APOMORPHINE Injection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Citizen Cyborg.” Citizen a Groundbreaking Work of Social Commentary, Citizen Cyborg Artificial Intelligence, Nanotechnology, and Genetic Engineering —DR
hughes (continued from front flap) $26.95 US ADVANCE PRAISE FOR ARTIFICIAL INTELLIGENCE NANOTECHNOLOGY GENETIC ENGINEERING MEDICAL ETHICS INVITRO FERTILIZATION STEM-CELL RESEARCH $37.95 CAN citizen LIFE EXTENSION GENETIC PATENTS HUMAN GENETIC ENGINEERING CLONING SEX SELECTION ASSISTED SUICIDE UNIVERSAL HEALTHCARE human genetic engineering, sex selection, drugs, and assisted In the next fifty years, life spans will extend well beyond a century. suicide—and concludes with a concrete political agenda for pro- cyborg Our senses and cognition will be enhanced. We will have greater technology progressives, including expanding and deepening control over our emotions and memory. Our bodies and brains “A challenging and provocative look at the intersection of human self-modification and human rights, reforming genetic patent laws, and providing SOCIETIES MUST RESPOND TO THE REDESIGNED HUMAN OF FUTURE WHY DEMOCRATIC will be surrounded by and merged with computer power. The limits political governance. Everyone wondering how society will be able to handle the coming citizen everyone with healthcare and a basic guaranteed income. of the human body will be transcended, as technologies such as possibilities of A.I. and genomics should read Citizen Cyborg.” citizen A groundbreaking work of social commentary, Citizen Cyborg artificial intelligence, nanotechnology, and genetic engineering —DR. GREGORY STOCK, author of Redesigning Humans illuminates the technologies that are pushing the boundaries of converge and accelerate. With them, we will redesign ourselves and humanness—and the debate that may determine the future of the our children into varieties of posthumanity. “A powerful indictment of the anti-rationalist attitudes that are dominating our national human race itself. -

Addictions and the Brain
9/18/2012 Addictions and the Brain TAAP Conference September 14, 2012 Acknowledgements • La Hacienda Treatment Center • American Society of Addiction Medicine • National Institute of Drug Abuse © 2012 La Hacienda Treatment Center. All rights reserved. 1 9/18/2012 Definition • A primary, progressive biochemical, psychosocial, genetically transmitted chronic disease of relapse who’s hallmarks are denial, loss of control and unmanageability. DSM IV Criteria for dependency: At least 3 of the 7 below 1. Withdrawal 2. Tolerance 3. The substance is taken in larger amounts or over a longer period than was intended. 4. There is a persistent desire or unsuccessful efforts to cut down or control substance use. 5. A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from its effects. 6. Important social, occupational, or recreational activities are given up or reduced because of the substance use. 7. The substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance. © 2012 La Hacienda Treatment Center. All rights reserved. 2 9/18/2012 Dispute between behavior and disease Present understanding of the Hypothalamus location of the disease hypothesis. © 2012 La Hacienda Treatment Center. All rights reserved. 3 9/18/2012 © 2012 La Hacienda Treatment Center. All rights reserved. 4 9/18/2012 © 2012 La Hacienda Treatment Center. All rights reserved. 5 9/18/2012 Dispute regarding behavior versus disease © 2012 La Hacienda Treatment Center. All rights reserved. 6 9/18/2012 © 2012 La Hacienda Treatment Center. -

“STOP” and “GO” Pathways for the Treatment of Alcohol Use Disorders
UCSF UC San Francisco Previously Published Works Title Targeting the intracellular signaling "STOP" and "GO" pathways for the treatment of alcohol use disorders. Permalink https://escholarship.org/uc/item/6hd3x2cv Journal Psychopharmacology, 235(6) ISSN 0033-3158 Authors Ron, Dorit Berger, Anthony Publication Date 2018-06-01 DOI 10.1007/s00213-018-4882-z Peer reviewed eScholarship.org Powered by the California Digital Library University of California Psychopharmacology (2018) 235:1727–1743 https://doi.org/10.1007/s00213-018-4882-z REVIEW Targeting the intracellular signaling “STOP” and “GO” pathways for the treatment of alcohol use disorders Dorit Ron1 & Anthony Berger1 Received: 18 January 2018 /Accepted: 12 March 2018 /Published online: 14 April 2018 # The Author(s) 2018 Abstract In recent years, research has identified the molecular and neural substrates underlying the transition of moderate “social” con- sumption of alcohol to the characteristic alcohol use disorder (AUD) phenotypes including excessive and compulsive alcohol use which we define in the review as the GO signaling pathways. In addition, growing evidence points to the existence of molecular mechanisms that keep alcohol consumption in check and that confer resilience for the development of AUD which we define herein as the STOP signaling pathways. In this review, we focus on examples of the GO and the STOP intracellular signaling pathways and discuss our current knowledge of how manipulations of these pathways may be used for the treatment of AUD. Keywords Alcohol . Addiction . Signaling . Translation . Medication Development . Fyn . mTOR . BDNF . GDNF Introduction medications such as naltrexone, acamprosate, and disulfiram not only are beneficial but also suffer from efficacy and com- Alcohol use disorder (AUD) is a serious worldwide health prob- pliance issues (Wackernah et al. -

