Lorreen Atieno Agandi Degree and Date to Be Conferred
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SU Magazine Spring 2014
A PUBLICATION FOR SALISBURY UNIVERSITY SPRING 2014 SUMagazinewww.salisbury.edu SUALUMNI AND FRIENDS Magazine You know the name, but do you know the face? Digital Conflict Resolution page 9 SU Foundation Turns 40 page 14 Class Notes page 23 SUMagazine SUA PUBLICATION FOR SALISBURY MagazineUNIVERSITY ALUMNI AND FRIENDS 3 Helping in Haiti One alumna helped save lives and limbs following the devastation in Haiti. 13 Campus Then and Now A past and current student share their views of SU. 17 Departments Super Bowl Sea Gull 3 Feature Stories Dan Quinn ’94 shares his experiences 17 Athletics coaching the 19 Alumni News Super Bowl Champion Seahawks. 23 Class Notes ON THE COVER: First principal and Holloway Hall namesake Dr. William Holloway – read about Dr. Holloway and other founders whose www.salisbury.edu names grace buildings around campus on page 11. 1 WELCOME Letter from the President Volume 44 • 2014 PRESIDENT Dr. Janet Dudley-Eshbach By now most people have read how Salisbury University has VICE PRESIDENT OF ADVANCEMENT AND EXTERNAL AFFAIRS expanded its footprint and transformed the skyline of south T. Greg Prince Salisbury with the construction of several remarkable state-of-the- ASSISTANT VICE PRESIDENT OF DEVELOPMENT AND art facilities. At the same time, the profile of our student body has ALUMNI RELATIONS consistently improved. These trends continue in 2013-14: GPAs Jason E. Curtin ’98 and SAT scores remain at the highest level in the institution’s ASSISTANT VICE PRESIDENT OF MARKETING AND PUBLIC RELATIONS history, and the demolition of Caruthers Hall will make way for Susan Maxwell Eagle the soon-to-be crown jewel of our campus the Patricia R. -

TELEVISION: the Onion News Network Anchor
TELEVISION: The Onion News Network Anchor Kathy Johnson iFC TruTV Saturday Night CoHost TruTV IHRA NitroJam Pit Reporter Speed Channel Monster Jam Pit Reporter Speed Channel Open Spaces, Historic Places Host PBS (NJTV) Fresh Host PBS (NJTV) 20 Ways to Get Slim CoHost/Stylist TLC Best Night In Recurring Guest TV Land Better TV Beauty/ Lifestyle Reporter Syndicated Game, Set… Makeover! (Pilot) Host Tennis Channel The Single’s Life Host Dating on Demand Cube Fabulous Host Leftfield Pictures Makeup My Mate (Pilot) Host/Stylist Hearst/ Snap Films Technistas Host We.TV Softball 360 Field Correspondent Fox Sports Net Fit Happens Host Aardvark Video Works Talk Show TV CoHost CN8 Dirtbike Television Host IDrive (Dish Network) Whiplash TV CoHost Jalbert Productions Winter Sportscast Host Jalbert Productions Racing 97: The NASCAR Team Host Sharpleft Productions E.W.P. Host Brainbox Productions The Consumer Guide Show Host Consumer Guide TV LIVE APPEARANCES: *Main Stage Host for Self Magazine’s Annual Workout In the Park Mission Bay Park San Diego, CA Central Park New York, NY Grant Park Chicago, IL *Consultancy Media, Host and Product Spokesperson (Satellite Media Tour TV and Radio) “New Year, New You!” *Plus Media, Host and Product Spokesperson (10 City InStudio TV Tour) “Summer Survival” “Beauty Boosters” * Jimmy Kimmel Live ABC TV Spokesmodel and Presenter for “Pontiac BusStop Giveaway” Series * Miss Maryland USA Titleholder Represent Maryland in the nationally televised 2001 Miss USA Pageant Speaking Engagements, Media Appearances, Charity Fundraisers *WNBC New York, NY. NBC Channel 4 FillIn Traffic Reporter *WCAU Philadelphia, PA. -
Heartlands at Severna Park
in this section | Politics & Opinion | Arts & Entertainment | Business ECRWSS Severna Park Football US POSTAGE F REE - Grab A Copy PAID Beats Glen Burnie, PERMIT NO. 546 COUPON SOURCE YOUR COMMUNITY Millersville, MD V November 2019 Annapolis O I Severna �� Page B1 LOCAL C POSTAL E Park Voice CUSTOMER V Values A St. John L �� Inside Outreach Team U VoicE E Severna Park Visits Jamaica S SERVING OUR COMMUNITY SINCE 1981 �� Page A5 Severna Park VoicE SERVING OUR COMMUNITY SINCE 1981 VOTED THE 2019 SMALL BUSINESS ADMINISTRATION MARYLAND FAMILY-OWNED BUSINESS Of THE YEAR SEVERNA PARK, MD NOM VE BER 1, 2019 A1 Severna Park Native Leads Eastern District