ICD-10 Dx Edit Code Lists
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Male Reproductive System
Management of Men’s Reproductive 3 Health Problems Men’s Reproductive Health Curriculum Management of Men’s Reproductive 3 Health Problems © 2003 EngenderHealth. All rights reserved. 440 Ninth Avenue New York, NY 10001 U.S.A. Telephone: 212-561-8000 Fax: 212-561-8067 e-mail: [email protected] www.engenderhealth.org This publication was made possible, in part, through support provided by the Office of Population, U.S. Agency for International Development (USAID), under the terms of cooperative agreement HRN-A-00-98-00042-00. The opinions expressed herein are those of the publisher and do not necessarily reflect the views of USAID. Cover design: Virginia Taddoni ISBN 1-885063-45-8 Printed in the United States of America. Printed on recycled paper. Library of Congress Cataloging-in-Publication Data Men’s reproductive health curriculum : management of men’s reproductive health problems. p. ; cm. Companion v. to: Introduction to men’s reproductive health services, and: Counseling and communicating with men. Includes bibliographical references. ISBN 1-885063-45-8 1. Andrology. 2. Human reproduction. 3. Generative organs, Male--Diseases--Treatment. I. EngenderHealth (Firm) II. Counseling and communicating with men. III. Title: Introduction to men’s reproductive health services. [DNLM: 1. Genital Diseases, Male. 2. Physical Examination--methods. 3. Reproductive Health Services. WJ 700 M5483 2003] QP253.M465 2003 616.6’5--dc22 2003063056 Contents Acknowledgments v Introduction vii 1 Disorders of the Male Reproductive System 1.1 The Male -
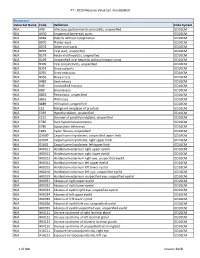
PT - 2020 Measure Value Set Avoidableed
PT - 2020 Measure Value Set_AvoidableED Numerator Value Set Name Code Definition Code System N/A A09 Infectious gastroenteritis and colitis, unspecified ICD10CM N/A A630 Anogenital (venereal) warts ICD10CM N/A B069 Rubella without complication ICD10CM N/A B070 Plantar wart ICD10CM N/A B078 Other viral warts ICD10CM N/A B079 Viral wart, unspecified ICD10CM N/A B179 Acute viral hepatitis, unspecified ICD10CM N/A B199 Unspecified viral hepatitis without hepatic coma ICD10CM N/A B309 Viral conjunctivitis, unspecified ICD10CM N/A B354 Tinea corporis ICD10CM N/A B355 Tinea imbricata ICD10CM N/A B356 Tinea cruris ICD10CM N/A B483 Geotrichosis ICD10CM N/A B49 Unspecified mycosis ICD10CM N/A B80 Enterobiasis ICD10CM N/A B852 Pediculosis, unspecified ICD10CM N/A B853 Phthiriasis ICD10CM N/A B889 Infestation, unspecified ICD10CM N/A C61 Malignant neoplasm of prostate ICD10CM N/A E039 Hypothyroidism, unspecified ICD10CM N/A E215 Disorder of parathyroid gland, unspecified ICD10CM N/A E780 Pure hypercholesterolemia ICD10CM N/A E786 Lipoprotein deficiency ICD10CM N/A E849 Cystic fibrosis, unspecified ICD10CM N/A G5600 Carpal tunnel syndrome, unspecified upper limb ICD10CM N/A G5601 Carpal tunnel syndrome, right upper limb ICD10CM N/A G5602 Carpal tunnel syndrome, left upper limb ICD10CM N/A H00011 Hordeolum externum right upper eyelid ICD10CM N/A H00012 Hordeolum externum right lower eyelid ICD10CM N/A H00013 Hordeolum externum right eye, unspecified eyelid ICD10CM N/A H00014 Hordeolum externum left upper eyelid ICD10CM N/A H00015 Hordeolum externum -

Utility of the Digital Rectal Examination in the Emergency Department: a Review