Memantine Increases NMDA Receptor Level in the Prefrontal Cortex
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Dundee Online Publications University of Dundee Memantine increases NMDA receptor level in the prefrontal cortex but fails to reverse apomorphine-induced conditioned place preference in rats Ndlazi, Ziphozethu; Abboussi, Oualid; Mabandla, Musa; Daniels, Willie Published in: AIMS Neuroscience DOI: 10.3934/NEUROSCIENCE.2018.4.211 Publication date: 2018 Document Version Publisher's PDF, also known as Version of record Link to publication in Discovery Research Portal Citation for published version (APA): Ndlazi, Z., Abboussi, O., Mabandla, M., & Daniels, W. (2018). Memantine increases NMDA receptor level in the prefrontal cortex but fails to reverse apomorphine-induced conditioned place preference in rats. AIMS Neuroscience, 5(4), 211-220. https://doi.org/10.3934/NEUROSCIENCE.2018.4.211 General rights Copyright and moral rights for the publications made accessible in Discovery Research Portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from Discovery Research Portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain. • You may freely distribute the URL identifying the publication in the public portal. Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. -

Patient Information
Patient Information Memantine Hydrochloride (me-MAN-teen HYE-droe-KLOR-ide) Tablets Read this Patient Information that comes with Memantine Hydrochloride Tablets before you start taking it and each time you get a refill. There may be new information. This information does not take the place of talking to your doctor about your medical condition or your treatment. What are Memantine Hydrochloride Tablets? Memantine Hydrochloride Tablets are a prescription medicine used for the treatment of moderate to severe dementia in people with Alzheimer's disease. Memantine Hydrochloride Tablets belongs to a class of medicines called NMDA (N-methyl-D-aspartate) inhibitors. It is not known if Memantine Hydrochloride Tablets are safe and effective in children. Who should not take Memantine Hydrochloride Tablets? Do not take Memantine Hydrochloride Tablets if you are allergic to memantine or any of the ingredients in Memantine Hydrochloride Tablets. See the end of this leaflet for a complete list of ingredients in Memantine Hydrochloride Tablets. What should I tell my doctor before taking Memantine Hydrochloride Tablets? Before you take Memantine Hydrochloride Tablets, tell your doctor if you: • have or have had seizures • have or have had problems passing urine • have or have had bladder or kidney problems • have liver problems • have any other medical conditions • are pregnant or plan to become pregnant. It is not known if Memantine Hydrochloride Tablets will harm your unborn baby. • are breastfeeding or plan to breastfeed. It is not known if memantine passes into your breast milk. You and your doctor should decide if you will take Memantine Hydrochloride Tablets or breastfeed. -

Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss
Supplemental Material can be found at: /content/suppl/2020/12/18/73.1.202.DC1.html 1521-0081/73/1/202–277$35.00 https://doi.org/10.1124/pharmrev.120.000056 PHARMACOLOGICAL REVIEWS Pharmacol Rev 73:202–277, January 2021 Copyright © 2020 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: MICHAEL NADER Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss Antonio Inserra, Danilo De Gregorio, and Gabriella Gobbi Neurobiological Psychiatry Unit, Department of Psychiatry, McGill University, Montreal, Quebec, Canada Abstract ...................................................................................205 Significance Statement. ..................................................................205 I. Introduction . ..............................................................................205 A. Review Outline ........................................................................205 B. Psychiatric Disorders and the Need for Novel Pharmacotherapies .......................206 C. Psychedelic Compounds as Novel Therapeutics in Psychiatry: Overview and Comparison with Current Available Treatments . .....................................206 D. Classical or Serotonergic Psychedelics versus Nonclassical Psychedelics: Definition ......208 Downloaded from E. Dissociative Anesthetics................................................................209 F. Empathogens-Entactogens . ............................................................209 -

