Role of Avastin in Management of Diabetic Retinopathy Cataract
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
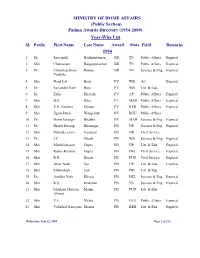
(Public Section) Padma Awards Directory (1954-2009) Year-Wise List Sl
MINISTRY OF HOME AFFAIRS (Public Section) Padma Awards Directory (1954-2009) Year-Wise List Sl. Prefix First Name Last Name Award State Field Remarks 1954 1 Dr. Sarvapalli Radhakrishnan BR TN Public Affairs Expired 2 Shri Chakravarti Rajagopalachari BR TN Public Affairs Expired 3 Dr. Chandrasekhara Raman BR TN Science & Eng. Expired Venkata 4 Shri Nand Lal Bose PV WB Art Expired 5 Dr. Satyendra Nath Bose PV WB Litt. & Edu. 6 Dr. Zakir Hussain PV AP Public Affairs Expired 7 Shri B.G. Kher PV MAH Public Affairs Expired 8 Shri V.K. Krishna Menon PV KER Public Affairs Expired 9 Shri Jigme Dorji Wangchuk PV BHU Public Affairs 10 Dr. Homi Jehangir Bhabha PB MAH Science & Eng. Expired 11 Dr. Shanti Swarup Bhatnagar PB UP Science & Eng. Expired 12 Shri Mahadeva Iyer Ganapati PB OR Civil Service 13 Dr. J.C. Ghosh PB WB Science & Eng. Expired 14 Shri Maithilisharan Gupta PB UP Litt. & Edu. Expired 15 Shri Radha Krishan Gupta PB DEL Civil Service Expired 16 Shri R.R. Handa PB PUN Civil Service Expired 17 Shri Amar Nath Jha PB UP Litt. & Edu. Expired 18 Shri Malihabadi Josh PB DEL Litt. & Edu. 19 Dr. Ajudhia Nath Khosla PB DEL Science & Eng. Expired 20 Shri K.S. Krishnan PB TN Science & Eng. Expired 21 Shri Moulana Hussain Madni PB PUN Litt. & Edu. Ahmed 22 Shri V.L. Mehta PB GUJ Public Affairs Expired 23 Shri Vallathol Narayana Menon PB KER Litt. & Edu. Expired Wednesday, July 22, 2009 Page 1 of 133 Sl. Prefix First Name Last Name Award State Field Remarks 24 Dr. -

University of Lucknow Undergraduate Admissions
UNIVERSITY OF LUCKNOW B.A. B.A. (Hons) UNDERGRADUATE ADMISSIONS 2016 OVERALL MERIT LIST Roll No Name Father Name DOB Gender CAT Sub Cat High School Test Marks Sports NCC Final Index Rank Cat Rank 1611610091 TANYA SALUJA H S SALUJA 12/03/1998 F General 86.33 266 0 0 266 1 1611140207 HIMANSHU SRIVASTAVA HARI MOHAN SRIVASTAVA 26/05/2001 M General 79.33 265 0 0 265 2 1611610351 VISHESH KUMAR YADAV SURESH CHANDRA YADAV 16/06/1998 M OBC 85.50 249 0 0 249 3 ÓBC-1 1611220018 SHAILJA CHAURASIA JAGDISH PRASAD CHAURASIA 27/08/1997 M OBC 94.20 245 0 0 245 4 ÓBC-2 1611110421 AANCHAL SAXENA SHYAM PRAKASH SAXENA 07/07/2000 F General 94.50 234 0 0 234 5 1611160412 RADHIKA GUPTA RAJEEV GUPTA 29/03/1998 F General 89.40 234 0 0 234 6 1611610013 SURAJ MEHROTRA DILIP MEHROTRA 05/12/1997 M General 89.83 233 0 0 233 7 1611160063 NITI PANDEY MOHAN CHANDRA PANDEY 02/11/1998 F General 89.50 233 0 0 233 8 1611160266 PRAPHULL AWASTHI MAYANK AWASTHI 30/11/1998 M General 86.00 233 0 0 233 9 1611150210 MANSI RAWAT HCS RAWAT 13/11/1998 F General 89.50 232 0 0 232 10 1611210257 SAKSHI