Matiko, Joseph M. Nderitu , Musa K. Misiani, Julius A. Ogeng’o Corresponding Author: Beda Otieno Olabu P.O.Box 30197 – 00100 GPO, Nairobi Kenya Email: [email protected] or [email protected]. Cell phone: +254 720 915 805 or +254 736 791 617 ABSTRACT Variant anatomy of the external jugular vein is important when performing invasive procedures in the neck. Although there are a number of case reports on some of these variations, there are few descriptive cross-sectional regarding the same. This study therefore aimed at describing the variant anatomy of the external jugular vein as seen in a sample Kenyan population. One hundred and six (106) sides of the neck from 53 cadaveric specimens (70 males and 36 females) in the Department of Human Anatomy, University of Nairobi, Kenya, were used. Pattern and level of formation, course, communications and termination were studied by dissection. The vein was absent in 14.2% of cases, all males. It was formed within the substance of the parotid gland in 44%, and did not receive posterior auricular vein in 6.6%. Variant communications noted included facial vein, internal jugular, and a presence of a large anastomotic vein connecting it to the anterior jugular. It was duplicated in 2.2% cases and terminated into internal jugular vein in 7.7% of cases. The most common variations were in origin, course, communications and termination. These may limit its clinical utilization, and their awareness is important when considering the vein for any invasive procedure. -

Ó Drainage of External Jugular Vein Into an Unusually Wider Internal
JKIMSU, Vol. 9, No. 3, July-September 2020 ISSN 2231-4261 CASE REPORT Drainage of External Jugular Vein into an Unusually Wider Internal Jugular Vein - A Rare Case Report Ashwija Shetty1, Suhani Sumalatha1, Sushma Prabhath1* 1Department of Anatomy, Kasturba Medical College Manipal, Manipal Academy of Higher Education, Manipal-576104 (Karnataka) India Abstract: The superficial veins are of utmost importance formed at the base of the skull by the union of the clinically for cannulation, which is required for sigmoid sinus and inferior petrosal sinus, runs diagnostic purposes and intravenous therapy. One such vertically downwards to unite with the SV and superficial vein in the neck region is the external form the brachiocephalic vein. Jugular veins are jugular vein. The other vein, deeper in this region, is among the accessible veins for various clinical the internal jugular vein. The internal jugular vein is and diagnostic approaches. IJV is one of the routes commonly used for central venous catheterization. for Central Venous Cannulation (CVC), which is Anomaly in the course and termination of both external and Internal Jugular Veins (IJV) are critical as feasible and accessible in almost all age groups. they serve as an important route/site to perform various EJV also serves as an alternate route for CVC diagnostic or therapeutic procedures. Present case especially in children in shock, dehydration and shows a rare variation of termination of the right also cardiac patients with higher rates of success external jugular vein into an unusually wider IJV. [1-2]. Variation as described in the present case, if found, EJV is an easily accessible superficial vein in the would ease the clinicians' task to approach a less neck. -

A Rare Variation of Superficial Venous Drainage Pattern of Neck Anatomy Section
ID: IJARS/2014/10764:2015 Case Report A Rare Variation of Superficial Venous Drainage Pattern of Neck Anatomy Section TANWI GHOSAL(SEN), SHABANA BEGUM, TANUSHREE ROY, INDRAJIT GUPta ABSTRACT jugular vein is very rare and is worth reporting. Knowledge Variations in the formation of veins of the head and neck of the variations of external jugular vein is not only important region are common and are well explained based on their for anatomists but also for surgeons and clinicians as the embryological background. Complete absence of an vein is frequently used for different surgical procedures and important and major vein of the region such as external for obtaining peripheral venous access as well. Keywords: Anomalies, External jugular vein, Retromandibular vein CASE REPOrt the subclavian vein after piercing the investing layer of deep During routine dissection for undergraduate students in the cervical fascia [1]. Apart from its formative tributaries, the Department of Anatomy of North Bengal Medical College, tributaries of EJV are anterior jugular vein, posterior external Darjeeling, an unusual venous drainage pattern of the head jugular vein, transverse cervical vein, suprascapular vein, and neck region was found on the right side in a middle aged sometimes occipital vein and communications with internal female cadaver. The right retromandibular vein (RMV) was jugular vein [Table/Fig-4]. formed within the parotid gland by the union of right maxillary During embryonic period, superficial head and neck veins and superficial temporal vein. The RMV which was wider than develop from superficial capillary plexuses which will later facial vein continued downwards and joined with the facial form primary head veins. -

