Coding and Reimbursement Primer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Practice Guideline for Limb Salvage Or Early Amputation
Limb Salvage or Early Amputation Evidence-Based Clinical Practice Guideline Adopted by: The American Academy of Orthopaedic Surgeons Board of Directors December 6, 2019 Endorsed by: Please cite this guideline as: American Academy of Orthopaedic Surgeons. Limb Salvage or Early Amputation Evidence-Based Clinical Practice Guideline. https://www.aaos.org/globalassets/quality-and-practice-resources/dod/ lsa-cpg-final-draft-12-10-19.pdf Published December 6, 2019 View background material via the LSA CPG eAppendix Disclaimer This clinical practice guideline was developed by a physician volunteer clinical practice guideline development group based on a formal systematic review of the available scientific and clinical information and accepted approaches to treatment and/or diagnosis. This clinical practice guideline is not intended to be a fixed protocol, as some patients may require more or less treatment or different means of diagnosis. Clinical patients may not necessarily be the same as those found in a clinical trial. Patient care and treatment should always be based on a clinician’s independent medical judgment, given the individual patient’s specific clinical circumstances. Disclosure Requirement In accordance with AAOS policy, all individuals whose names appear as authors or contributors to this clinical practice guideline filed a disclosure statement as part of the submission process. All panel members provided full disclosure of potential conflicts of interest prior to voting on the recommendations contained within this clinical practice guideline. Funding Source This clinical practice guideline was funded exclusively through a research grant provided by the United States Department of Defense with no funding from outside commercial sources to support the development of this document. -

CPT® New Codes 2019: Biopsy, Skin
Billing and Coding Update Alexander Miller, M.D. AAD Representative to the AMA CPT Advisory Committee New Skin Biopsy CPT® Codes It’s all about the Technique! SPEAKER: Alexander Miller, M.D. AAD Representative to the AMA -CPT Advisory Committee Chair AAD Health Care Finance Committee Arriving on January 1, 2019 New and Restructured Biopsy Codes Tangential biopsy Punch Biopsy Incisional Biopsy How Did We Get Here? CMS CY 2016 Biopsy codes (11100, 11101 identified as potentially mis-valued; high expenditure RUC Survey sent to AAD Members Specialty survey results are the only tool available to support code values Challenging survey results Survey revealed bimodal data distribution; CPT Codes 11100, 11101 referred to CPT for respondents were valuing different procedures restructuring Rationale for New Codes 11100; 11101 • Previous skin biopsy codes did not distinguish between the different biopsy techniques that were being used CPT Recommended technique specification in new biopsy codes • Will also provide for reimbursement commensurate with the technique used How Did We Get Here? • CPT Editorial Panel deleted 11100; 11101 February 2017 • 6 New codes created based on technique utilized • Each technique: primary code and add-on code March 2017 • RUC survey sent to AAD members April 2017 • Survey results presented to the RUC Biopsy Codes Effective Jan., 1, 2019 • Integumentary biopsy codes 11755 Biopsy of nail unit (plate, bed, matrix, hyponychium, proximal and lateral nail folds 11100, 11101 have been deleted 30100 Biopsy, intranasal • New -

Transplantation and Hepatic Pathology University of Pittsburgh Medical Center November, 2007
Resident Handbook Division of Transplantation and Hepatic Pathology University of Pittsburgh Medical Center November, 2007 For private use of residents only- not for public distribution Table of Contents Anatomic Transplantation Pathology Rotation Clinical Responsibilities of the Division ........................................................3 Categorizations of Specimens and Structure of Signout.................................3 Resident Responsibilities................................................................................4 Learning Resources.........................................................................................4 Transplantation Pathology on the World-Wide Web......................................4 Weekly Schedule ............................................................................................6 Staff Locations and Telephone Numbers........................................................7 Background Articles Landmarks in Transplantation ........................................................................8 Trends in Organ Donation and Transplantation US 1996-2005.....................18 Perspectives in Organ Preservation………....................................................26 Transplant Tolerance- Editorial……………………………………….