The Journal of Emergency Medicine, Vol. 43, No. 6, pp. 1196–1204, 2012 Published by Elsevier Inc. Printed in the USA 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2012.06.015 Clinical Reviews UTILITY OF THE DIGITAL RECTAL EXAMINATION IN THE EMERGENCY DEPARTMENT: A REVIEW Chad Kessler, MD, MHPE*† and Stephen J. Bauer, MD† *Department of Emergency Medicine, Jesse Brown VA Medical Center and †University of Illinois-Chicago College of Medicine, Chicago, Illinois Reprint Address: Chad Kessler, MD, MHPE, Department of Emergency Medicine, Jesse Brown Veterans Hospital, 820 S Damen Ave., M/C 111, Chicago, IL 60612 , Abstract—Background: The digital rectal examination abdominal pain and acute appendicitis. Stool obtained by (DRE) has been reflexively performed to evaluate common DRE doesn’t seem to increase the false-positive rate of chief complaints in the Emergency Department without FOBTs, and the DRE correlated moderately well with anal knowing its true utility in diagnosis. Objective: Medical lit- manometric measurements in determining anal sphincter erature databases were searched for the most relevant arti- tone. Published by Elsevier Inc. cles pertaining to: the utility of the DRE in evaluating abdominal pain and acute appendicitis, the false-positive , Keywords—digital rectal; utility; review; Emergency rate of fecal occult blood tests (FOBT) from stool obtained Department; evidence-based medicine by DRE or spontaneous passage, and the correlation be- tween DRE and anal manometry in determining anal tone. Discussion: Sixteen articles met our inclusion criteria; there INTRODUCTION were two for abdominal pain, five for appendicitis, six for anal tone, and three for fecal occult blood. -

Hypocalcemia Associated with Subcutaneous Fat Necrosis of the Newborn: Case Report and Literature Review Alphonsus N
case report Oman Medical Journal [2017], Vol. 32, No. 6: Hypocalcemia Associated with Subcutaneous Fat Necrosis of the Newborn: Case Report and Literature Review Alphonsus N. Onyiriuka 1* and Theodora E. Utomi2 1Endocrine and Metabolic Unit, Department of Child Health, University of Benin Teaching Hospital, Benin City, Nigeria 2Special Care Baby Unit, Department of Nursing Services, St Philomena Catholic Hospital, Benin City, Nigeria ARTICLE INFO ABSTRACT Article history: Subcutaneous fat necrosis of the newborn (SCFNN) is a rare benign inflammatory Received: 4 November 2015 disorder of the adipose tissue but may be complicated by hypercalcemia or less frequently, Accepted: 21 October 2016 hypocalcemia, resulting in morbidity and mortality. Here we report the case of a neonate Online: with subcutaneous fat necrosis who surprisingly developed hypocalcemia instead DOI 10.5001/omj.2017.99 of hypercalcemia. A full-term female neonate was delivered by emergency cesarean section for fetal distress and was subsequently admitted to the Special Care Baby Keywords: Hypocalcemia; Infant, Unit. The mother’s pregnancy was uncomplicated up to delivery. Her anthropometric Newborn; Subcutaneous Fat measurements were birth weight 4.1 kg (95th percentile), length 50 cm (50th percentile), Necrosis; Perinatal Stress. and head circumference 34.5 cm (50th percentile). The Apgar scores were 2, 3, and 8 at 1, 5, 10 minutes, respectively. There was no abnormal facies and she was fed with breast milk only. On the seventh day of life, the infant was found to have multiple nodules located in the neck, upper back, and right arm. The nodules were firm, well circumscribed with no evidence of tenderness. -

16. Questions and Answers