American Academy of Otolaryngology — Head and Neck Surgery, 5
Index A lesser occipital nerve, 40 sternohyoid muscle, 39 levator scapulae muscle, 42 sternothyroid muscle, 39 American Academy of lingual artery, 47, 52 strap muscles, 37 Otolaryngology — Head and lingual nerve, 46 stylohyoid muscle, 45 Neck Surgery, 5 lingual vein, 47, 49 stylomandibular ligament, 48 American approach to neck lymphatics, 26 sublingual artery, 47 dissection, 1 deep, 26 submandibular ganglion, 48 American Society for Head and Neck deep anterior chain, 28 submandibular gland, 47 Surgery, 5 internal jugular chain, 26 submandibular nodes, 26 Anatomy jugular trunk, 28 submandibular triangle, 33, 45 ansa cervicalis, 40 left thoracic duct, 28 submental nodes, 26 anterior jugular nodes, 26 right lymphatic duct, 28 submental triangle, 33 anterior jugular vein, 36 spinal accessory chain, 28 superficial temporal artery, 52 anterior triangle, 33 superficial, 26 superior laryngeal artery, 52 ascending pharyngeal artery, 52 transverse cervical chain, 28 superior thyroid artery, 52 brachial plexus, 44 marginal nerve, 40, 48 superior thyroid veins, 49 brachiocephalic trunk, 50 mastoid nodes, 26 supraclavicular nerve, 40 carotid artery, 50 maxillary artery, 52 surgical, 35 carotid sheath, 24, 49 middle thyroid vein, 49 sympathetic trunk, 54 carotid sinus, 50 muscular triangle, 35 thyrohyoid muscle, 39 carotid triangle, 35 mylohyoid muscle, 45 thyrolinguofacial trunk, 49 cervical fascia, 23 nodal groups, 28 topographic, 33 deep, 24 disadvantages, 31 vagus nerve, 50, 53 superficial, 24 subzones, 30 Anesthesia, 64 cervical plexus, 39 occipital -
27. Veins of the Head and Neck
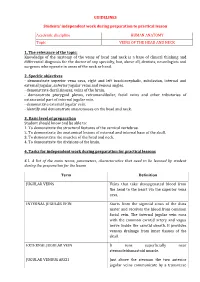
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic VEINS OF THE HEAD AND NECK 1. The relevance of the topic: Knowledge of the anatomy of the veins of head and neck is a base of clinical thinking and differential diagnosis for the doctor of any specialty, but, above all, dentists, neurologists and surgeons who operate in areas of the neck or head. 2. Specific objectives - demonstrate superior vena cava, right and left brachiocephalic, subclavian, internal and external jugular, anterior jugular veins and venous angles. - demonstrate dural sinuses, veins of the brain. - demonstrate pterygoid plexus, retromandibular, facial veins and other tributaries of extracranial part of internal jugular vein. - demonstrate external jugular vein. - identify and demonstrate anastomoses on the head and neck. 3. Basic level of preparation Student should know and be able to: 1. To demonstrate the structural features of the cervical vertebrae. 2. To demonstrate the anatomical lesions of external and internal base of the skull. 3. To demonstrate the muscles of the head and neck. 4. To demonstrate the divisions of the brain. 4. Tasks for independent work during preparation for practical lessons 4.1. A list of the main terms, parameters, characteristics that need to be learned by student during the preparation for the lesson Term Definition JUGULAR VEINS Veins that take deoxygenated blood from the head to the heart via the superior vena cava. INTERNAL JUGULAR VEIN Starts from the sigmoid sinus of the dura mater and receives the blood from common facial vein. The internal jugular vein runs with the common carotid artery and vagus nerve inside the carotid sheath. -

7. Internal Jugular Vein the Internal Jugular Vein Is a Large Vein That Receives Blood from the Brain, Face, and Neck
د.احمد فاضل Lecture 16 Anatomy The Root of the Neck The root of the neck can be defined as the area of the neck immediately above the inlet into the thorax. Muscles of the Root of the Neck Scalenus Anterior Muscle Scalenus Medius Muscle The Thoracic Duct The thoracic duct begins in the abdomen at the upper end of the cisterna chyli. It enters the thorax through the aortic opening in the diaphragm and ascends upward, inclining gradually to the left. On reaching the superior mediastinum, it is found passing upward along the left margin of the esophagus. At the root of the neck, it continues to ascend along the left margin of the esophagus until it reaches the level of the transverse process of the seventh cervical vertebra. Here, it bends laterally behind the carotid sheath. On reaching the medial border of the scalenus anterior, it turns 1 downward and drains into the beginning of the left brachiocephalic vein. It may, however, end in the terminal part of the subclavian or internal jugular veins. Main Nerves of the Neck Cervical Plexus Brachial Plexus The brachial plexus is formed in the posterior triangle of the neck by the union of the anterior rami of the 5th, 6th, 7th, and 8th cervical and the first thoracic spinal nerves. This plexus is divided into roots, trunks, divisions, and cords. The roots of C5 and 6 unite to form the upper trunk, the root of C7 continues as the middle trunk, and the roots of C8 and T1 unite to form the lower trunk. -