SINGH GAMLESH KUMAR SINGH 10/12/1999 F General 93.00 231 0 0 231 11 1611150255 MEGHA MAJUMDAR OMKARESWAR MAJUMDAR 08/06/1997 F General 74.17 230 0 0 230 12 1611110482 ABHINAV KESHARI DURGA CHARAN PRASAD 19/07/1997 M General 95.00 228 0 0 228 13 1611160306 PRATEEKSHA SHRIVASTAVA BRIJENDRA NATH SHRIVASTAVA 29/01/1999 F General 94.83 228 0 0 228 14 1611130106 APARAJITA ANGAD PRASAD GUPTA 21/10/1998 F General 83.00 227 0 0 227 15 1611150214 MANSI VERMA SHIV SHANKAR VERMA 20/01/1999 F OBC 87.33 -

List of Fellows (Name-Wise) Upto 2016
LIST OF FELLOWS (NAME-WISE) UPTO 2016 0. Description Year 1. Abdul Kalam, A.P.J. Biomedical Engineering July 1995 DMIT. Former President, Republic of India. Res: 10 Rajaji Marg, New Delhi-110001. Permanent Address: No. 2, Mosque Street, Rameswaram, Ramanathapuram District, Tamil Nadu-623526. Tel: Off: (011) 3015321, 3014930, Res: (04567) 6493708, Fax: 2300756, E-mail: [email protected] (b 1931) (d.2015) Gen. Amir Chand Oration (NAMS, 1997-98) Padma Bhushan (1981); Padma Vibhushan (1990); Bharat Ratna (1997); D.Sc (h.c.) from several Universities; National Design Award; Dr. Biren Roy Space Award; Om Prakash Bhasin Award; National Nehru Award by Govt. of Madhya Pradesh; GM Modi Award for Science 1996; HK Firodia Award for Excellence in S&T 1996; Veer Savarkar Award 1998; Hon Fellow-Institution of Electronics and Telecommunication Engineers. 2. Abraham, Jacob Neurosurgery 1984 MS, MS (Neuro), FACS, FACA. Res: 10, 15th Avenue, Harrington Road, Chennai- 600031. Tel: Res: (044) 28363211, 42849258, Mobile: 09940118382, E-mail: [email protected] (b.1931). Basanti Devi Amir Chand Prize (ICMR, 1984); Sachs Memorial Lecturer, USA (1989). 3. Achari, Kamala Obstetrics and Gynecology 1982 MS, FRCOG, FICS, FACS. Emeritus Professor, Patna Medical College, Patna-800001 (Bihar). Res: 'Tirumalai', 21/D Road No.10, Rajendra Nagar, Patna- 800016. (b.1924) (d. 2014). 4. Adithan, C. Pharmacology July 2003 MD, PhD, FIMSA, FIPS. Former Professor & Head, Department of Pharmacology, Jawaharlal Institute of Postgraduate Medical Education & Research, Pondicherry- 605006. Currently: Director-CIDRF and Professor of Pharmacology, Mahatma Gandhi Medical College and Research Institute, Pondicherry-607403. Res: Flat No. 1, Srinivas Towers, Vazhudavour Road, Kathirkamam, Pondicherry-605009. -

PIO Notice SECL Exec List
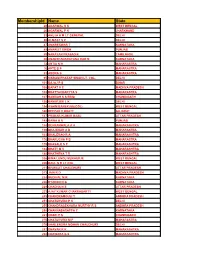
EMP_NAME Discipline Grade AREA KAMAL MOHAN BHATTACHARYA CHE M1 SECL HQ DEBASISH GUHA CHE E5 RAIGARH RADHA RAMAN NANDI CHE E5 BTG SURESH HARIBHAU DHUNDE CIV M2 SECL HQ DIWAKAR JHA CIV M2 SECL HQ M BHATTACHARJEE CIV M2 SECL HQ GOPAL CHANDRA DAS CIV M2 KORBA RAM PRASAD MUKHOPADHYAY CIV M1 KUSMUNDA SUDHIR KRISHNARAO BIDKAR CIV M1 SECL HQ RK SHRIVASTAVA CIV M1 SECL HQ GOVIND KUMAR SHARMA CIV M1 DIPKA ASHOKA NAND JHA CIV M1 SGP P RAVI