Effects of Anti Depressants on Our Sleep
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
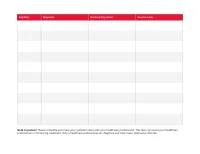
Print Your Symptom Diary
MEDICATION GUIDE FETZIMA® (fet-ZEE-muh) (levomilnacipran) extended-release capsules, for oral use What is the most important information I should know about FETZIMA? FETZIMA may cause serious side effects, including: • Increased risk of suicidal thoughts or actions in some children, adolescents, and young adults. FETZIMA and other antidepressant medicines may increase suicidal thoughts or actions in some children and young adults, especially within the first few months of treatment or when the dose is changed. FETZIMA is not for use in children. o Depression or other serious mental illnesses are the most important causes of suicidal thoughts or actions. Some people may have a higher risk of having suicidal thoughts or actions. These include people who have (or have a family history of) depression, bipolar illness (also called manic-depressive illness) or have a history of suicidal thoughts or actions. How can I watch for and try to prevent suicidal thoughts and actions? o Pay close attention to any changes, especially sudden changes in mood, behavior, thoughts, or feelings, or if you develop suicidal thoughts or actions. This is very important when an antidepressant medicine is started or when the dose is changed. o Call your healthcare provider right away to report new or sudden changes in mood, behavior, thoughts, or feelings. o Keep all follow-up visits with your healthcare provider as scheduled. Call your healthcare provider between visits as needed, especially if you have concerns about symptoms. Call your healthcare provider or -

Levomilnacipran (Fetzima®) Indication
Levomilnacipran (Fetzima®) Indication: Indicated for the treatment of major depressive disorder (MDD), FDA approved July 2013. Mechanism of action Levomilnacipran, the more active enantiomer of racemic milnacipran, is a selective SNRI with greater potency for inhibition of norepinephrine relative to serotonin reuptake Compared with duloxetine or venlafaxine, levomilnacipran has over 10-fold higher selectivity for norepinephrine relative to serotonin reuptake inhibition The exact mechanism of the antidepressant action of levomilnacipran is unknown Dosage and administration Initial: 20 mg once daily for 2 days and then increased to 40 mg once daily. The dosage can be increased by increments of 40 mg at intervals of two or more days Maintenance: 40-120 mg once daily with or without food. Fetzima should be swallowed whole (capsule should not be opened or crushed) Levomilnacipran and its metabolites are eliminated primarily by renal excretion o Renal impairment Dosing: Clcr 30-59 mL/minute: 80 mg once daily Clcr 15-29 mL/minute: 40 mg once daily End-stage renal disease (ESRD): Not recommended Discontinuing treatment: Gradually taper dose, if intolerable withdrawal symptoms occur, consider resuming the previous dose and/or decrease dose at a more gradual rate How supplied: Capsule ER 24 Hour Fetzima Titration: 20 & 40 mg (28 ea) Fetzima: 20 mg, 40 mg, 80 mg, 120 mg Warnings and Precautions Elevated Blood Pressure and Heart Rate: measure heart rate and blood pressure prior to initiating treatment and periodically throughout treatment Narrow-angle glaucoma: may cause mydriasis. Use caution in patients with controlled narrow- angle glaucoma Urinary hesitancy or retention: advise patient to report symptoms of urinary difficulty Discontinuation Syndrome Seizure disorders: Use caution with a previous seizure disorder (not systematically evaluated) Risk of Serotonin syndrome when taken alone or co-administered with other serotonergic agents (including triptans, tricyclics, fentanyl, lithium, tramadol, tryptophan, buspirone, and St. -

Levomilnacipran for the Treatment of Major Depressive Disorder
Out of the Pipeline Levomilnacipran for the treatment of major depressive disorder Matthew Macaluso, DO, Hala Kazanchi, MD, and Vikram Malhotra, MD An SNRI with n July 2013, the FDA approved levomil- Table 1 once-daily dosing, nacipran for the treatment of major de- Levomilnacipran: Fast facts levomilnacipran pressive disorder (MDD) in adults.1 It is I Brand name: Fetzima decreased core available in a once-daily, extended-release formulation (Table 1).1 The drug is the fifth Class: Serotonin-norepinephrine reuptake symptoms of inhibitor serotonin-norepinephrine reuptake inhibi- MDD and was well Indication: Treatment of major depressive tor (SNRI) to be sold in the United States disorder in adults tolerated in clinical and the fourth to receive FDA approval for FDA approval date: July 26, 2013 trials treating MDD. Availability date: Fourth quarter of 2013 Levomilnacipran is believed to be the Manufacturer: Forest Pharmaceuticals more active enantiomer of milnacipran, Dosage forms: Extended–release capsules in which has been available in Europe for 20 mg, 40 mg, 80 mg, and 120 mg strengths years and was approved by the FDA in Recommended dosage: 40 mg to 120 mg 2009 for treating fibromyalgia. Efficacy of capsule once daily with or without food levomilnacipran for treating patients with Source: Reference 1 MDD was established in three 8-week ran- domized controlled trials (RCTs).1 cial and occupational functioning in addi- Clinical implications tion to improvement in the core symptoms Levomilnacipran is indicated for treating of depression.5 -