Unsuspected Herniated Lung Obstructing the Right Internal Jugular Vein and Internal Carotid Artery in a Patient with Thoracic Outlet Syndrome: MRI/MRA and MRV
RADIOLOGY ROUNDS Unsuspected Herniated Lung Obstructing the Right Internal Jugular Vein and Internal Carotid Artery in a Patient with Thoracic Outlet Syndrome: MRI/MRA and MRV James D. Collins, M.D. (TOS), left greater than right, and requested bilateral Abbreviations: MRI, Magnetic Resonance Imaging; MRA, Magnetic Resonance MRI/MRA and MRV of the brachial plexus to determine Angiography; MRV, Magnetic Resonance Venography; TOS, Thoracic Outlet 1 Syndrome site(s) of costoclavicular compression. Keywords: lung herniation-thoracic outlet syndrome-migraine-brachial plexus-costoclavicular compression-venous obstruction-internal jugular veins-MRI-MRA-MRV METHODS AND MATERIALS Plain chest radiographs (PA and lateral) are obtained and reviewed prior to the MRI. The procedure is discussed and Correspondence: James D. Collins, M.D., Department of Radiological Sciences, David the patient examined. Respiratory gating is applied Geffen School of Medicine at UCLA. throughout the procedure to minimize motion artifact. The Copyright ª 2016 by the National Medical Association patient is supine in the body coil, arms down to the side http://dx.doi.org/10.1016/j.jnma.2016.03.001 and imaging is monitored at the MRI station. Magnetic resonance images are obtained on the 1.5 Tesla GE Signa XL MR scanner (GE Medical Systems, Milwaukee, Wis- CLINICAL HISTORY consin). A body coil is used and no intravenous contrast 61-year-old, right-handed female complained of agents are administered. A saline water bag is placed on tingling and numbness in the ulnar aspect of the the right and the left side of the neck to increase signal to fi left hand eight weeks prior to a second orthopedic noise ratio for high-resolution imaging. -

The Carotid Endarterectomy Cadaveric Investigation for Cranial Nerve Injuries: Anatomical Study
brain sciences Article The Carotid Endarterectomy Cadaveric Investigation for Cranial Nerve Injuries: Anatomical Study Orhun Mete Cevik 1,2,3 , Murat Imre Usseli 1, Mert Babur 2, Cansu Unal 3,4, Murat Sakir Eksi 1, Mustafa Guduk 1, Talat Cem Ovalioglu 2, Mehmet Emin Aksoy 3 , M. Necmettin Pamir 1 and Baran Bozkurt 1,3,* 1 Department of Neurosurgery, Acıbadem Mehmet Ali Aydinlar University, 34662 Istanbul, Turkey; [email protected] (O.M.C.); [email protected] (M.I.U.); [email protected] (M.S.E.); [email protected] (M.G.); [email protected] (M.N.P.) 2 Department of Neurosurgery, Bakırkoy Training and Research Hospital for Psychiatric and Nervous Diseases, Health Sciences University, 34147 Istanbul, Turkey; [email protected] (M.B.); [email protected] (T.C.O.) 3 (CASE) Center of Advanced Simulation ant Education, Acıbadem Mehmet Ali Aydinlar University, 34684 Istanbul, Turkey; [email protected] (C.U.); [email protected] (M.E.A.) 4 School of Medicine, Acıbadem Mehmet Ali Aydinlar University, 34684 Istanbul, Turkey * Correspondence: [email protected]; Tel.: +90-533-315-6549 Abstract: Cerebral stroke continues to be one of the leading causes of mortality and long-term morbidity; therefore, carotid endarterectomy (CEA) remains to be a popular treatment for both symptomatic and asymptomatic patients with carotid stenosis. Cranial nerve injuries remain one of the major contributor to the postoperative morbidities. Anatomical dissections were carried out on 44 sides of 22 cadaveric heads following the classical CEA procedure to investigate the variations of the local anatomy as a contributing factor to cranial nerve injuries. -