SHANKER PRASAD CIV M1 SECL HQ LL KOSHLEY CIV M1 SECL HQ SUNIL KUMAR GARG CIV M1 SGP RABINDRA NATH DWIVEDI CIV M1 BSRMP NAWAL KISHORE CIV M1 SECL HQ DL JAIN CIV M1 HSD SANJAY KUMAR JHA CIV M1 BTG DILIP HARIHAR LIMSAY CIV M1 RAIGARH ABHAY KUMAR VERMA CIV M1 JOH BHASKAR SENGUPTA CIV M1 BSRMP SATINDRA KUMAR SHARMA CIV M1 CHRM SHAMBHOO SHARAN CIV M1 SECL HQ SAHENDRA KUMAR SINHA CIV M1 J&K BANASHRI NAIR SMT. CIV M1 SECL HQ SD PRASAD CIV M1 SECL HQ MRITYUNJAY KUMAR CIV E5 BTG MODI SATYENDRA KR. JAIN CIV E5 KORBA M KUPPUSWAMY CIV E5 BSRMP MD TANWEER ALAM CIV E5 SECL HQ M RAVI CHANDRA CIV E5 BKP MANOJ KUMAR CIV E5 DIPKA MADAN KUMAR JAIN CIV E5 JOH TAPAS KUMAR SARKAR CIV E5 KORBA SN PRASAD CIV E5 CHRM MANOJ KUMAR CIV E5 DIPKA SYED VILAYATULLAH CIV E5 CHRM T JEEVAN CIV E5 J&K MA BAIG CIV E5 DIPKA KAMESHWAR SINGH CIV E5 KUSMUNDA DR SINGH CIV E5 SGP DULICHAND AGRAWAL CIV E5 GEVRA EKHLAKH AHMED SIDDIQUI CIV E5 BTG GAJANAN CHAURASIA CIV E5 SECL HQ GB DAMODHARAN CIV E5 SGP GOPAL PATEL CIV E5 JOH GOVIND PRASAD AGRAWAL CIV E5 SECL HQ HN TIWARI CIV E5 HSD JEET BANDHAN CIV E5 CHRM KN BHARADWAJ CIV E5 GEVRA KAMESH PRASAD GUPTA CIV E5 BKP LAXMAN SINGH CIV E5 JOH KAMLESH KUMAR SINGH CIV E5 SGP KD MUKHERJEE CIV E5 SECL HQ KIRTI TIWARI SMT. -
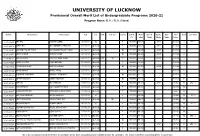
UNIVERSITY of LUCKNOW Provisional Overall Merit List of Undergraduate Programs 2020-21 Program Name: B.A
UNIVERSITY OF LUCKNOW Provisional Overall Merit List of Undergraduate Programs 2020-21 Program Name: B.A. / B.A. (Hons) Roll No. Student Name Father's Name DoB Cat. EWS Sub Cat. Gender INTER Merit NCC 'B' Sports Girls Final Rank Cat. Rank (%) Index Marks Marks Marks Index 20201000649 ARTI RAJ SURESH KUMAR 08/07/2001 SC F 96.800 96.800 4.840 101.640 1 SC - 1 20201062313 SMRITI RAI MR. KABINDRA NARAIN RAI 11/08/2001 General F 96.600 96.600 4.830 101.430 2 20201019761 TANISHQ PRATAP SINGH SAVITENDRA PRATAP SINGH 23/06/2000 General M 93.600 96.495 4.825 101.320 3 20201004674 ADNAN AHMED NAFEES AHMED 22/01/2000 General M 95.400 96.364 4.818 101.182 4 20201036035 AASTHA SINGH RAJESH KUMAR SINGH 06/12/2002 General EWS DP F 95.000 95.960 4.798 100.758 5 20201049267 NOORIA FATIMA NADEEM KAZMI 13/02/2002 General F 99.600 100.606 100.606 6 20201000936 PRIYANSH MISHRA AKHILESH KUMAR 02/07/2002 General M 94.800 95.758 4.788 100.546 7 20201016128 NAYAB SHAMS SHAMS JAMAL 21/05/2000 General F 100.000 100.000 100.000 8 20201021003 AISHANYA UPADHYAY SHARDUL UPADHYAY 20/11/2002 General M 100.000 100.000 100.000 9 20201021516 ADITYA VASHISHT ASHISH VASHISHT 07/06/2003 General M 99.000 100.000 100.000 10 20201033060 VARSHA MR. RAMNATH 03/08/2003 OBC(NCL) F 95.200 95.200 4.760 99.960 11 OBC - 1 20201033987 ISHA TRIPATHI AJAY KUMAR TRIPATHI 29/08/2002 General F 98.833 99.831 99.831 12 20201018325 SHLAGHYA MISHRA SHIVENDRA KUMAR MISRA 01/07/2002 General F 99.600 99.600 99.600 13 20201026682 AASTHIKA NARAYAN SHYAM NARAYAN 19/01/2003 SC F 98.600 99.596 99.596 -