Police Station Photo by Chris Fincham Captain Jeff Adams, the commanding officer of the Eastern District Police Station, graduated from SPHS in 1987 and took over the leadership position in July. By Chris Fincham it’s a great place.” [email protected] An SPHS class of 1987 alum, Adams worked at Council Continues Debate On eff Adams always Fort Meade briefly before wanted to be a police applying to become a police officer. Growing up in officer. Baltimore City ac- Complex Forest Conservation Law JSeverna Park, he was raised cepted him, and he worked to help others, and police more than four years there, template a conservation law wants to strengthen protec- important to the county,” work was a natural fit. and then transferred to Amended Bill Will that would impose tougher tions for our remaining for- Trumbauer said. “They soak More than three de- the Anne Arundel County restrictions on developers. -

Megan Gunning TELEVISION
Megan Gunning TELEVISION: The Onion News Network News Anchor iFC Emerging Sports TV Host Syndicated TruTV Saturday Night Co-Host TruTV IHRA NitroJam Pit Reporter Speed Channel Monster Jam Pit Reporter Speed Channel Open Spaces, Historic Places Host PBS (NJTV) Fresh Host PBS (NJTV) 20 Ways to Get Slim Co-Host/Stylist TLC Best Night In Recurring Guest TV Land Better TV Beauty/ Lifestyle Reporter Syndicated Game, Set… Makeover! (Pilot) Host Tennis Channel The Single’s Life Host Dating on Demand Cube Fabulous Host Leftfield Pictures Makeup My Mate (Pilot) Host/Stylist Hearst/ Snap Films Technistas Host We.TV Softball 360 Field Correspondent Fox Sports Net Fit Happens Host Aardvark Video Works Talk Show TV Co-Host CN8 Dirtbike Television Host I-Drive (Dish Network) Whiplash TV Co-Host Jalbert Productions Winter Sportscast Host Jalbert Productions Racing 97: The NASCAR Team Host Sharpleft Productions E.W.P. Host Brainbox Productions The Consumer Guide Show Host Consumer Guide TV LIVE APPEARANCES: *Main Stage Host for Self Magazine’s Annual Workout In the Park - Mission Bay Park- San Diego, CA - Central Park- New York, NY - Grant Park- Chicago, IL *Consultancy Media, Host and Product Spokesperson (Satellite Media Tour- TV and Radio) - “New Year, New You!” *Plus Media, Host and Product Spokesperson (10 City In-Studio TV Tour) - “Summer Survival” - “Beauty Boosters” * Jimmy Kimmel Live- ABC TV - Spokesmodel and Presenter for “Pontiac Bus-Stop Giveaway” Series * Miss Maryland USA Titleholder - Represent Maryland in the nationally televised 2001 Miss USA Pageant - Speaking Engagements, Media Appearances, Charity Fundraisers *WNBC- New York, NY. NBC Channel 4 - Fill-In Traffic Reporter *WCAU- Philadelphia, PA. -

CSM Stepping Stone for Miss Maryland/USA
CSM Stepping Stone for Miss Maryland/USA Posted by TBN On 06/21/2011 For Allyn Rose, of Newburg, attending the College of Southern Maryland was a stepping stone not only to college life but also to a crown. The 22-year-old and former CSM student is the current Miss Maryland USA and competed for the Miss USA title on June 19 in Las Vegas, reaching the semi-finals. Rose attended CSM for one semester in 2006 and said it helped her to find herself before transferring to the University of Maryland (UMD). Rose was recruited to play for the Hawks by CSM Head Volleyball Coach Michelle Ruble, who said it was Rose’s vertical leap that first caught her attention at La Plata High School but that she also saw pluses in Rose’s leadership skills, work ethic and strong academics. Already accepted to attend UMD in 2006, Rose deferred admission to play for CSM. “Ally was a hard sell because she was concerned about being challenged academically,” Ruble said. Rose not only found CSM courses to be challenging, she also found instructors who were supportive. She recalls her communications professor being very tough, but that the rigor helped her develop interpersonal and public speaking skills. To be successful in pageantry, Rose said, “You have to know how to speak, conduct yourself and your body language. There were a lot of intricacies she taught me that definitely helped out.” Rose also recalls the support she received from her English professor, William Barton and the volleyball coaching staff. “They were all great, great people—very supportive. -