The Use of Psychedelic Drugs in the Treatment of Problematic Drug and Alcohol Use
Tripping up addiction: The use of psychedelic drugs in the treatment of problematic drug and alcohol use Short Title: Illicit drugs in the treatment of addiction Celia Morgan 1,3, Amy McAndrew1, Tobias Stevens1, David Nutt2, Will Lawn1,3 1. Psychopharmacology and Addiction Research Centre, University of Exeter, UK 2. Centre for Neuropsychopharmacology, Imperial College London, UK 3. Clinical Psychopharmacology Unit, University College London, UK Address Corrrespondence to: Celia Morgan Psychopharmacology and Addiction Research Centre Washington Singer Laboratory University of Exeter Perry Road, Exeter Devon UK EX4 4QG Key words: addiction, psychedelics, ketamine, ibogaine, ayahuasca, LSD , psilocybin, neurogenesis, 1 Highlights: Psilocybin may reduce alcohol and tobacco use in addicted samples. Ibogaine and ayahuasca have shown promise in the treatment of various addictions through observational studies. Ketamine has been used to treat alcohol dependence and reduces cocaine self- administration in the human laboratory. Randomised controlled trials are greatly needed to further test the efficacy of all of these compounds. Psychedelic drugs may have their therapeutic qualities due to anti-depressant effects, stimulating neuroplasticity and long-term psychological changes. 2 Abstract Psychedelic drugs have been used as treatments in indigenous cultures for thousands of years. Yet, due to their legal status, there has been limited scientific research into the therapeutic potential of these compounds for psychiatric disorders. In the absence of other effective treatments however, researchers have begun again to systematically investigate such compounds and there is now evidence pointing to the use of psychedelic drugs in the treatment of addiction. In this review we focus on human evidence for the effectiveness of preparations used by indigenous cultures in the Amazon (ayahausca) and Africa (ibogaine) and worldwide (psilocybin), and more recently synthetised drugs such as the serotonergic hallucinogen LSD and the dissociative anaesthetic ketamine. -
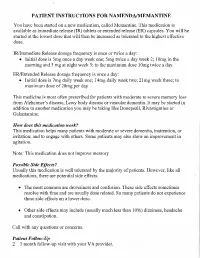
PATIENT INSTRUCTIONS for NAMENDA/MEMANTINE You Have Been Started on a New Medication, Called Memantine
PATIENT INSTRUCTIONS FOR NAMENDA/MEMANTINE You have been started on a new medication, called Memantine. This medication is available as immediate release (IR) tablets or extended release (ER) capsules. You will be started at the lowest dose that will then be increased as tolerated to the highest effective dose. IR/ImmediateRelease dosage frequencyis once or twice a day: • Initial dose is 5mg once a day week one; 5mg twice a day week 2; 10mg in the morning and 5 mg at night week 3; to the maximum dose 10mg twice a day. ER/Extended Release dosage frequencyis once a day: • Initial dose is 7mg daily week one; 14mg daily week two; 21mg week three; to maximum dose of 28mg per day This medicine is most oftenprescribed for patients with moderate to severe memory loss fromAlzheimer's disease, Lewy body disease or vascular dementia. It may be started in addition to another medication you may be taking like Donepezil, Rivastigmine or Galantamine. How does thismedication work?. This medication helps many patients with moderate or severe dementia, inattention, or irritation; and to engage with others. Some patients may also show an improvement in agitation. Note: This medication does not improve memory Possible Side Effects? Usually this medication is well tolerated by the majority of patients. However, like all medications, there are potential side effects. • The most common are drowsiness and confusion. These side effectssometimes resolve with time and are usually dose related. So many patients do not experience these side effectson a lower dose. • Other side effectsmay include (usually much less than 10%) dizziness, headache and constipation. -

WO 2013/085849 A2 13 June 2013 (13.06.2013) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2013/085849 A2 13 June 2013 (13.06.2013) P O P C T (51) International Patent Classification: AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, C07D 487/22 (2006.01) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (21) International Application Number: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, PCT/US20 12/067627 KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, (22) International Filing Date: ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, 3 December 2012 (03.12.2012) NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, (25) Filing Language: English TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, (26) Publication Language: English ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/569,144 9 December 201 1 (09. 12.201 1) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, (71) Applicant: DEMERX, INC. [US/US]; 4400 Biscayne UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, Boulevard, Suite 580, Miami, Florida 33 137 (US). TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, LV, (72) Inventors; and MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, SM, (71) Applicants : GLESS, Richard D. -