16. Questions and Answers 1. Which of the following is not associated with esophageal webs? A. Plummer-Vinson syndrome B. Epidermolysis bullosa C. Lupus D. Psoriasis E. Stevens-Johnson syndrome 2. An 11 year old boy complains that occasionally a bite of hotdog “gives mild pressing pain in his chest” and that “it takes a while before he can take another bite.” If it happens again, he discards the hotdog but sometimes he can finish it. The most helpful diagnostic information would come from A. Family history of Schatzki rings B. Eosinophil counts C. UGI D. Time-phased MRI E. Technetium 99 salivagram 3. 12 year old boy previously healthy with one-month history of difficulty swallowing both solid and liquids. He sometimes complains food is getting stuck in his retrosternal area after swallowing. His weight decreased approximately 5% from last year. He denies vomiting, choking, gagging, drooling, pain during swallowing or retrosternal pain. His physical examination is normal. What would be the appropriate next investigation to perform in this patient? A. Upper Endoscopy B. Upper GI contrast study C. Esophageal manometry D. Modified Barium Swallow (MBS) E. Direct laryngoscopy 4. A 12 year old male presents to the ER after a recent episode of emesis. The parents are concerned because undigested food 3 days old was in his vomit. He admits to a sensation of food and liquids “sticking” in his chest for the past 4 months, as he points to the upper middle chest. Parents relate a 10 lb (4.5 Kg) weight loss over the past 3 months. -

N35.12 Postinfective Urethral Stricture, NEC, Female N35.811 Other
N35.12 Postinfective urethral stricture, NEC, female N35.811 Other urethral stricture, male, meatal N35.812 Other urethral bulbous stricture, male N35.813 Other membranous urethral stricture, male N35.814 Other anterior urethral stricture, male, anterior N35.816 Other urethral stricture, male, overlapping sites N35.819 Other urethral stricture, male, unspecified site N35.82 Other urethral stricture, female N35.911 Unspecified urethral stricture, male, meatal N35.912 Unspecified bulbous urethral stricture, male N35.913 Unspecified membranous urethral stricture, male N35.914 Unspecified anterior urethral stricture, male N35.916 Unspecified urethral stricture, male, overlapping sites N35.919 Unspecified urethral stricture, male, unspecified site N35.92 Unspecified urethral stricture, female N36.0 Urethral fistula N36.1 Urethral diverticulum N36.2 Urethral caruncle N36.41 Hypermobility of urethra N36.42 Intrinsic sphincter deficiency (ISD) N36.43 Combined hypermobility of urethra and intrns sphincter defic N36.44 Muscular disorders of urethra N36.5 Urethral false passage N36.8 Other specified disorders of urethra N36.9 Urethral disorder, unspecified N37 Urethral disorders in diseases classified elsewhere N39.0 Urinary tract infection, site not specified N39.3 Stress incontinence (female) (male) N39.41 Urge incontinence N39.42 Incontinence without sensory awareness N39.43 Post-void dribbling N39.44 Nocturnal enuresis N39.45 Continuous leakage N39.46 Mixed incontinence N39.490 Overflow incontinence N39.491 Coital incontinence N39.492 Postural -

Intravenous Drug Use-Associated Infective Endocarditis in Pregnant Patients at a Hospital in West Virginia