Kevin Mccarthy's (Code 450) 64 Days with FEMA
Page 1 The Critical Path Volume 14 number 1 2006 Spring INSIDE THIS ISSUE: Kevin McCarthy and FEMA Page 1 Kevin McCarthy’s (Code 450) STEREO Page 1 64 Days with FEMA Message From The Director Page 2 Watching the coverage of Hurricane Katrina on TV I felt an Tintype Page 3 overwhelming desire to help. My donation to the NASA Fam- ily Assistance fund to help our colleagues at Stennis or Mi- Technology Corner Page 4 choud was one way. However, on Sept. 12th when the Fed- eral Emergency Management Agency (FEMA) requested vol- Quotes Page 5 unteers from other federal agencies to deploy for 30 day PM Challenge 2006 Page 9 minimum field assignments in response and recovery efforts, I jumped at the chance to do more. In fact, the response PMDE Graduation Page 10 from NASA employees was so overwhelming that NASA Comings & Goings Page 11 closed the volunteer list a day or two later. ST5 Launch Page 12 After volunteering, I did not hear from FEMA until I received an email on Sept. 24th, the same day Hurricane Rita made CALIPSO Page 13 (FEMA Continued on page 6) SAP Version Update (SVU) Page 18 Contract Management Mod- Page 19 ule (CMM) STEREO Meets the Public Changes Page 20 The Solar TErrestrial RElations Observatory (STEREO) mis- Social News Page 21 sion was introduced to the community at large with the help Goddard Honor Awards Page 22 of the Public Affairs Office which hosted several events to in- clude the media, VIP’s, stakeholders, foreign space agencies, Pat on the Back Page 27 and the Goddard Family. -
Be Part of a Beautiful Dream…
Be part of a beautiful dream… Where beautiful dreams come true Official State Preliminaries MISS USA® & MISS TEEN USA® 2018 MISS MARYLAND TEEN USA® Contestant’s Handbook TABLE OF CONTENTS SPONSORSHIP INFORMATION (Cont’d) 2 INTRODUCTION ! Welcome from the State Directors ! Submitting your Final Sponsor Listing ! Pageant Office Contact Information ! Sample Telephone Script ! Sample Sponsorship Letter WHAT TO DO NEXT ! Sponsor Receipts 4 ! First Step ! Mark Your Calendar 16 WARDROBE INFORMATION ! Prioritize ! Opening Number ! Deadlines ! Active wear Competition ! Sponsorship ! Evening Gown Competition ! Sponsors & Third Party Vendors ! Interview Competition ! What if I Win? ! Rehearsals / Other ! What Do I Do If I Decide to Withdraw? ! Wardrobe Reference Sheet 6 ACCOMMODATIONS 19 JUDGING INFORMATION ! Host Hotel Location ! Who are the Judges? ! Arrival ! What are they Looking For? ! Meals ! Judging the Phases of Competition ! Pageant Chaperones ! Scoring Procedures ! Transportation ! Incidental Expenses PREPARING FOR THE PAGEANT 20 ! Professional Assistance SPONSORSHIP INFORMATION 7 ! Sponsors ! Overview ! What is it for? GENERAL INFORMATION ! How to Get Sponsorship 23 ! Some Important Tips ! Things to Keep in Mind ! Who are Sponsors? ! Pageant Etiquette ! Press Release Template ! Benefits to Sponsors ! Submitting Payment FREQUENTLY ASKED QUESTIONS 26 1 ONGRATULATIONS FROM THE TATE IRECTORS C S D Congratulations and Welcome! 2018 Miss You have been selected as an Official State Finalist in the Maryland Teen USA pageant! You are about to embark on an invaluable experience that will remain memorable in all the years to come. Only a very select group of young women have the opportunity to participate in this prestigious event, and you are one of them. This year’s pageant promises to be one of the most exciting ever, and we are thrilled to have you as a contestant. -

The Queen City's Crown Jewel
