E-FILED Wednesday, 01 July, 2020 04:24:16 PM Clerk, U.S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

WHERE Do WE STAND on UPC IMPLEMENTATION
WHERE Do WE STAND ON UPC IMPLEMENTATION by Tom Wilson Vice President, McKinsey & Co. New York, New York I. Four topics will be discussed 2. Source symbol marking A. Status against program goals - Grocery manufacturers B. Public policy issues - Retailers (private - Price mark legislation label) - Labor union position 3. Availability of equipment c. Recent code council actions D. Open issues IV. Code conversion membership in UPCC II. Key dates in UPC development 1966 - Kroger Technology Conference 1975 Cumula- 1969 - IMS Test Installation to tive 1970 - AD HOC Committee formed 1972 1973 1974 Date Total (8/70) Manufac- 1971 - Code Selection Announced turers 209 578 1582 1284 3653 (5/71) 1972 - Code Council Formed (3/72) Retailers 84 62 58 24 228 First Number Issues (5/72) —— —— First U.S. Scanner Test 293 640 1640 1308 3881 (7/72) 1973 - Symbol Selection Announced (4/73) v. Source symbol marking Symbol Specifications Pub- A. Goal was to have 50 percent of lished (5/73) nonvariable weight items First UPC Scanner Announced source marked by year-end 1974, (10/73) 75 percent by year-end 1975. 1974 - First UPC Scanner Installed 1. Percentages are on all (6/74) commodity item movement 1975 - 50 Percent Source Symbol basis. Marking (5/75) 2. 50 percent source mark was First Price Mark Legislation economic break-even. (6/75) B. Progress by manufacturers judged sufficient to meet these III. Status against goals goals. A. Three basic measurers of UPC 1. Testing chains report 55-65 implementation percent level on shelf 1. Code conversion 2. Nielsen audit shows 58 - Membership in UGPCC percent in July - Use on shippers, paper work February 76/page 96 Journal of Food Distribution Researck VI, Percentage of items with UPC VIII. -

Freson Bros. Stony Plain AB Bobs' IGA Wrangell AK City Market, Inc
NGA Retail Membership List by State – Summer 2018 Company City State Freson Bros. Stony Plain AB Bobs' IGA Wrangell AK City Market, Inc. Wrangell AK Copper Valley IGA Glennallen AK Country Foods IGA Kenai AK Cubby's Marketplace IGA Talkeetna AK Fairway Market, IGA Skagway AK Hames Corporation dba Sea Mart Quality Foods Sitka AK Howsers Supermarket IGA Haines AK IGA Food Cache Delta Junction AK Tatsuda's IGA Ketchikan AK Trading Union IGA Petersburg AK A & R Supermarkets, Inc. dba Sav Mor Calera AL Autry Greer & Sons, Inc. Mobile AL Baker Foods, Inc. dba Piggly Wiggly Pell City AL Big Bear of Luverne, Inc. dba Super Foods Supermarkets Luverne AL Farmers IGA Foodliner Opp AL Forster & Howell, Inc. dba Grocery Outlets Dothan AL Fourth Avenue Supermarket Inc. dba Four Winds Fine Foods Bessemer AL Freeman Foods Inc. dba Freeman's Shur-Valu Foods Dothan AL Gregerson's Foods, Inc. dba Gregerson's Foods Gadsden AL Hackleburg Market Hackleburg AL Holley Oil Company Wetumpka AL Hopper Family Market Cullman AL Johnson's Giant Food, Inc. Altalla AL Langley Inc. Hayneville AL M&B Enterprises dba Fuller's Supermarket Greensboro AL Piggly Wiggly - Warrior, AL Russell Supermarket, Inc. Warrior AL Pinnacle Foods Mobile AL Ragland Bros. Retail Co. Inc. Huntsville AL Shan Bruce Enterprises, Inc. dba Foodland Fort Payne AL Tallassee Super Foods Tallassee AL Western Supermarkets, Inc. Birmingham AL Williams-McGue Inc. dba WM Grocery Wedowee AL Wrights Markets Opelika AL Bill's Fresh Market Jonesboro AR Cash Saver Russellville AR Cranford's Fresh World White Hall White Hall AR Dale Newman Management Co. -