Open Access Original Article DOI: 10.7759/cureus.17218 Intravenous Drug Use-Associated Infective Endocarditis in Pregnant Patients at a Hospital in West Virginia Deena Dahshan 1 , Mohamed Suliman 2 , Ebad U. Rahman 3 , Zachary Curtis 1 , Ellen Thompson 2 1. Internal Medicine, Marshall University Joan C. Edwards School of Medicine, Huntington, USA 2. Cardiology, Marshall University Joan C. Edwards School of Medicine, Huntington, USA 3. Internal Medicine, St. Mary's Medical Center, Huntington, USA Corresponding author: Deena Dahshan, [email protected] Abstract Introduction Due to high levels of intravenous drug use (IVDU) in West Virginia (WV), there are increasing numbers of hospitalizations for infective endocarditis (IE). More specifically, pregnant patients with IE are a uniquely challenging population, with complex management and a clinical course that further affects the health of the fetus, with high morbidity and mortality. Timely recognition and awareness of the most common bacterial causes will provide hospitals and clinicians with valuable information to manage future patients. Methods This retrospective study analyzed the clinical course of pregnant patients admitted with IE and IVDU history presenting at Cabell Huntington Hospital from 2013 to 2018. Inclusion criteria were women between 16 and 45 years of age confirmed to be pregnant by urine pregnancy test and ultrasonography with at least eight weeks gestation, with a first-time diagnosis of endocarditis and an identified history of IVDU. We excluded charts with pre-existing risk factors including a history of valvular disease, rheumatic heart disease, surgical valve repair or mechanical valve replacement, or a diagnosis of coagulopathies. The resulting charts were evaluated for isolated organisms, reported clinical course, and complications of the pregnancy. -
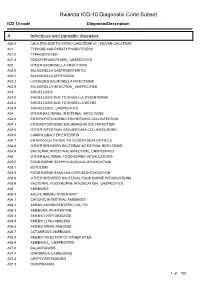
Rwanda ICD-10 Diagnostic Code Subset
Rwanda ICD-10 Diagnostic Code Subset ICD 10 code Diagnosis/Description A Infectious and parasitic diseases A00.0 CHOLERA DUE TO VIBRIO CHOLERAE 01_ BIOVAR CHOLERAE A01 TYPHOID AND PARATYPHOID FEVERS A01.0 TYPHOID FEVER A01.4 PARATYPHOID FEVER_ UNSPECIFIED A02 OTHER SALMONELLA INFECTIONS A02.0 SALMONELLA GASTROENTERITIS A02.1 SALMONELLA SEPTICEMIA A02.2 LOCALIZED SALMONELLA INFECTIONS A02.9 SALMONELLA INFECTION_ UNSPECIFIED A03 SHIGELLOSIS A03.0 SHIGELLOSIS DUE TO SHIGELLA DYSENTERIAE A03.2 SHIGELLOSIS DUE TO SHIGELLA BOYDII A03.9 SHIGELLOSIS_ UNSPECIFIED A04 OTHER BACTERIAL INTESTINAL INFECTIONS A04.0 ENTEROPATHOGENIC ESCHERICHIA COLI INFECTION A04.1 ENTEROTOXIGENIC ESCHERICHIA COLI INFECTION A04.4 OTHER INTESTINAL ESCHERICHIA COLI INFECTIONS A04.5 CAMPYLOBACTER ENTERITIS A04.7 ENTEROCOLITIS DUE TO CLOSTRIDIUM DIFFICILE A04.8 OTHER SPECIFIED BACTERIAL INTESTINAL INFECTIONS A04.9 BACTERIAL INTESTINAL INFECTION_ UNSPECIFIED A05 OTHER BACTERIAL FOOD-BORNE INTOXICATIONS A05.0 FOOD-BORNE STAPHYLOCOCCAL INTOXICATION A05.1 BOTULISM A05.4 FOOD-BORNE BACILLUS CEREUS INTOXICATION A05.8 OTHER SPECIFIED BACTERIAL FOOD-BORNE INTOXICATIONS A05.9 BACTERIAL FOOD-BORNE INTOXICATION_ UNSPECIFIED A06 AMEBIASIS A06.0 ACUTE AMEBIC DYSENTERY A06.1 CHRONIC INTESTINAL AMEBIASIS A06.2 AMEBIC NONDYSENTERIC COLITIS A06.3 AMEBOMA OF INTESTINE A06.4 AMEBIC LIVER ABSCESS A06.5 AMEBIC LUNG ABSCESS A06.6 AMEBIC BRAIN ABSCESS A06.7 CUTANEOUS AMEBIASIS A06.8 AMEBIC INFECTION OF OTHER SITES A06.9 AMEBIASIS_ UNSPECIFIED A07.0 BALANTIDIASIS A07.1 GIARDIASIS [LAMBLIASIS] -

Let's Talk About What's Hard