JCSU BULLETIN 2013_2014_v01_Layout 1 12/19/2014 11:29 AM Page 1 The BullA Magazine from Johnson C. Smithet University | 2013-2014in INTELLECTUAL RIGOR SOCIALLY CONSCIOUS AGENTS OF CHANGE GLOBAL EDUCATION CULTURE OF COMMUNITY The Queen City’s Crown jewel 03 jcsu’s favorable impact on charlotte 14 historic george e. davis house restored In this issue 40 stephen joyner sr. inducted to ciaa hall of fame 72 honor roll of donors 2013-14 JCSU BULLETIN 2013_2014_v01_Layout 1 12/19/2014 11:29 AM Page 2 2 C O V E R S T O R Y JCSU BULLETIN 2013_2014_v01_Layout 1 12/19/2014 11:29 AM Page 1 02 President’s Message 03 Cover Story CONTENTS OF TABLE 12 Features 18 University News 26 Academics 36 Student News 40 Athletics 48 Philanthropy 58 Community Engagement 62 Alumni 70 Class Notes A magazine from Johnson C. Smith University 2013 - 2014 President Ronald L. Carter, Ph.D. Vice President Institutional Advancement Joy Paige Executive Editor Sherri Belfield Editors Jennifer K. Gaskins | Vashti Crowell Managing Editor Kate Marcus Contributing Writers Lamont Hinson | Melissa Davis Photographers Jennifer K. Gaskins | Jonathan Keitt | Kate Marcus Published annually by University Communications and Marketing for alumni and friends of JCSU. Johnson C. Smith University is accredited by the Southern Association of Colleges and Schools Commission on Colleges to award baccalaureate and master’s degrees. Contact the Commission on Colleges at 1866 Southern Lane, Decatur, Georgia 30033-4097 or call 404-679-4500 for questions about the accreditation of Johnson C. Smith University. Opposite page: Chairman and CEO of Lowe's Companies, Robert A. -
Official Forms Packet
MISS NEW YORK USA® OFFICIAL FORMS PACKET Please complete pages 1 – 14 and Mail the completed forms as well as a copy of your Birth Certificate and Proof of Residency Documents to Pageant Headquarters by the first deadline on your checklist. Before mailing these forms into Pageant Headquarters, please check to be sure you have: 1. Initialed the bottom of pages 2 – 8 2. Signed and Dated all forms where indicated Official Forms ® 2018 MISS NEW YORK USA First & Last Name: _______________________________________________________________ Your name will be printed in the Official State Program Book as written above. (No middle name or initial.) Address: ______________________________________________________________________ City: ___________________________________State: __________________ Zip: ___________ Phone Number: ( )___________________Current Age: ____________________________ Date of Birth: __________________________ Age you will be on December 31, 2017: ________ In order for you to participate in the 2018 MISS NEW YORK USA® pageant, please complete and return pages 1 - 14 of this form, plus photocopies of your birth certificate and proof of residency documents. Please refer to the enclosed checklist for your due date. Parent/Guardian signatures are required only if you are under 18 years old on the date you enter your signature. ! 1. Contestant’s Official Entry Form / Contract ! Date of birth entered on page 2 ! Shaded Boxes completed on pages 2, 3 and 6 ! Bottom of pages 2 - 8 initialed ! All signatures complete, and initials on page 8 ! 2. Release & Participation Agreement ! 3. Comportment and Hotel Responsibilities ! 4. Contestant Agreement ! 5. Pageant Weekend Rules & Regulations ! 6. Medical Information Form ! 7. Title Request Form ! 8. Proof of Age Documentation – A photocopy of birth certificate is required ! 9. -

Adrianna David Resume
@adriannacdavid ADRIANNA DAVID (240) 672-2250 [email protected] Actor // Host // Social Media // Nonprofit // www.adriannadavid.com EXPERIENCE // SKILLS // The Kidney Project, San Francisco — N ational Spokesperson Authenticity + Charisma SEPTEMBER 2014 - PRESENT Goal-Oriented + Purpose Dedicated to raising awareness and funds for this research project at the Driven University of California San Francisco who is developing a bioartificial kidney to replace dialysis. Raised over $750,000 through Charities Angels Public Speaking + Hosting #JulianasHope Campaign in honor of my cousin. Creative Direction + Social Media Strategy Decades, Washington DC — V IP Host SEPTEMBER 2018 - AUGUST 2019 Grassroots Fundraising + Greeted and recruited guests upon entry + exit. Organized reservations Nonprofit Event Planning and walk-in parties. Handled payments at door and/or once escorted to Personal Branding + table. Assisted marketing and promoting events. Developed rapport with Interview Packaging clients and ascertained any needs when necessary. Drawing + Painting Miss America Organization, Maryland — M iss Maryland 2018 JUNE 2018 - JUNE 2019 Keynote Speaker to 45+ organizations on various topics including kidney AWARDS // disease, volunteerism, scholarships, women in leadership, and female empowerment. State Ambassador for Children’s Miracle Network Maryland Senate and House Hospitals. Represented Maryland at the 2019 Miss America Competition. of Representatives floor Doubled followers on official @missamericaMD Instagram account. recognition(s) (2019) Miss Universe Organization, Maryland — M ISS MARYLAND Jean Bartel Quality of Life USA® 2017 Award 1st Runner-Up at Miss America (2018) NOVEMBER 2016 - NOVEMBER 2017 Spokesperson for MISS MARYLAND USA, partners + sponsors. Traveled Governor’s Volunteer Service making over 175 appearances on behalf of the State of Maryland. Certificate recipient, Larry Represented Maryland at the 2017 MISS USA® Competition. -
Ssbo Event Manual
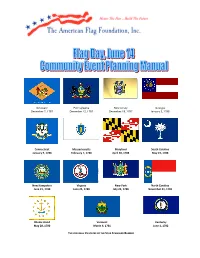
Delaware Pennsylvania New Jersey Georgia December 7, 1787 December 12, 1787 December 18, 1787 January 2, 1788 Connecticut Massachusetts Maryland South Carolina January 9, 1788 February 7, 1788 April 28, 1788 May 23, 1788 New Hampshire Virginia New York North Carolina June 21, 1788 June 25, 1788 July 26, 1788 November 21, 1789 Rhode Island Vermont Kentucky May 28, 1790 March 4, 1791 June 1, 1792 THE ORIGINAL 15 STATES OF THE STAR SPANGLED BANNER Star-Spangled Banner Outreach Program’s June 14th National Flag Day Community Event Planning Manual for THE NATIONAL PAUSE FOR THE PLEDGE OF ALLEGIANCE PARADE OF STATE FLAGS LIVING AMERICAN FLAG PREFACE AFF MISSION STATEMENT: Enhance awareness of the American Flag as the symbol of patriotism through education, outreach and recognition. Founded: 1982, as a non-profit, national patriotic education organization in Maryland (formerly The National Flag Day Foundation, Inc. until its name change in 2006) OUR CORE PROGRAMS: The Living American Flag (15-star 15-stripe Star-Spangled Banner) held in the 3d week of May each year at Fort McHenry National Monument and Historic Shrine, Baltimore, Maryland, birthplace of the Star-Spangled Banner The Annual National Pause for the Pledge of Allegiance, parade of state flags and fireworks held annually on Flag Day, June 14, at Fort McHenry National Monument and Historic Shrine. The Star- Spangled Banner Outreach Program: An AFF program packaged for “export” based on this manual, for the use of other community sponsoring organizations nationwide that do not have easy access to Ft McHenry. The Louis V. Koerber Patriotism Award Luncheon: an annual event honoring local and national patriotic leaders. -

Miss Oklahoma Usa, Olivia Jordan, Wins the Miss Usa 2015 Title During the Live Reelz Channel Telecast from Baton Rouge, Louisiana
MISS OKLAHOMA USA, OLIVIA JORDAN, WINS THE MISS USA 2015 TITLE DURING THE LIVE REELZ CHANNEL TELECAST FROM BATON ROUGE, LOUISIANA Baton Rouge, LA – July 12, 2015 – This evening, a panel of former Miss Universe Organization titleholders chose Miss Oklahoma USA, Olivia Jordan, as Miss USA 2015. Emmy Award-winning game show host Todd Newton and former Miss Wisconsin USA 2009 Alex Wehrley hosted the competition. OK! TV’s Julie Alexandria provided backstage behind-the-scenes commentary from the Baton Rouge River Center in Baton Rouge, Louisiana. Olivia Jordan, a 26-year-old from Tulsa, Oklahoma, has appeared in several national/international commercials and feature films. Olivia is a graduate of Boston University, where she earned a degree in health science. As a model, Olivia has walked for Sherri Hill in New York Fashion Week 2015 and the runway at Miami Mercedes-Benz Fashion Week Swim 2014. She has also been featured in Cosmopolitan, Shape and Vogue Japan. Olivia has been recognized by Children of the Night, a group dedicated to getting children out of prostitution, for her work with the organization. The judging panel for the 2015 MISS USA® Pageant included Nana Meriwether, Miss USA 2012, two-time All- American athlete and co-founder of the non-profit Meriwether Foundation, which serves the most impoverished sectors in five southern African nations; Leila Umenyiora, Miss Universe 2011, humanitarian and named Drylands Ambassador by the United Nation Convention to Combat Desertification (UNCCD); Rima Fakih, Miss USA 2010, named one of the