Prices and Profits of Leading Retail Food Chains, 1970-74
K76 PRICES AND PROFITS OF LEADING RETAIL FOOD CHAINS, 1970-74 HEARINGS BEFORE THE JOINT ECONOMIC COMMITTEE CONGRESS OF THE UNITED STATES NINETY-FIFTH CONGRESS FIRST SESSION MARCH 30 AND APRIL 5, 1977 Printed for the use of the Joint Economic Committee U.S. GOVERNMENT PRINTING OFFICE 96-514 WASHINGTON: 1977 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, D.C. 20402 , It. I4 JOINT ECONOMIC COMMITTEE (Created pursuant to sec. 5(a) of Public Law 304, 79th Cong.) RICHARD BOLLING, Missouri, Chairman HUBERT H. HUMPHREY, Minnesota, Vice Chairman HOUSE OF REPRESENTATIVES SENATE HENRY S. REUSS, Wisconsin JOHN SPARKMAN, Alabama WILLIAM S. MOORHEAD, Pennsylvania WILLIAM PROXMIRE, Wisconsin LEE H. HAMILTON, Indiana ABRAHAM RIBICOFF, Connecticut GILLIS W. LONG, Louisiana LLOYD BENTSEN, Texas OTIS G. PIKE, New York EDWARD M. KENNEDY, Massachusetts CLARENCE J. BROWN, Ohio JACOB K. JAVITS, New York GARRY BROWN, Michigan WILLIAM V. ROTH, JR., Delaware MARGARET M. HECKLER, Massachusetts JAMES A. McCLURE, Idaho JOHN H. ROUSSELOT, California ORRIN G. HATCH, Utah JOHN R. STARK, Executive Director Louts C. KRAUTHOFF II, Assistant Director RICHARD F. KAUFMAN, General Counsel ECONOMISTS WILLIAm R. BUECHNER KENT H. HUGHES PHILIP MCMARTIN G. THOMAS CATOR SARAH JACKSON GEORGE R. TYLER WILLIAM A. Cox JOHN R. KARLIK ROBERT D. HAMRIN L. DOUGLAS LEE MINoarIY CHARLES H. BRADFORD STEPHEN J. ENTIN GEORGE D. KRuMSHAAR, Jr. M. CATHERINE MILLER MARE R. POLICINSEI (II) -CONTENTS WITNESSES AND STATEMENTS WEDNESD-AY, MARCH 30,41977 Long, Hon. Gillis W., cochairperson, member of the Joint Economic Com- Page mittee: Opening statement - - 1 Heckler, Hon. Margaret M., cochairperson, member of the Joint Economic Committee: Opening statement--____________-__-_-_-_-__-__-_ 3 Mueller, Willard F., and Bruce W. -

United States Et Al. V. Supervalu, Inc. Et Al., NO. 11-3290
United States et al. v. Supervalu, Inc. et al. 2019 WL 6112839 (C.D. Ill. 2019) ediscoveryassistant.com UNITED STATES OF AMERICA, and THE STATES OF CALIFORNIA, DELAWARE, ILLINOIS, INDIANA, MASSACHUSETTS, MINNESOTA, MONTANA, NEVADA, NEW JERSEY, NORTH CAROLINA, RHODE ISLAND, VIRGINIA, ex rel. TRACY SCHUTTE and MICHAEL YARBERRY, Plaintiffs and Relators, v. SUPERVALU, INC., SUPERVALU HOLDINGS, INC., FF ACQUISITIONS, LLC, FOODARAMA, LLC, SHOPPERS FOOD WAREHOUSE CORP., SUPERVALU PHARMACIES, INC., ALBERTSON'S LLC, JEWEL OSCO SOUTHWEST LLC, NEW ALBERTSON'S INC., AMERICAN DRUG STORES, LLC, ACME MARKETS, INC., SHAW'S SUPERMARKET, INC., STAR MARKET COMPANY. INC., JEWEL FOOD STORES, INC., and AB ACQUISITION LLC, Defendants NO. 11-3290 United States District Court, C.D. Illinois Nov 18, 2019 Mills, Richard H., United States District Judge OPINION *1 Pending is the Relators' motion for sanctions. In their reply brief, the Relators also request an in camera review of Defendants' litigation holds. I. The Relators seek the entry of an Order imposing appropriate sanctions against the Defendants for what they allege is (1) Defendants' failure to timely issue a litigation hold; (2) the intentional destruction of material evidence relating to Defendants' price match program; and (3) their subsequent efforts to conceal and obstruct discovery of their spoliation of evidence, including the wrongful withholding of material evidence of the spoliation until just days before the close of discovery in this case. The Defendants claim (1) they timely issued a litigation hold in this matter; (2) did not intentionally destroy material evidence; and (3) did not attempt to conceal and obstruct discovery of any alleged spoliation of evidence. -