Let’s Talk About What’s Hard “Bobby” Duc Tran, MD, MSc Assistant Professor, Emory University 2017 HoG State Meeting Case Presentation March 3, 2017 WARNING The following presentation contains some foul language, nudity, and images that some viewers may find upsetting Case Presentation • 32yo white male • Past medical history: • severe hemophilia B • hemophilic arthropathy of bilateral knees and elbows • Marfan’s syndrome • atrial fibrillation • blind in one eye • hepatitis C • Current hemophilia treatment: Aprolix • Previous issues with mixing the factor. Case Presentation • Past surgeries: • Aortic root repair • Full dentition extraction • Bilateral knee arthroscopic synevectomies at 5 and 7 yo • Left orchiectomy for testicular torsion • Last seen in clinic for his annual comprehensive visit in 9/2016 Case Presentation • Called to the HTC clinic nurse on 12/5/2016 • Embarrassingly he reported: • This morning “my penis and testicles are blackish purple and feels like a bleed” • I had sex with my wife last night • Last infused 3 days ago and is not due for next infusion until tomorrow • “This has never happened before” How to talk about this? • Approach from a professional standpoint • Discuss these topics when discussing safe sexual practices • Gauge the patient’s comfort with using medical terms • Nicknames used: • Dick, dong, schlong, wiener, peen, so many more • Not wenis What to do first? • When was the bleeding recognized? • Did you hear/feel a “pop”? • Recognize associated injuries • Urethra, bladder, vascular • Consider GU referral -

Successful Treatment of Genital Pruritus Using Topical Immunomodulators As a Single Therapy in Multi-Morbid Patients
Letters to the Editor 195 Successful Treatment of Genital Pruritus Using Topical Immunomodulators as a Single Therapy in Multi-morbid Patients Elke Weisshaar Clinical Social Medicine, Occupational and Environmental Dermatology, University Hospital Heidelberg, Thibautstrasse 3, DE-69115 Heidelberg, Germany. E-mail: [email protected] Accepted October 29, 2007. Sir, origin. He had been suffering from arterial hyperten- Anogenital pruritus is defined as pruritus affecting the skin sion, recurrent back pain and occasional heartburn. of the anus, perianal and genital area. In men it frequently Various topical treatments, including glucocortico- presents as scrotal pruritus and in females as vulval steroids and pimecrolimus 1% cream, did not relieve his pruritus. It may be caused by skin diseases (e.g. eczema, scrotal pruritus. Because of the history of encephalitis psoriasis, irritant or allergic contact dermatitis), infections he rejected any further diagnostic tests and systemic (e.g. candidiasis, parasitosis, lichen sclerosus, prema- treatments and requested symptomatic relief. The lignant or malignant conditions), as well as by systemic scrotum showed mild lichenifications. Topical tacro- diseases. Age, especially in female patients, determines limus 0.03% was started twice daily and the pruritus the initial most common differential diagnoses that need resolved completely within 2 weeks (VAS 0). After 6 to be considered (1). Acute genital pruritus is often caused weeks he continued to apply tacrolimus 0.03% twice a by infections, allergic or irritant contact dermatitis, leading week for a further period of 8 weeks. He has now been to prompt resolution after causal therapy. In a number of almost free of pruritus for one year and uses tacrolimus patients no underlying disease can be identified and the approximately 3 applications a week every 2 months condition is termed “pruritus of undetermined origin”. -

Very Low Birth Weight Infants