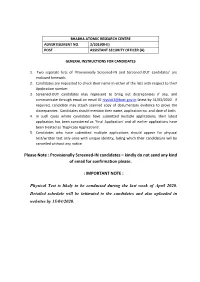
Please Note : Provisionally Screened-IN Candidates – Kindly Do Not Send Any Kind of Email for Confirmation Please
BHABHA ATOMIC RESEARCH CENTRE ADVERTISEMENT NO. 2/2019(R-II) POST ASSISTANT SECURITY OFFICER (A) GENERAL INSTRUCTIONS FOR CANDIDATES 1. Two separate lists of ‘Provisionally Screened-IN and Screened-OUT candidates’ are enclosed herewith. 2. Candidates are requested to check their name in either of the lists with respect to their Application number. 3. Screened-OUT candidates may represent to bring out discrepancies if any, and communicate through email on email ID [email protected] latest by 31/03/2020. If required, candidate may attach scanned copy of documentary evidence to prove the discrepancies. Candidates should mention their name, application no. and date of birth. 4. In such cases where candidates have submitted multiple applications, their latest application has been considered as ‘Final Application’ and all earlier applications have been treated as ‘Duplicate Applications’. 5. Candidates who have submitted multiple applications should appear for physical test/written test only once with unique identity, failing which their candidature will be cancelled without any notice. Please Note : Provisionally Screened-IN candidates – kindly do not send any kind of email for confirmation please. : IMPORTANT NOTE : Physical Test is likely to be conducted during the last week of April 2020. Detailed schedule will be intimated to the candidates and also uploaded in websites by 15/04/2020. List of candidates provisionally Screened - IN for the post of Assistant Security Officer (A) against advertisement No. 02/2019(R-II) Sl No Appl No Title -
Unregistered/Unreachable Members List
MembershipId Name State 20 AGARWAL S K WEST BENGAL 26 AGARWAL P K JHARKHAND 33 AHUJA A M LT GENERAL DELHI 39 ALMAST S C DELHI 47 AMARESWAR T KARNATAKA 48 AMARJIT SINGH PUNJAB 59 NARAYAN PRASAD K TAMILNADU 60 ANANTHANARAYANA RAO N KARNATAKA 72 ANTIA N H MAHARASTRA 76 APTE B P MAHARASTRA 83 ARORA S MAHARASTRA 95 VIKRAM PRATAP SINGH LT. COL. DELHI 101 BAJAJ P S BIHAR 108 BAPAT V C MADHYA PRADESH 109 BHATTACHARYYA S MAHARASTRA 127 BAMRAH N S BRIG CHANDIGARH 130 BANERJEE L K DELHI 134 ASHIM BANERJEE(COL) WEST BENGAL 140 DEEPAK V BHATT GUJARAT 147 PRANAB KUMAR BASU UTTAR PRADESH 149 BAWA H S PUNJAB 154 BEHRANWALA A A MAHARASHTRA 159 BHAJEKAR A B MAHARASTRA 163 BHALERAO R A MAHARASHTRA 176 BHARUCHA P B MAHARASTRA 179 BHASALE S P MAHARASHTRA 184 BHATT M V MAHARASHTRA 188 BHATHENA T R MAHARASHTRA 206 BIMA LENDU MUKHERJE WEST BENGAL 209 BAUL N R LT COL WEST BENGAL 211 BISWAJIT CHAUDHURI UTTAR PRADESH 213 JAIN R D MADHYA PRADESH 224 BUDIHAL M R