Identification of Genes Regulated by Memantine and MK-801 in Adult Rat Brain by Cdna Microarray Analysis
Neuropsychopharmacology (2004) 29, 1070–1079 & 2004 Nature Publishing Group All rights reserved 0893-133X/04 $25.00 www.neuropsychopharmacology.org Identification of Genes Regulated by Memantine and MK-801 in Adult Rat Brain by cDNA Microarray Analysis ´ ´1 1 ,1 Marketa Marvanova , Merja Lakso and Garry Wong* 1AI Virtanen Institute for Molecular Sciences, Department of Neurobiology, Laboratory of Functional Genomics and Bioinformatics, University of Kuopio, Kuopio, Finland In this study, we monitored gene expression profiles using cDNA microarrays after an acute systemic administration of the high affinity N-methyl-D-aspartate (NMDA) uncompetitive antagonist MK-801 (1 mg/kg; 4 h), and the clinically used moderate affinity antagonist memantine (25 mg/kg; 4 h) in adult rat brains. From a microarray containing 1090 known genes, 13 genes were regulated by both treatments of which 12 were upregulated and one was downregulated. In addition, 28 and 34 genes were regulated (X1.5- or p0.67- fold change) by either memantine or MK-801, respectively. Genes commonly regulated by both treatments and not previously reported were confirmed by in situ hybridization (ISH) and include regenerating liver inhibitory factor-1 (RL/IF-1), GDP-dissociation inhibitor 1 2 þ þ þ (GDI-1), neural visinin Ca -binding protein 2 (NVP-2), neuromedin B receptor, and Na /K transporting ATPase 2b. ISH with memantine (5–50 mg/kg) revealed regulation of these genes in other cortical and hippocampal regions. RL/IF-1 induction occurred at 1 h and returned to basal levels by 8 h, consistent with the profile of an immediate early gene. -

Memantine Hydrochloride)
NDA 21-627 Page 3 Namenda® Tablets/Oral Solution (memantine hydrochloride) Rx Only DESCRIPTION Namenda® (memantine hydrochloride) is an orally active NMDA receptor antagonist. The chemical name for memantine hydrochloride is 1-amino-3,5-dimethyladamantane hydrochloride with the following structural formula: . NH2 HCl CH3 H3C The molecular formula is C12H21N•HCl and the molecular weight is 215.76. Memantine HCl occurs as a fine white to off-white powder and is soluble in water. Namenda is available as tablets or as an oral solution. Namenda is available for oral administration as capsule-shaped, film-coated tablets containing 5 mg and 10 mg of memantine hydrochloride. The tablets also contain the following inactive ingredients: microcrystalline cellulose, lactose monohydrate, colloidal silicon dioxide, talc and magnesium stearate. In addition the following inactive ingredients are also present as components of the film coat: hypromellose, triacetin, titanium dioxide, FD&C yellow #6 and FD&C blue #2 (5 mg tablets), iron oxide black (10 mg tablets). Namenda oral solution contains memantine hydrochloride in a strength equivalent to 2 mg of memantine hydrochloride in each mL. The oral solution also contains the following inactive ingredients: sorbitol solution (70%), methyl paraben, propylparaben, propylene glycol, glycerin, natural peppermint flavor #104, citric acid, sodium citrate, and purified water. CLINICAL PHARMACOLOGY Mechanism of Action and Pharmacodynamics Persistent activation of central nervous system N-methyl-D-aspartate (NMDA) receptors by the excitatory amino acid glutamate has been hypothesized to contribute to the symptomatology of Alzheimer’s disease. Memantine is postulated to exert its therapeutic effect through its action as a low to moderate affinity uncompetitive (open-channel) NMDA receptor antagonist which binds preferentially to the NMDA receptor-operated cation channels. -

Product Monograph
PRODUCT MONOGRAPH Pr Ebixa® Memantine Hydrochloride Tablets 10 mg N-methyl-D-aspartate (NMDA) receptor antagonist Lundbeck Canada Inc. Date of revision: 2600 Alfred-Nobel July 8th, 2016 Suite 400 St-Laurent, QC H4S 0A9 Control No. 181785 2 NAME OF DRUG Pr Ebixa® Memantine Hydrochloride Tablets 10 mg THERAPEUTIC CLASSIFICATION N-methyl-D-aspartate (NMDA) receptor antagonist ACTION AND CLINICAL PHARMACOLOGY Persistent activation of the central nervous system N-methyl-D-aspartate (NMDA) receptors by the excitatory amino acid glutamate has been hypothesized to contribute to the symptomatology of Alzheimer’s disease. Memantine is postulated to exert its therapeutic effect through its action as a low to moderate affinity uncompetitive (open channel) NMDA receptor antagonist, which binds preferentially to the NMDA receptor-operated cation channels. It blocks the effects of pathologically elevated sustained levels of glutamate that may lead to neuronal dysfunction. There is no clinical evidence that memantine prevents or slows neurodegeneration or alters the course of the underlying dementing process in patients with Alzheimer’s disease. Memantine exhibits low to negligible affinity for other receptors (GABA, benzodiazepine, dopamine, adrenergic, noradrenergic, histamine and glycine) or voltage-dependent Ca2+, Na+ or K+ channels. In addition, it does not directly affect the acetylcholine receptor or cholinergic transmission, which have been implicated in the cholinomimetic side effects (e.g., increased gastric acid secretion, nausea and vomiting) seen with acetylcholinesterase inhibitors. Memantine showed antagonist effects at the 5HT3 receptor with a potency similar to that for the NMDA receptor. 3 In vitro studies have shown that memantine does not affect the reversible inhibition of acetylcholinesterase by donepezil or galantamine.