Premium Non-Specialty Quantity Limit List January 2016
Premium Non-Specialty Quantity Limit List January 2016 Therapeutic Category Drug Name Dispensing Limit Anti-infectives Antibiotics DIFICID (fidaxomicin) 200 mg 2 tabs/day & 10 days/30 days SIVEXTRO (tedizolid) Solr 6 vials/30 days SIVEXTRO (tedizolid) Tabs 6 tabs/30 days ZYVOX (linezolid) 28 tabs/30 days ZYVOX (linezolid) Suspension 4 bottles (600 mL)/28 days Antifungals LAMISIL (terbinafine) 250 mg 84 days supply/180 days Antimalarial QUALAQUIN (quinine) QL varies* Antivirals, Herpetic FAMVIR (famciclovir) 125 mg 1 tab/day FAMVIR (famciclovir) 250 mg 2 tabs/day FAMVIR (famciclovir) 500 mg 21 tabs/30 days SITAVIG (acyclovir) 50 mg 2 tabs/30 days VALTREX (valacyclovir) 1000 mg 3 tabs/day VALTREX (valacyclovir) 500 mg 2 tabs/day Antivirals, Influenza RELENZA (zanamivir) QL is 40 inh per 365 days. TAMIFLU (oseltamivir) 30 mg 40 caps per 365 days TAMIFLU (oseltamivir) 45 mg, 75 mg 20 caps per 365 days TAMIFLU (oseltamivir) Suspension 360 mL/365 days Cardiology Anticoagulants ELIQUIS (apixiban) 2 tabs/day ELIQUIS (apixiban) 5 mg 3 tabs/day IPRIVASK (desirudin) 35 days supply/180 days PRADAXA (dabigatran) 2 caps/day SAVAYSA (edoxaban) 1 tab/day XARELTO (rivaroxaban) 10 mg 35 days supply/180 days XARELTO (rivaroxaban) 15 mg 2 tabs/day XARELTO (rivaroxaban) 20 mg 1 tab/day XARELTO (rivaroxaban) Starter Pack 2 starter packs/year Heart Failure CORLANOR (ivabradine) 2 tabs/day Central Nervous System ADHD Agents ADDERALL (amphetamine/dextroamphetamine) 3 tabs/day ADDERALL XR (amphetamine/dextroamphetamine mixed salts) 1 cap/day APTENSIO XR (methylphenidate) -

Pristiq (Desvenlafaxine Succinate) – First-Time Generic
Pristiq® (desvenlafaxine succinate) – First-time generic • On March 1, 2017, Teva launched AB-rated generic versions of Pfizer’s Pristiq (desvenlafaxine succinate) 25 mg, 50 mg, and 100 mg extended-release tablets for the treatment of major depressive disorder. — Teva launched the 25 mg tablet with 180-day exclusivity. — In addition, Alembic/Breckenridge, Mylan, and West-Ward have launched AB-rated generic versions of Pristiq 50 mg and 100 mg extended-release tablets. — Greenstone’s launch plans for authorized generic versions of Pristiq 25 mg, 50 mg, and 100 mg tablets are pending. — Lupin and Sandoz received FDA approval of AB-rated generic versions of Pristiq 50 mg and 100 mg tablets on June 29, 2015. Lupin’s and Sandoz’s launch plans are pending. • Other serotonin-norepinephrine reuptake inhibitors approved for the treatment of major depressive disorder include desvenlafaxine fumarate, duloxetine, Fetzima™ (levomilnacipran), Khedezla™ (desvenlafaxine) , venlafaxine, and venlafaxine extended-release. • Pristiq and the other serotonin-norepinephrine reuptake inhibitors carry a boxed warning for suicidal thoughts and behaviors. • According to IMS Health data, the U.S. sales of Pristiq were approximately $883 million for the 12 months ending on December 31, 2016. optumrx.com OptumRx® specializes in the delivery, clinical management and affordability of prescription medications and consumer health products. We are an Optum® company — a leading provider of integrated health services. Learn more at optum.com. All Optum® trademarks and logos are owned by Optum, Inc. All other brand or product names are trademarks or registered marks of their respective owners. This document contains information that is considered proprietary to OptumRx and should not be reproduced without the express written consent of OptumRx. -