…….36 Kidney Grading Systems Banff 2005 Update……………………….....................................................42 Banff 97 Components (I t v g etc.) ................................................................44 Readings Banff 05 Meeting Report………………………………………...................47 -
Msc Payment Schedule Index
MSC PAYMENT SCHEDULE INDEX SECTIONS (To go directly to the an applicable section of the Payment Schedule, click on the Section heading listed below) GENERAL PREAMBLE TO THE PAYMENT SCHEDULE .................................. 1 2. OUT-OF-OFFICE HOURS PREMIUMS ............................................................... 2 3. GENERAL SERVICES ......................................................................................... 3 4. DIAGNOSTIC AND SELECTED THERAPEUTIC PROCEDURES ...................... 4 5. CRITICAL CARE .................................................................................................. 5 6. EMERGENCY MEDICINE .................................................................................... 6 7. GENERAL PRACTICE ......................................................................................... 7 8. ANESTHESIA ...................................................................................................... 8 9. DERMATOLOGY ................................................................................................. 9 10. OPHTHALMOLOGY .......................................................................................... 10 11. OTOLARYNGOLOGY ........................................................................................ 11 12. GENERAL INTERNAL MEDICINE .................................................................... 12 13. CARDIOLOGY ................................................................................................... 13 14. CLINICAL IMMUNOLOGY AND ALLERGY -
15-Coned-Ccrn-Cardiovascular.Pdf
1 Cardiovascular Introduction A. Anatomy & Physiology B. Cardiac Assessment 1. Cardiac Risk Factors Non Modifiable Age Gender Family History Race Modifiable Smoking Hypertension Diabetes Obesity Stress Exercise Hyperlipidemia 2. Medical & Surgical History 3. Social History 4. Medication History 5. Physical Exam 2 Color Pulses Rate & Rhythm PMI Location Extremity Temperature Dyspnea Fatigue Level Fluid Retention Palpitations Dizziness 6. Chest Pain Exam PQRST Assessment P: Pain, Placement, Provocation Q: Quality (sharp, stabbing, pressure) , Quantity R: Radiation, Relief S: Severity, Systems (nausea, sweaty, dizziness) T: Timing (when it started, how long did it last, what makes it better or worse) C. Diagnostic Tests & Procedures 1. 12 Lead ECG 2. Echocardiography (Transthoracic and Transesepheal) 3. Stress Test 4. Cardiac Catheterization 5. Doppler Ultrasound 6. Blood Work Acute Coronary Syndrome Cardiac Enzymes: CK-MB, Amino Acids: Troponins Heme Proteins: Myoglobin Lipid Profile Triglycerides Cholesterol Low Density Lipoproteins High Density Lipoprotein Coagulation Profile PT/INR aPTT ACT 3 Misc B Type Naturetic Peptide – BNP C Reactive Protein Homocysteine Hemodynamic Monitoring/Assessment CARDIAC OUTPUT HEART RATE X STROKE VOLUME PRELOAD + AFTERLOAD + CONTRACTILITY + The volume of blood in the The pressure or resistance the LV must contract The ability of the against or overcome to eject the blood or create ventricle at end diastole. systole. myocardium to contract. Total Blood Volume -

Skin Grafts in Cutaneous Oncology* Enxertia De Pele Em Oncologia