KARNATAKA 226 BYAKOD N G KARNATAKA 229 CHADHA N S UTTAR PRADESH 233 AJAY KUMAR CHAKRABARTY WEST BENGAL 249 CHANDRAMOULI Y ANDHRA PRADESH 251 CHATURVEDI P K DELHI 255 CHANDRASEKHARA MURTHY R S ANDHRA PRADESH 258 CHANNABASAPPA C KARNATAKA 261 CHARI P S CHANDIGARH 275 CHATURVEDI M P MAHARASTRA 279 SHAILENDRA MOHAN CHAUDHURI DELHI 287 CHAVAN R K MAHARASHTRA 288 CHAWARA G S MAHARASHTRA 301 CHINNASWAMI C TAMIL NADU 309 YOG D K UTTAR PRADESH 324 PRAKASH RAO S R K TELANGANA 325 DAS M M WEST BENGAL 326 DAS P B ANDHRA PRADESH 339 DATTA A P WEST BENGAL 342 DAULAT RAM J MAHARASTRA 343 SHERE P M MAHARASTRA 345 DAVER B -

R1a2 11March2013.Pdf
List of Applicants applied for registration in Gokul Gram Yojna (Bibi-Khera), Lucknow sch_cd age aplcnt_nm form_no pmt_mode pty_cat_cd REGS_AMT_DEP resv_cat_cd sex annual_income_cd father_nm spouse_nm Hor_Rev_Cat PTY_TYP sch_name pty_cat_desc COMMENTS 223 30 SANTOSH KUMAR 39425 1 R1A2 14000 1 M 4 PARAGI LAL NA-[Not Available] Plot Gokul Gram Yojna-II(Bibi Khera) 51-80 SQ. M 223 40 KRASHNA KUMAR GUPTA 14426 1 R1A2 14000 3 M 4 GANGA PRASAD NA-[Not Available] Plot Gokul Gram Yojna-II(Bibi Khera) 51-80 SQ. M receipt of cast certificate held 223 32 VINOD KUMAR SINGH 15772 2 R1A2 28000 4 M 4 VIJAY PRATP SINGH NA-[Not Available] Plot Gokul Gram Yojna-II(Bibi Khera) 51-80 SQ. M CERTIFICATE OF G NOT HELD 223 53 CHINTA YADAV 15780 1 R1A2 14000 3 F 4 KOMAL PRASAD YADAV KOMAL PRASAD YADAV NA-[Not Available] Plot Gokul Gram Yojna-II(Bibi Khera) 51-80 SQ. M 223 37 SHACHI RASTOGI 18061 1 R1A2 14000 3 F 4 SURESH KUMAR SURESH KUMAR NA-[Not Available] Plot Gokul Gram Yojna-II(Bibi Khera) 51-80 SQ. M CAST CERTIFICATE OF HUSBAND HELD 223 32 GAURAV PANT 34143 2 R1A2 28000 4 M 4 LALIT CHANDRA PANT RICHA PANT NA-[Not Available] Plot Gokul Gram Yojna-II(Bibi Khera) 51-80 SQ. M 223 26 MAHENDRA KUMAR 21071 1 R1A2 14000 3 M 4 BANWARI LAL PRAJAPATI NA-[Not Available] Plot Gokul Gram Yojna-II(Bibi Khera) 51-80 SQ. M 223 30 RAJ KUMAR PRAJAPATI 21391 2 R1A2 14000 3 M 4 RAM JANM PRAJAPATI SHOBHA PRAJAPATI NA-[Not Available] Plot Gokul Gram Yojna-II(Bibi Khera) 51-80 SQ. -
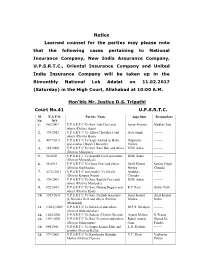
Notice Learned Counsel for the Parties May Please Note That the Following
Notice Learned counsel for the parties may please note that the following cases pertaining to National Insurance Company, New India Assurance Company, U.P.S.R.T.C., Oriental Insurance Company and United India Insurance Company will be taken up in the Bimonthly National Lok Adalat on 11.02.2017 (Saturday) in the High Court, Allahabad at 10:00 A.M. Hon'ble Mr. Justice D.S. Tripathi Court No.41 U.P.S.R.T.C. Sl. F.A.F.O. Parties Name Appellant Respondent No. NO. 1. 966/2003 U.P.S.R.T.C Vs Smt. Atto Devi and Samir Sharma Madhav Jain others (District Agra) 2. 395/2012 U.P.S.R.T.C Vs Tikori Chaudhary and Ajay Singh -------- others (District Basti) 3. 