NGA Retail Membership List by State – Winter 2019
NGA Retail Membership List by State – Winter 2019 Company City State A & R Super Markets, Inc. Calera Alabama Autry Greer & Sons Inc Mobile Alabama Baker Foods, Inc. Pell City Alabama Bruce Management, Inc. Fort Payne Alabama Farmers IGA Foodliner Opp Alabama Food Giant, Inc. Bessemer Alabama Forster & Howell Inc Dothan Alabama Fourth Avenue Supermarket Bessemer Alabama Freeman's Shur-Valu Foods Dothan Alabama Fuller's Supermarket Greensboro Alabama Gateway Foodland Inc Double Spgs Alabama Gregerson's Foods, Inc. HQ Gadsden Alabama Holley Oil Company Wetumpka Alabama Johnson's Giant Food, Inc. Attalla Alabama Piggly Wiggly Warrior Alabama Pinnacle Foods dba Save A Lot Mobile Alabama Ragland Bros Retail Co's, Inc. Huntsville Alabama Renfroe, Inc. Montgomery Alabama Star Super Market, Inc. Huntsville Alabama Tallassee Super Foods Tallassee Alabama Western Supermarkets, Inc Birmingham Alabama Wright's Markets, Inc. Opelika Alabama Benjamin's IGA Wrangell Alaska City Market, Inc. Wrangell Alaska Copper Valley IGA Glennallen Alaska Country Foods IGA Kenai Alaska Cubbys Marketplace IGA Talkeetna Alaska Fairway Market IGA Skagway Alaska Hames Corporation Sitka Alaska Howsers IGA Supermarket Haines Alaska IGA Food Cache Delta Junction Alaska Tatsudas IGA Ketchikan Alaska Trading Union IGA Market Petersburg Alaska Freson Bros. Stony Plain Alberta Rodney's Supermarket Arima Arima Del Sol IGA #6 San Luis Arizona Ed's IGA Market Snowflake Arizona El Rancho Market IGA Chandler Arizona Food Town IGA Eloy Arizona Garrett's IGA Supermarket Rio Rico Arizona Norms IGA Kearny Arizona Olsens IGA Market Yuma Arizona RCCM Foodtown IGA Market Eloy Arizona Shopes Market IGA Coolidge Arizona The Butcher & The Farmer Marketplace IGA Buckeye Arizona Tonto Basin Market Place IGA Tonto Basin Arizona Wilburs IGA Market Saint Johns Arizona Cranford's Fresh World Little Rock Arkansas Cranford's Fresh World dba FoodWise Hot Springs Village White Hall Arkansas Cranford's Fresh World dba ShopWise Redfield Redfield Arkansas Cranford's Fresh World, Rison Rison Arkansas Dale Newman Management Co. -

Agenda - Council Meeting - Tuesday - April 3, 2007 - 1:30 P
AGENDA - COUNCIL MEETING - TUESDAY - APRIL 3, 2007 - 1:30 P. M. COUNCIL CHAMBER - SECOND FLOOR - CITY HALL 901 BAGBY - HOUSTON, TEXAS PRAYER AND PLEDGE OF ALLEGIANCE - Council Member Garcia 1:30 P. M. - ROLL CALL ADOPT MINUTES OF PREVIOUS MEETING 2:00 P. M. - PUBLIC SPEAKERS - Pursuant to City Council Rule 8, City Council will hear from members of the public; the names and subject matters of persons who had requested to speak at the time of posting of this Agenda are attached; the names and subject matters of persons who subsequently request to speak may be obtained in the City Secretary’s Office 5:00 P. M. - RECESS RECONVENE WEDNESDAY - APRIL 4, 2007 - 9:00 A. M. DESCRIPTIONS OR CAPTIONS OF AGENDA ITEMS WILL BE READ BY THE CITY SECRETARY PRIOR TO COMMENCEMENT MAYOR’S REPORT 9:00 A.M. - REPORT FROM CITY CONTROLLER AND THE CITY ADMINISTRATION REGARDING THE CURRENT FINANCIAL STATUS OF THE CITY including but not limited to, a revenue, expenditure and encumbrance report for the General Fund, all special revenue funds and all enterprise funds, and a report on the status of bond funds CONSENT AGENDA NUMBERS 1 through 37 AGENDA - APRIL 4, 2007 - PAGE 2 MISCELLANEOUS - NUMBERS 1 and 2 1. RECOMMENDATION from Director Finance & Administration Department to authorize and grant a waiver of certain requirements under the City of Houston Ordinance No. 97-416 with respect to the terms and conditions of certain refunding bonds to be issued by BEECHNUT MUNICIPAL UTILITY DISTRICT 2. RECOMMENDATION from Director Department of Public Works & Engineering for payment of $1,012,146.00 permit fees to the HARRIS-GALVESTON SUBSIDENCE DISTRICT for Permit Year 2007 aggregated Ground Water Withdrawal and accrual of Over-Conversion Credits Enterprise Fund DAMAGES - NUMBER 3 3. -