RevABDV81N5.qxd 07.11.06 17:07 Page 465 465 Artigo de Revisão Enxertia de pele em oncologia cutânea* Skin grafts in cutaneous oncology* José Anselmo Lofêgo Filho1 Paula Dadalti2 Diogo Cotrim de Souza3 Paulo Roberto Cotrim de Souza4 Marcos Aurélio Leiros da Silva5 Cristina Maeda Takiya6 Resumo: Em oncologia cutânea depara-se freqüentemente com situações em que a confec- ção de um enxerto é uma boa alternativa para o fechamento do defeito cirúrgico. Conhecer aspectos referentes à integração e contração dos enxertos é fundamental para que os cirur- giões dermatológicos procedam de maneira a não contrariar princípios básicos do trans- plante de pele. Os autores fazem uma revisão da classificação e fisiologia dos enxertos de pele, acrescendo considerações cirúrgicas determinantes para o sucesso do procedimento. Palavras-chave: Neoplasias cutâneas; Transplante de pele; Transplante homólogo Abstract: In cutaneous oncology, there are many situations in which skin grafts could be a good alternative for closing surgical defect. Dermatological surgeons should have enough knowledge about graft integration and contraction in order to not contradict the basic prin- ciples of skin transplantation. The authors review skin graft classification and physiology and make some surgical considerations on successful procedures. Keywords: Skin neoplasms; Skin transplantation; Transplantation, homologous INTRODUÇÃO Enxerto é parte de um tecido vivo transplanta- tológica. São simples quando apresentam um único do de um lugar para outro no mesmo organismo ou tipo de tecido e compostos quando constituídos de em organismos distintos.1 Contudo, a utilização da dois ou mais tipos de tecidos. Em oncologia cutânea, terminologia enxerto para designar uma modalidade um enxerto composto é usado quando o defeito cirúrgica, apesar de errônea, tornou-se coloquial. -

Culdocentesis in Diagnosis of Disturbed Ectopic Pregnancy Still a Useful Procedure in Developing Countries
CULDOCENTESIS IN DIAGNOSIS OF DISTURBED ECTOPIC PREGNANCY STILL A USEFUL PROCEDURE IN DEVELOPING COUNTRIES Pages with reference to book, From 5 To 6 Tasneem Aslam Tariq ( Department of Obstetrics and Gynaecology, Jinnah Postgraduate Medical Centre, Karachi. ) Razia Korejo ( Department of Obstetrics and Gynaecology, Jinnah Postgraduate Medical Centre, Karachi. ) ABSTRACT Over a period of 5 years culdocentesis was carried out in 156 cases of suspected ectopic pregnancy using needle aspiration through the pouch of Douglas. The result was positive in 134 cases, with 131 being true positive and 3 false positive. In 22 cases the result was negative, 6 of which were false negative. It is concluded that culdocentesis is an effective method of diagnosing disturbed ectopic pregnancy (JPMA 42: 5, 1992). INTRODUCTION Ectopic pregnancy, a clinical diagnosis in majority of cases is infrequently seen in our hospital. Since it can present with varied symptoms, diagnosis can be difficult in some cases. To increase the accuracy rate of preoperative diagnosis in suspected cases of ectopic pregnancy, various diagnostic procedures have been employed over the years. The purpose of this study was to evaluate the efficacy of culdocentesis for the diagnosis of ectopic pregnancy. PATIENTS AND METHOD The present study included 156 suspected cases of ectopic pregnancy admitted to the Department of Obstetrics and Gynaecology between January, 1985 to December 1989. Culdocentesis was done in the operating theatre under aseptic precautions with or without general anaesthesia depending on the certainty of the diagnosis. Urinary bladder was catheterized and gentle bimanual vaginal examination was done to confirm the previous vaginal findings. Sims speculum was introduced in the vagina and posterior lip of cervix was held gently with a Vulsellum forceps, pulled upwards and forwards exposing the posterior fornix. -

Women's Health Course Guide