4077/2012 U.P.S.R.T.C Vs Sagir Ahmad @ Babu Nripendra -------- and another (District Bareilly) Mishra 4. 385/2000 U.P.S.R.T.C Vs Smt. Rani Beti and others M.M. Sahai -------- (District Mainpuri) 5. 20/2009 U.P.S.R.T.C Vs Saurabh Goel and others M.M. Sahai -------- (District Moradabad) 6. 58/2015 U.P.S.R.T.C Vs Geeta Devi and others Sunil Kumar Sanjay Singh (District Sonbhadra) Mishra Chandel 7. (671)/2011 U.P.S.R.T.C and another Vs Sheelu Anubhav ------- (District Kanpur Nagar) Chandra 8. 378/2005 U.P.S.R.T.C Vs Smt. Sushila Devi and M.M. Sahai -------- others (District Mainpuri) 9. 972/2012 U.P.S.R.T.C Vs Smt. Mehraj Begum and R.P. -

Eligible Voter's List
Sl.No ASI ID Name State 1 10 BHAT K L DELHI 2 13 ADINARAYANA RAO S V ANDHRA PRADESH 3 20 AGARWAL S K WEST BENGAL 4 22 AGARWAL Y M HARYANA 5 26 AGARWAL P K JHARKHAND 6 32 AHMAD ABDUL HAI BIHAR 7 33 AHUJA A M LT GENERAL DELHI 8 35 SINGHVI A M RAJASTHAN 9 39 ALMAST S C DELHI 10 46 AMARESH BHASKAR NALLAVANDU AIR MSHL KARNATAKA 11 47 AMARESWAR T KARNATAKA 12 48 AMARJIT SINGH PUNJAB 13 49 AMBIKE V S MAHARASTRA 14 55 ANAND PRAKASH UTTAR PRADESH 15 58 ANANTHAKRISHNAN L TAMIL NADU 16 59 NARAYAN PRASAD K TAMILNADU 17 60 ANANTHANARAYANA RAO N KARNATAKA 18 72 ANTIA N H MAHARASTRA 19 76 APTE B P MAHARASTRA 20 79 ARCANJO DE MENESES GOA 21 83 ARORA S MAHARASTRA 22 91 ASOPA H S UTTAR PRADESH 23 95 VIKRAM PRATAP SINGH LT. COL. DELHI 24 101 BAJAJ P S BIHAR 25 108 BAPAT V C MADHYA PRADESH 26 109 BHATTACHARYYA S MAHARASTRA 27 118 KRISHNA HANDE H TAMIL NADU 28 123 BALLAL C R KARNATAKA 29 127 BAMRAH N S BRIG CHANDIGARH 30 130 BANERJEE L K DELHI 31 131 BANERJEE S WEST BENGAL 32 134 ASHIM BANERJEE(COL) WEST BENGAL 33 138 BAPAT S D MAHARASHTRA 34 140 DEEPAK V BHATT GUJARAT 35 147 PRANAB KUMAR BASU UTTAR PRADESH 36 149 BAWA H S PUNJAB 37 153 BEHERA D K ODISHA 38 159 BHAJEKAR A B MAHARASTRA 39 161 BAKTHAVATSALAM G TAMIL NADU 40 163 BHALERAO R A MAHARASHTRA 41 170 BHANUSHALI H S MAHARASTRA 42 176 BHARUCHA P B MAHARASTRA 43 179 BHASALE S P MAHARASHTRA 44 184 BHATT M V MAHARASHTRA 45 188 BHATHENA T R MAHARASHTRA 46 189 JAGDISHWER BHATT RAJASTHAN 47 195 SINGARAJU KRISHNA PRABHAKAR TELANGANA 48 199 RAVIKANTH C BANGALORE KARNATAKA 49 200 BHAKTA V P MAHARASTRA 50 206 BIMA -

10+ 2 (Tes-36) Jan 2017 Cut Off Pcm : 87% & Above
ALLOTMENT OF CENTRE :10+ 2 (TES-36) JAN 2017 CUT OFF PCM : 87% & ABOVE Sl No. RollNo CandidateName FatherName Centre 1 100001 AYUSH TRIPATHI HANUMAN PRASAD Allahabad 2 100007 PRAPHULL AWASTHI MAYANK AWASTHI Allahabad 3 100008 DEVESH CHAUDHARY DHARAMVEER CHAUDHARY Allahabad 4 100025 SIKANDAR WASEEM WASEEM HASAN Allahabad 5 100030 VIVEK SINGH VIKRAM PRATAP SINGH Allahabad 6 100035 MOHIT TIWARI DAYA SHANKAR TIWARI Allahabad 7 100089 AKHILESH KUMAR SUNIL KUMAR YADAV Allahabad 8 100099 PUNIT KUMAR