Pasadena Independent School District
PASADENA INDEPENDENT SCHOOL DISTRICT Meeting of the Board of Trustees Tuesday, September 27, 2011, at 6:00 P.M. AGENDA The Pasadena Independent School District Board of Trustees Personnel Committee will meet in Room L101 of the Administration Building, 1515 Cherrybrook, Pasadena, Texas on Tuesday, September 27, 2011, at 6:00 P.M. I. Convene in a Quorum and Call to Order; Invocation; Pledge of Allegiance II. Adjournment to closed session pursuant to Texas Government Code Section 551.074 for the purpose of considering the appointment, employment, evaluation, reassignment, duties, discipline or dismissal of a public officer, employee, or to hear complaints or charges against a public officer or employee. III. Reconvene in Open Session IV. Adjourn The Pasadena Independent School District Board of Trustees Policy Committee will meet in the Board Room of the Administration Building, 1515 Cherrybrook, Pasadena, Texas on Tuesday, September 27, 2011, at 6:00 P.M. I. Convene into Open Session II. Discussion regarding proposed policies III. Adjourn 1 The Board of Trustees of the Pasadena Independent School District will meet in regular session at the conclusion of any committee meetings on Tuesday, September 27, 2011, in the Board Room of the Administration Building, 1515 Cherrybrook, Pasadena, Texas. A copy of items on the agenda is attached. I. Convene in a Quorum and Call to Order THE SUBJECTS TO BE DISCUSSED OR CONSIDERED OR UPON WHICH ANY FORMAL ACTION MIGHT BE TAKEN ARE AS FOLLOWS: II. First Order of Business Section II 1. Adjournment to closed -
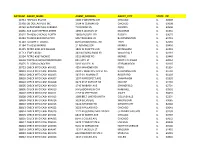
Agtnum Agent Name Agent Address Agent City
AGTNUM AGENT_NAME AGENT_ADDRESS AGENT_CITY STATE ZIP 21931 HISPANO ENVIOS 5000 S WESTERN AVE CHICAGO IL 60609 21938 OB DOLLAR PLUS INC 1704 W CERMAK RD CHICAGO IL 60608 21969 SUPERMERCADO CARRERA 710 FORAN LN AURORA IL 60506 26836 ACE CASH EXPRESS #9309 1690 E JACKSON ST MACOMB IL 61455 31025 TA #030 CHICAGO NORTH 16650 RUSSELL RD RUSSELL IL 60075 31059 TA #092 BLOOMINGTON 505 TRUCKERS LN BLOOMINGTON IL 61701 31140 TA #199 ST LOUIS E 819 EDWARDSVILLE RD TROY IL 62294 31184 TA #236 MORRIS 21 ROMINES DR MORRIS IL 60450 31225 PETRO #321 EFFINGHAM 1805 W FAYETTE AVE EFFINGHAM IL 62401 31713 JEWEL #3341 343 W IRVING PARK RD WOOD DALE IL 60191 32594 PETRO #367 MONEE 5915 MONEE RD MONEE IL 60449 34609 TORTILLERIA/SUPERMERCADO 821 10TH ST NORTH CHICAGO IL 60064 35875 EL GORDO GROCERY 5032 VALLEY LN STREAMWOOD IL 60107 38723 CHECK INTO CASH #04001 4254 MAHONEY DR PERU IL 61354 38801 CHECK INTO CASH #04004 2303 E WASHINGTON ST STE BLOOMINGTON IL 61704 38802 CHECK INTO CASH #04005 3437-39 N MAIN ST ROCKFORD IL 61103 38803 CHECK INTO CASH #04007 1507 N PROSPECT AVE CHAMPAIGN IL 61820 38804 CHECK INTO CASH #04008 3923 41ST AVENUE DR MOLINE IL 61265 38805 CHECK INTO CASH #04009 1740 WABASH AVE SPRINGFIELD IL 62704 38806 CHECK INTO CASH #04010 9 MEADOWVIEW CTR KANKAKEE IL 60901 38807 CHECK INTO CASH #04011 2157 W JEFFERSON JOLIET IL 60435 38808 CHECK INTO CASH #04013 1099 BELT LINE RD UNIT H COLLINSVILLE IL 62234 38809 CHECK INTO CASH #04014 3024 BELVIDERE WAUKEGAN IL 60085 38810 CHECK INTO CASH #04015 3224 NAMEOKI RD GRANITE CITY IL 62040 38813 CHECK -