Course Guide for Women’s Health 1 Approach to the Patient The OB/GYN History Rationale: A gynecological evaluation is an important part of primary health care and preventive medicine for women. A gynecological assessment should be a part of every woman’s general medical history and physical examination. Certain questions must be asked of every woman, whereas other questions are specific to particular problems. To accomplish these objectives, optimal communication must be achieved between patient and physician. The student will demonstrate the ability to: A. Perform a thorough obstetric-gynecologic history as a portion of a general medical history, including: 1. Chief complaint 2. Present illness 3. Menstrual history 4. Obstetric history 5. Gynecologic history 6. Contraceptive history 7. Sexual history 8. Family history 9. Social history B. Interact with the patient to gain her confidence and to develop an appreciation of the effect of her age, racial and cultural background, and economic status on her health; C. Communicate the results of the obstetric-gynecologic and general medical history by well-organized written and oral reports. The OB/GYN Examination Rationale: An accurate examination complements the history, provides additional information and helps determine diagnosis and guide management. It also provides an opportunity to educate and reassure the patient. The student will demonstrate the ability to: A. Interact with the patient to gain her confidence and cooperation, and assure her comfort and modesty B. Perform a painless obstetric-gynecologic examination as part of a woman’s general medical examination, including: 1. Breast examination 2. Abdominal examination 3. Complete pelvic examination 4. -

ANMC Specialty Clinic Services
Cardiology Dermatology Diabetes Endocrinology Ear, Nose and Throat (ENT) Gastroenterology General Medicine General Surgery HIV/Early Intervention Services Infectious Disease Liver Clinic Neurology Neurosurgery/Comprehensive Pain Management Oncology Ophthalmology Orthopedics Orthopedics – Back and Spine Podiatry Pulmonology Rheumatology Urology Cardiology • Cardiology • Adult transthoracic echocardiography • Ambulatory electrocardiology monitor interpretation • Cardioversion, electrical, elective • Central line placement and venous angiography • ECG interpretation, including signal average ECG • Infusion and management of Gp IIb/IIIa agents and thrombolytic agents and antithrombotic agents • Insertion and management of central venous catheters, pulmonary artery catheters, and arterial lines • Insertion and management of automatic implantable cardiac defibrillators • Insertion of permanent pacemaker, including single/dual chamber and biventricular • Interpretation of results of noninvasive testing relevant to arrhythmia diagnoses and treatment • Hemodynamic monitoring with balloon flotation devices • Non-invasive hemodynamic monitoring • Perform history and physical exam • Pericardiocentesis • Placement of temporary transvenous pacemaker • Pacemaker programming/reprogramming and interrogation • Stress echocardiography (exercise and pharmacologic stress) • Tilt table testing • Transcutaneous external pacemaker placement • Transthoracic 2D echocardiography, Doppler, and color flow Dermatology • Chemical face peels • Cryosurgery • Diagnosis -

A Clinical and Histological Study of Radiofrequency-Assisted Liposuction (RFAL) Mediated Skin Tightening and Cellulite Improvement ——RFAL for Skin Tightening
Journal of Cosmetics, Dermatological Sciences and Applications, 2011, 1, 36-42 doi:10.4236/jcdsa.2011.12006 Published Online June 2011 (http://www.SciRP.org/journal/jcdsa) A Clinical and Histological Study of Radiofrequency-Assisted Liposuction (RFAL) Mediated Skin Tightening and Cellulite Improvement ——RFAL for Skin Tightening Marc Divaris1, Sylvie Boisnic2, Marie-Christine Branchet2, Malcolm D. Paul3 1Plastic and Maxillo-Facial Surgery, University of Pitie Salpetiere, Paris, France; 2Institution GREDECO, Paris, France; 3Department of Surgery, Aesthetic and PlasticSurgery Institute, University of California, Irvine, USA. Email: [email protected] Received May 1st, 2011; revised May 27th, 2011; accepted June 6th, 2011. ABSTRACT Background: A novel Radiofrequency-Assisted Liposuction (RFAL) technology was evaluated clinically. Parallel origi- nal histological studies were conducted to substantiate the technology’s efficacy in skin tightening, and cellulite im- provement. Methods: BodyTiteTM system, utilizing the RFAL technology, was used for treating patients on abdomen, hips, flanks and arms. Clinical results were measured on 53 patients up to 6 months follow-up. Histological and bio- chemical studies were conducted on 10 donors by using a unique GREDECO model of skin fragments cultured under survival conditions. Fragments from RFAL treated and control areas were examined immediately and after 10 days in culture, representing long-term results. Skin fragments from patients with cellulite were also examined. Results: Grad- ual improvement in circumference reduction (3.9 - 4.9 cm) and linear contraction (8% - 38%) was observed until the third month. These results stabilized at 6 months. No adverse events were recorded. Results were graded as excellent by most patients, including the satisfaction from minimal pain, bleeding, and downtime. -