SHUKLA RAJ KISHOR SHUKLA Allahabad 9 100128 KUNWAR ABHINAV RATHAUR K G S RATHAUR Allahabad 10 100151 SAGAR GOSWAMI HARIOM GOSWAMI Allahabad 11 100185 SOHIT SIWAL ANIL SINGH Allahabad 12 100187 SANJAY KUMAR UMASHANKER YADAV Allahabad 13 100189 ASHUTOSH KUMAR TULSI RAM BIND Allahabad 14 100193 ASHISH KUMAR KUSHWAHA JAGADISH NARAYAN Allahabad 15 100196 ANKIT UNIYAL MANMOHAN UNIYAL Allahabad 16 100209 TARUN RAJ YADAV MUKUT SINGH YADAV Allahabad 17 100211 GAURAV PANDEY RAJESH KUMAR PANDEY Allahabad 18 100221 NISHU KUMAR OM KUMAR Allahabad 19 100222 AMIT YADAV VIRENDAR YADAV Allahabad 20 100251 NIKHIL PANDEY RAVI KUMAR PANDEY Allahabad 21 100256 SHUBHAM GUPTA SHAILESH KUMAR GUPTA Allahabad 22 100262 SATYAM PAL SANJAY PAL Allahabad 23 100283 SHUBHAM KUMAR SINGH RADHESHYAM SINGH Allahabad 24 100306 SAGAR PUNDIR SANJEEV KUMAR Allahabad 25 100337 VISHAL DAGAR VINOD DAGAR Allahabad 26 100365 CHANDAN MAURYA RAJESH MAURYA Allahabad 27 100371 ANANT KUMAR VIPIN KUMAR Allahabad 28 100380 RAJ SINGH CHAUHAN JITENDRA SINGH CHAUHAN Allahabad 29 100389 ANUJ SACHAN VINOD -

No.A.23011/2/2019-CHS-III Government of India Ministry of Health & Family Welfare (CHS DIVISION)
No.A.23011/2/2019-CHS-III Government of India Ministry of Health & Family Welfare (CHS DIVISION) Nirman Bhawan, New Delhi, Dated: 17 June, 2019 OFFICE MEMORANDUM Sub: Draft Seniority List of Teaching Specialists Sub-cadre of Central Health Service as on 01.04. 2019. The undersigned is directed to enclose herewith a copy of draft Seniority List of the Teaching Specialists Sub-cadre of Central Health Service as on 01.04.2019. 2. All efforts have been made to make this list /database as authentic as possible. However, the officers concerned are requested to bring to the notice of this Ministry the errors/omissions and objections, if any, within one month from the date of issue of this Office Memorandum. Other-wise, particulars given in the enclosed list will be assumed to be correct. — 24-2a1/ (C.S. Bahuguna) Under Secretary to the Government of India Telefax No.23061875 to The Secretary (Health), Health & FW Deptt. Govt. of NCT of Delhi, Delhi Sachivalaya, I P Estate, New Delhi. The Dean, Maulana Azad Medical College, 2-Bahadur Shah Zafar Road, New Delhi. The Director, G B Pant Hospital, New Delhi. The Medical Superintendent, Guru Teg Bahadur Hospital, Dilshad Garden, New Delhi. The Medical Superintendent, Safdarjung Hospital, New Delhi. The Director, Lady Hardinge Medical College, New Delhi. The Medical Superintendent, Dr. RML Hospital, New Delhi. The Director, All India Institute of Hygiene & Public Health, 110 Chittaranjan Avenue, Kolkata- 700073. The Director, Central Institute of Psychiatry, Ranchi. The Director, All India Institute of Physical Medicine & Rehabilitation, Hazi Ali Park, K. Ahadye Marg, Mahalaxmi, Mumbai-400034.