A Brief Overview of Psychiatric Pharmacotherapy
A Brief Overview of Psychiatric Pharmacotherapy Joel V. Oberstar, M.D. Chief Executive Officer Disclosures • Some medications discussed are not approved by the FDA for use in the population discussed/described. • Some medications discussed are not approved by the FDA for use in the manner discussed/described. • Co-Owner: – PrairieCare and PrairieCare Medical Group – Catch LLC Disclaimer The contents of this handout are for informational purposes only and are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical or psychiatric condition. Never disregard professional/medical advice or delay in seeking it because of something you have read in this handout. Material in this handout may be copyrighted by the author or by third parties; reasonable efforts have been made to give attribution where appropriate. Caveat Regarding the Role of Medication… Neuroscience Overview Mind Over Matter, National Institute on Drug Abuse, National Institutes of Health. Available at: http://teens.drugabuse.gov/mom/index.asp. http://medicineworld.org/images/news-blogs/brain-700997.jpg Neuroscience Overview Mind Over Matter, National Institute on Drug Abuse, National Institutes of Health. Available at: http://teens.drugabuse.gov/mom/index.asp. Neurotransmitter Receptor Source: National Institute on Drug Abuse Common Diagnoses and Associated Medications • Psychotic Disorders – Antipsychotics • Bipolar Disorders – Mood Stabilizers, Antipsychotics, & Antidepressants • Depressive Disorders – Antidepressants • Anxiety Disorders – Antidepressants & Anxiolytics • Attention Deficit Hyperactivity Disorder – Stimulants, Antidepressants, 2-Adrenergic Agents, & Strattera Classes of Medications • Anti-depressants • Stimulants and non-stimulant alternatives • Anti-psychotics (a.k.a. -

Levomilnacipran (Fetzima) for Major Depressive Disorder SAMIRA ZAMAN, MD, and MAURA R
STEPS New Drug Reviews Levomilnacipran (Fetzima) for Major Depressive Disorder SAMIRA ZAMAN, MD, and MAURA R. MCLAUGHLIN, MD, University of Virginia Health System, Charlottesville, Virginia STEPS new drug reviews Levomilnacipran (Fetzima) is a serotonin-norepinephrine reuptake inhibitor (SNRI) labeled cover Safety, Tolerability, for the treatment of major depressive disorder in adults.1 Effectiveness, Price, and Simplicity. Each indepen- dent review is provided by authors who have no Drug Dosage Dose form Cost* financial association with Levomilnacipran 20 mg per day for two days, 20-, 40-, 80-, $286 for 30 capsules (prices the drug manufacturer. (Fetzima) then increases to 40 mg and 120-mg are identical for 20-,40-, This series is coordinated per day (maximum = 120 capsules 80-, and 120-mg capsules) by Allen F. Shaughnessy, mg per day) PharmD, MMedEd, Con- tributing Editor. *—Estimated retail price of one month’s treatment based on information obtained at http://www.goodrx.com (accessed August 19, 2015). A collection of STEPS pub- lished in AFP is available at http://www.aafp.org/ afp/steps. SAFETY when used concurrently with a cytochrome Levomilnacipran causes few serious adverse P450 3A4 inhibitor because levomilnaci- effects, although long-term safety has not pran is partially metabolized by the liver, been established.2 As with all antidepres- and medications that inhibit the cytochrome sants, levomilnacipran carries a warning P450 3A4 system, such as ketoconazole, may of increased risk of suicidal thoughts and cause it to accumulate.1 Patients with moder- behavior in patients 24 years or younger, and ate and severe renal impairment should be it has not been studied in patients younger limited to a dosage of 80 mg per day and 40 than 18 years.1 Levomilnacipran increases mg per day, respectively. -