Unusual and Multiple Variations of Head and Neck Veins: a Case Report
Surgical and Radiologic Anatomy (2019) 41:535–538 https://doi.org/10.1007/s00276-019-02203-0 ANATOMIC VARIATIONS Unusual and multiple variations of head and neck veins: a case report P. C. Vani1 · S. S. S. N. Rajasekhar1 · V. Gladwin1 Received: 14 July 2018 / Accepted: 1 February 2019 / Published online: 18 February 2019 © Springer-Verlag France SAS, part of Springer Nature 2019 Abstract We report an unusual and multiple variation involving the right head and neck veins which were found during routine dissec- tion in a 50-year-old male cadaver, facial vein draining into both external and internal jugular veins, fenestration in external jugular vein transmitting the supraclavicular nerve trunk, the anterior division of the retromandibular vein draining into anterior jugular vein and the absence of the common facial vein. The knowledge about these variations is important during various surgical and diagnostic procedures involving head and neck region. Keywords Common facial vein · External jugular vein · Facial vein · Fenestration · Retromandibular vein Introduction carotid endarterectomy [14]. The EJV has been known to have multiple uses. It is used for the insertion of temporary Head and neck region is drained by both superficial and deep hemodialysis catheter [9], as a draining site for shunt proce- veins. The superficial veins mainly receive the blood from dures involving hydrocephalus surgery [2] and as a recipi- face as well as scalp and drain into deep veins. Some of the ent vessel in head and neck reconstruction using free flap superficial veins of the head and neck region include the transfers [20]. The variations involving the FV is important facial vein (FV), retromandibular vein (RMV), anterior jugu- during reconstructive surgeries and knowledge about these lar vein (AJV) and external jugular vein (EJV). -
Review of the Variations of the Superficial Veins of the Neck
Open Access Review Article DOI: 10.7759/cureus.2826 Review of the Variations of the Superficial Veins of the Neck Dominic Dalip 1 , Joe Iwanaga 1 , Marios Loukas 2 , Rod J. Oskouian 3 , R. Shane Tubbs 4 1. Seattle Science Foundation, Seattle, USA 2. Anatomical Sciences, St. George's University, St. George's, GRD 3. Neurosurgery, Swedish Neuroscience Institute, Seattle, USA 4. Neurosurgery, Seattle Science Foundation, Seattle, USA Corresponding author: Joe Iwanaga, [email protected] Abstract The venous drainage of the neck can be characterized into superficial or deep. Superficial drainage refers to the venous drainage of the subcutaneous tissues, which are drained by the anterior and external jugular veins (EJVs). The brain, face, and neck structures are mainly drained by the internal jugular vein (IJV). The superficial veins are found deep to the platysma muscle while the deep veins are found encased in the carotid sheath. The junction of the retromandibular vein and the posterior auricular vein usually form the EJV, which continues along to drain into the subclavian vein. The anterior jugular vein is usually formed by the submandibular veins, travels downward anterior to the sternocleidomastoid muscle (SCM), and drains either into the EJV or the subclavian vein. Other superficial veins of the neck to consider are the superior, middle, and inferior thyroid veins. The superior thyroid and middle thyroid veins drain into the IJV whereas the inferior thyroid vein usually drains into the brachiocephalic veins. Categories: Miscellaneous Keywords: external jugular, vein, superficial, internal jugular, thyroid vein Introduction And Background The external jugular vein (EJV) is the preferred vein when performing a central venous catheterization. -

Multiple Variations of the Superficial Jugular Veins: Case Report and Clinical Relevance
CASE REPORT MULTIPLE VARIATIONS OF THE SUPERFICIAL JUGULAR VEINS: CASE REPORT AND CLINICAL RELEVANCE George Paraskevas¹, Konstantinos Natsis¹, Orestis Ioannidis¹, Panagiotis Kitsoulis², Nikolaos Anastasopoulos1, Ioannis Spyridakis1 Department of Anatomy, Faculty of Medicine, Aristotle University of Thessaloniki, Thessaloniki, Greece¹; Department of Anatomy, Histology and Embryology, Faculty of Medicine, University of Ioannina, Ioannina, Greece² Summary: The jugular venous system constitutes the primary venous drainage of the head and neck. It includes a profundus or subfascial venous system, formed by the two internal jugular veins, and a superficial or subcutaneous one, formed by the two anterior and two external jugular veins. We report one case of unilateral anatomical variations of the external and anterior jugular veins. Particularly, on the right side, three external jugular veins co-existed with two anterior jugular veins. Such a combination of venous anomalies is extremely rare. The awareness of the variability of these veins is essential to anesthesiologists and radiologists, since the external jugular vein constitutes a common route for catheterization. Their knowledge is also important to surgeons performing head and neck surgery. Keywords: External jugular vein; Anterior jugular vein; Multiple veins Introduction Case report The veins of the neck are expanded as two separate ve- In a male embalmed cadaver aged 63 years old that nous systems, the superficial or subcutaneous comprised the has been used for educational and research purposes in anterior and external jugular veins draining mostly the sub- the Department of Anatomy at the Faculty of Medicine cutaneous tissues and the deep veins comprised the internal of the Aristotle University of Thessaloniki and after care- jugular veins draining mainly the brain and other structures ful preparation of the anterior and lateral cervical region of face and neck (27).