Types and Efficacy of Diagnostic Modalities of Ectopic Pregnancy
Jebmh.com Original Research Article Types and Efficacy of Diagnostic Modalities of Ectopic Pregnancy Pavani Pinjala1 1Department of Obstetrics and Gynaecology Mahavir Institute of Medical Sciences, Vikarabad, Hyderabad, Telangana, India. ABSTRACT BACKGROUND Ectopic pregnancy is not only the gynaecologist’s most critical emergency but also Corresponding Author: one of the major problems because of its difficulties in diagnosis, increased risks Dr. Pavani Pinjala, of mortality, and its profound implications with regard to future reproductive Block – D - 206, Vazhraa Nirmaan Pushpak Apartments, performance. We wanted to study the types and accuracy of various diagnostic Blooming Dale Road, Nizampet, modalities, and effect of various management modalities of ectopic pregnancy. Hyderabad – 500090, Telangana, India. E-mail: [email protected] METHODS This study was conducted at Meenakshi Medical College Hospital and Research DOI: 10.18410/jebmh/2020/568 Institute, Kanchipuram, for a period of 32 months from May 2010 to October 2012. During the same period, there were 2602 reported pregnancies. How to Cite This Article: Pinjala P. Types and efficacy of diagnostic modalities of ectopic RESULTS pregnancy. J Evid Based Med Healthc The incidence of ectopic pregnancy in the study is 15.3 / 1000 reported 2020; 7(47), 2767-2771. DOI: pregnancies. The incidence of ectopic pregnancy in patients with prior abdominal 10.18410/jebmh/2020/568 surgery was 86.6 %. Only 77.5 % patients gave history of typical amenorrhea. Submission 20-08-2020, 22.5 % patients gave history suggestive of atypical amenorrhoea. It was noted Peer Review 28-08-2020, that 55 % cases presented as tubal rupture, 7.5 % as tubal abortion, 35 % cases Acceptance 05-10-2020, presented with intact tubal pregnancy and 2.5 % cases presented as ovarian Published 23-11-2020. -
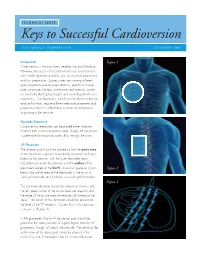
Keys to Successful Cardioversion
TECHNICAL NOTE: Keys to Successful Cardioversion ZOLL MEDICAL CORPORATION DECEMBER 2009 Introduction Figure 1 Cardioversion is the most direct treatment for atrial fibrillation. However, the success of a cardioversion can be enhanced with careful attention to details, such as electrode placement and skin preparation. Success rates vary among different types of patients and among institutions, and this technical note summarizes the keys to enhance cardioversion success as shared by electrophysiologists and cardiologists with vast experience. Cardioversions, which are intended to terminate atrial arrhythmias, require different electrode placement and preparation than for defibrillation to terminate arrhythmias originating in the ventricle. Electrode Placement Cardioversion electrodes can be placed either Anterior– Posterior (AP) or Anterior-Anterior (AA), though AP placement is preferable for maximum current flow through the atria. AP Placement The anterior pad should be placed so that the active area of the electrode is placed immediately adjacent and right lateral to the sternum, with the outer electrode foam circumference under the clavicle and the midline of the electrode located at the fourth intracostal space as shown Figure 2 below (the active area of the electrodes is the tin on a solid gel electrode and the foam on a wet gel electrode). Figure 3 The posterior electrode should be placed as shown, with the left upper corner of the active area sub-scapular and the edge of the active area immediately left lateral to the spine. The center of the electrode should be placed at the level of the T7 vertebra. Current flow in this position is shown in (Figure 3) . In AA placement (Figure 4) the sternal pad should be placed in the same position or slightly higher than for AP placement, though still below the clavicle.