Pharmacokinetic and Pharmacodynamic Interactions Between Antiepileptics and Antidepressants Domenico Italiano University of Messina, Italy
University of Kentucky UKnowledge Psychiatry Faculty Publications Psychiatry 11-2014 Pharmacokinetic and Pharmacodynamic Interactions between Antiepileptics and Antidepressants Domenico Italiano University of Messina, Italy Edoardo Spina University of Messina, Italy Jose de Leon University of Kentucky, [email protected] Right click to open a feedback form in a new tab to let us know how this document benefits oy u. Follow this and additional works at: https://uknowledge.uky.edu/psychiatry_facpub Part of the Psychiatry and Psychology Commons Repository Citation Italiano, Domenico; Spina, Edoardo; and de Leon, Jose, "Pharmacokinetic and Pharmacodynamic Interactions between Antiepileptics and Antidepressants" (2014). Psychiatry Faculty Publications. 40. https://uknowledge.uky.edu/psychiatry_facpub/40 This Article is brought to you for free and open access by the Psychiatry at UKnowledge. It has been accepted for inclusion in Psychiatry Faculty Publications by an authorized administrator of UKnowledge. For more information, please contact [email protected]. Pharmacokinetic and Pharmacodynamic Interactions between Antiepileptics and Antidepressants Notes/Citation Information Published in Expert Opinion on Drug Metabolism & Toxicology, v. 10, Issue 11, p. 1457-1489. © 2014 Taylor & Francis Group This is an Accepted Manuscript of an article published by Taylor & Francis Group in Expert Opinion on Drug Metabolism & Toxicology in Nov. 2014, available online: http://www.tandfonline.com/10.1517/ 17425255.2014.956081 Digital Object Identifier (DOI) http://dx.doi.org/10.1517/17425255.2014.956081 This article is available at UKnowledge: https://uknowledge.uky.edu/psychiatry_facpub/40 1 This is an Accepted Manuscript of an article published by Taylor & Francis Group in Expert Opinion on Drug Metabolism & Toxicology in Nov. -
Prescriber's Guide to Using 3 New Antidepressants W
VILAZODONE • LEVOMILNACIPRAN • VORTIOXETINE Prescriber’s guide to using 3 new antidepressants How do they work? What makes them different? And which patients might benefit most from taking them? Ahmed Z. Elmaadawi, MD Narendra Singh, MD ith a prevalence >17%, depression is one of the most common Jagadeesh Reddy, MD, MPH mental disorders in the United States and the second leading Adjunct Clinical Assistant Professors W 1,2 cause of disability worldwide. For decades, primary care and mental Suhayl Joseph Nasr, MD health providers have used selective serotonin reuptake inhibitors (SSRIs) Volunteer Clinical Professor as first-line treatment for depression—yet the remission rate after the first Department of Psychiatry trial of an antidepressant is <30%, and continues to decline after a first Indiana University School of Medicine- antidepressant failure.3 South Bend Campus South Bend, Indiana That is why clinicians continue to seek effective treatments for depres- sion—ones that will provide quick and sustainable remission—and why Disclosures Drs. Elmaadawi, Singh, and Reddy report no financial scientists and pharmaceutical manufacturers have been competing to relationships with any company whose products develop more effective antidepressant medications. are mentioned in this article or with manufacturers of competing products. Dr. Nasr is a member of the In the past 4 years, the FDA has approved 3 antidepressants— speakers’ bureau for Forest Pharmaceuticals and Takeda vilazodone, levomilnacipran, and vortioxetine—with the hope of Pharmaceutical Company Limited and H. Lundbeck A/S. increasing options for patients who suffer from major depression. These 3 antidepressants differ in their mechanisms of action from other available antidepressants, and all have been shown to have acceptable safety and tolerability profiles. -

STEP THERAPY CRITERIA BRAND NAME (Generic) (Desvenlafaxine Fumarate Extended-Release Tablets)
STEP THERAPY CRITERIA BRAND NAME (generic) (desvenlafaxine fumarate extended-release tablets) FETZIMA (levomilnacipran) KHEDEZLA (desvenlafaxine extended release tablets) PRISTIQ (desvenlafaxine succinate extended release tablets) Status: CVS Caremark Criteria Type: Initial Step Therapy; Post Step Therapy Prior Authorization with Limit POLICY FDA-APPROVED INDICATIONS Desvenlafaxine Desvenlafaxine, a serotonin and norepinephrine reuptake inhibitor (SNRI), is indicated for the treatment of major depressive disorder (MDD). The efficacy of desvenlafaxine has been established in four short-term (8-week, placebo- controlled studies) of outpatients who met DSM-IV criteria for major depressive disorder. Fetzima Fetzima, a serotonin and norepinephrine reuptake inhibitor (SNRI) is indicated for the treatment of major depressive disorder (MDD). The efficacy of Fetzima was established in three 8-week, randomized, double-blind, placebo-controlled studies in adult patients with a diagnosis of MDD Limitation of Use: Fetzima is not approved for the management of fibromyalgia. The efficacy and safety of Fetzima for the management of fibromyalgia have not been established. Khedezla Khedezla, a serotonin and norepinephrine reuptake inhibitor (SNRI), is indicated for the treatment of major depressive disorder (MDD). The efficacy of desvenlafaxine has been established in four short-term (8-week, placebo-controlled studies) in adult outpatients who met DSM-IV criteria for major depressive disorder. Pristiq Pristiq is indicated for the treatment of adults with -