Intensive Care Nursery House Staff Manual Very Low and Extremely Low Birthweight Infants INTRODUCTION and DEFINITIONS: Low birth weight infants are those born weighing less than 2500 g. These are further subdivided into: •Very Low Birth Weight (VLBW): Birth weight <1,500 g •Extremely Low Birth Weight (ELBW): Birth weight <1,000 g Obstetrical history (LMP, sonographic dating), newborn physical examination, and examination for maturational age (Ballard or Dubowitz) are critical data to differentiate premature LBW from more mature growth-retarded LBW infants. Survival statistics for ELBW infants correlate with gestational age. Morbidity statistics for growth-retarded VLBW infants correlate with the etiology and the severity of the growth-restriction. PREVALENCE: The rate of VLBW babies is increasing, due mainly to the increase in prematurely-born multiple gestations, in part related to assisted reproductive techniques. The distribution of LBW infants is shown in the Table: ________________________________________________________________________ Table. Prevalence by birth weight (BW) of LBW babies. Percentage of Percentage of Births Birth Weight (g) Total Births with BW <2,500 g <2,500 7.6% 100% 2,000-2,500 4.6% 61% 1,500-1,999 1.5% 20% 1,000-1,499 0.7% 9.5% 500-999 0.5% 7.5% <500 0.1% 2.0% ________________________________________________________________________ CAUSES: The primary causes of VLBW are premature birth (born <37 weeks gestation, and often <30 weeks) and intrauterine growth restriction (IUGR), usually due to problems with placenta, maternal health, or to birth defects. Many VLBW babies with IUGR are preterm and thus are both physically small and physiologically immature. RISK FACTORS: Any baby born prematurely is more likely to be very small. -

Diseases of the Digestive System (KOO-K93)
CHAPTER XI Diseases of the digestive system (KOO-K93) Diseases of oral cavity, salivary glands and jaws (KOO-K14) lijell Diseases of pulp and periapical tissues 1m Dentofacial anomalies [including malocclusion] Excludes: hemifacial atrophy or hypertrophy (Q67.4) K07 .0 Major anomalies of jaw size Hyperplasia, hypoplasia: • mandibular • maxillary Macrognathism (mandibular)(maxillary) Micrognathism (mandibular)( maxillary) Excludes: acromegaly (E22.0) Robin's syndrome (087.07) K07 .1 Anomalies of jaw-cranial base relationship Asymmetry of jaw Prognathism (mandibular)( maxillary) Retrognathism (mandibular)(maxillary) K07.2 Anomalies of dental arch relationship Cross bite (anterior)(posterior) Dis to-occlusion Mesio-occlusion Midline deviation of dental arch Openbite (anterior )(posterior) Overbite (excessive): • deep • horizontal • vertical Overjet Posterior lingual occlusion of mandibular teeth 289 ICO-N A K07.3 Anomalies of tooth position Crowding Diastema Displacement of tooth or teeth Rotation Spacing, abnormal Transposition Impacted or embedded teeth with abnormal position of such teeth or adjacent teeth K07.4 Malocclusion, unspecified K07.5 Dentofacial functional abnormalities Abnormal jaw closure Malocclusion due to: • abnormal swallowing • mouth breathing • tongue, lip or finger habits K07.6 Temporomandibular joint disorders Costen's complex or syndrome Derangement of temporomandibular joint Snapping jaw Temporomandibular joint-pain-dysfunction syndrome Excludes: current temporomandibular joint: • dislocation (S03.0) • strain (S03.4) K07.8 Other dentofacial anomalies K07.9 Dentofacial anomaly, unspecified 1m Stomatitis and related lesions K12.0 Recurrent oral aphthae Aphthous stomatitis (major)(minor) Bednar's aphthae Periadenitis mucosa necrotica recurrens Recurrent aphthous ulcer Stomatitis herpetiformis 290 DISEASES OF THE DIGESTIVE SYSTEM Diseases of oesophagus, stomach and duodenum (K20-K31) Ill Oesophagitis Abscess of oesophagus Oesophagitis: • NOS • chemical • peptic Use additional external cause code (Chapter XX), if desired, to identify cause.