Antidepressants for Major Depressive Disorder: Drug Information to Support Drug Therapy Decisions
Antidepressants for Major Depressive Disorder: Drug Information to Support Drug Therapy Decisions B.C. Provincial Academic Detailing (PAD) Service March 2020 Background This PAD education session focuses on commonly prescribed and recently marketed antidepressants for major depressive disorder. After achieving remission of an initial depressive episode, clinical practice guidelines recommend several months of continued antidepressant therapy (recommendations vary from 4 to 12 months) and longer if someone is at risk for relapse or has experienced recurrent episodes.1-6 A recent primary care trial found that discontinuing antidepressant therapy can be challenging even for people considered candidates for discontinuation according to guidelines.7 51% of people in the trial agreed to try a taper to discontinue their antidepressant therapy when provided with the recommendation from their primary care physician. Ten of 146 people considered eligible for antidepressant discontinuation were no longer taking an antidepressant at the end of follow up. Acknowledging that the most appropriate duration of antidepressant therapy is not known,8 participants in this PAD session will have the opportunity to discuss drug information that informs several decisions regarding antidepressants for non-pregnant adults, including: 1. How the efficacy of antidepressants is Antidepressant Brand Name Marketed9 measured in clinical trials and reported in meta-analyses Fluoxetine Prozac 1989 Sertraline Zoloft 1992 2. The quality and quantity of evidence that informs conclusions regarding Paroxetine Paxil 1993 antidepressant comparisons and Venlafaxine Effexor 1994 combinations Bupropion Wellbutrin 1998 3. Drug information relevant to the Citalopram Celexa 1999 prescribing, deprescribing and monitoring Mirtazapine Remeron 2001 of antidepressants, including: Escitalopram Cipralex 2005 . dose response Duloxetine Cymbalta 2008 . -

Safety of 80 Antidepressants, Antipsychotics, Anti‐Attention‐Deficit/Hyperactivity Medications and Mood Stabilizers in Child
RESEARCH REPORT Safety of 80 antidepressants, antipsychotics, anti-attention-deficit/ hyperactivity medications and mood stabilizers in children and adolescents with psychiatric disorders: a large scale systematic meta-review of 78 adverse effects Marco Solmi1-3, Michele Fornaro4, Edoardo G. Ostinelli5,6, Caroline Zangani6, Giovanni Croatto1, Francesco Monaco7, Damir Krinitski8, Paolo Fusar-Poli3,9-11, Christoph U. Correll12-15 1Neurosciences Department, University of Padua, Padua, Italy; 2Padua Neuroscience Center, University of Padua, Padua, Italy; 3Early Psychosis: Interventions and Clinical- detection (EPIC) lab, Department of Psychosis Studies, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London, UK; 4Department of Psychiatry, Federico II University, Naples, Italy; 5Oxford Health NHS Foundation Trust, Warneford Hospital, and Department of Psychiatry, University of Oxford, Oxford, UK; 6Depart- ment of Health Sciences, University of Milan, Milan, Italy; 7Department of Mental Health, ASL Salerno, Salerno, Italy; 8Integrated Psychiatry Winterthur (IPW), Winterthur, Switzerland; 9OASIS Service, South London & Maudsley NHS Foundation Trust, London, UK; 10Department of Brain and Behavioral Sciences, University of Pavia, Pavia, Italy; 11National Institute for Health Research, Maudsley Biomedical Research Centre, South London & Maudsley NHS Foundation Trust, London, UK; 12Department of Psychiatry, Zucker Hillside Hospital, Northwell Health, Glen Oaks, New York, NY, USA; 13Department of Psychiatry and Molecular Medicine, Zucker School of Medicine at Hofstra/Northwell, Hempstead, NY, USA; 14Center for Psychiatric Neuroscience, Feinstein Institute for Medical Research, Manhasset, NY, USA; 15Department of Child and Adolescent Psychiatry, Charité Universitätsmedizin Berlin, Berlin, Germany Mental disorders frequently begin in childhood or adolescence. Psychotropic medications have various indications for the treatment of mental dis orders in this age group and are used not infrequently offlabel.