Officials, C~Ureh Councilmen
.... '! • 0• .. p p 44 • $ • 4 a a s • aatas ssss, sass • All the News of All the Pointes Ijc * * Every Thursday Morning rosse ews COlnplete News Coverage of All the Pointes Home of the News ---;V~O;::\j"LiiU~M~E~2:;-7.~N:-;-O~.-:;2::8------;;E::-;nt-:.-:er~ed;-:-as~se-co-n-:-d-::C::-la-ss-:-:M:-:at-:-te-r-----G-R-O-S-'::-E-P-O-I-N-T-E-, -M-I-C-H-I-G-A-N-,-J-U-L-Y-I-3-,-1-9-b-' --------7c-P-e-r -CO;Y at the Post Office at Detroit, Mlch,... $4,00Per Yt>ar 20 PAGES - THREE SECTIONS - SECTION' Merchants Beautify Shopping District ]Lallge Cites (If ,hI' IWoods Residents, 'VEI~K i Rifts WitlI As Compiled b)' tbe Grosse Pointe NelliS .~ Officials, C~ureh Councilmen Big Difference of Opiniol3 Thursday, July 6 ,;:,' Argue over lienee As to Matters of Policy A NEW ARMY COUP in Al- geria which could lead to im- and Administration Given m<!diate repercussions in France Construction Halted When Public Safety Committee As Reason is now considered a serious posslblHty by observers in bot!' Indicates It Will Not Permit Adjoining Woods City Administra- France and Algeria, Driveway Entrance tor William Lange sub- Top officers in the French I mitted his resignation to A hassle raged Monday night at the Woods council Army in Algeria have been di- the Woodg council on Mon- meeting between James Lemhagen, attorney for Our vided since the deep Army day, July 10, to become purge ordered by Pre sId e n t Lady Star of the Sea Church, residents living near the effective on September 1, Charles de Gaulle after the church, and the Council itself. -

Act Ive Tra Member S
act ive t ra members A&S Supermarkets Fech, Inc. Maroon U dba CC Creations Sears Holdings Management Academy Sports & Outdoors Fiesta Mart, Inc. Mary Kay Inc. Sellers Brothers Advantage Sales & Marketing Flower's Bakeries Melvin's Menswear Silver Eagle Distributors Albertsons (Safeway/Tom Thumb) Food King Music Mountain Water Company Sol Supermarket Alcoholic Beverage License Service Foodworld Neiman Marcus Stage Stores, Inc. Altria Client Services, Inc. El Globo Supermarkets New Canaan Farms, Inc. SuitMart Amber's Designs FTS Solutions, Inc. Amway-Alticor Galveston Battery and Electric Nissin Foods Super Mercado Tamaulipas ANCO Insurance GE Foodland, Inc. Nocona Designs Supermercado del Pueblo Arlan's Market's Hill Country General Mills North Country Business Products Susan Eisen Jewelry Arlan's Markets, Gulf Coast Golden Flake Snack Foods Inc. Northgate Market Target Associated Wholesale Grocers Grocers Supply Co., Inc. Nothing Bundt Cakes/ Doxa Ventures Tax Advisors Group Auto Care Association Grocery Manufacturers Association LLC Texas A&M Center for Retailing AutoZone HAC, Inc Novolex Studies Avalara Hal Martin's Watch & Jewelry Oak Farms Dairy/Dean Foods Texas Aggieland Bookstore Avangard Innovative, LP HEB/ H.E. Butt Grocery Co. Patrick S. Molak Corp. Texas Association of Goodwills Barron's Books Hen House Boutique Payless Supermarket Texas Federation of Drug Stores Baywood Foods, Inc. Hiland Dairy Best Buy Hodge Food Basket Pepsi Bottling Houston Texas Petition Strategies Bimbo Bakeries Home Depot Pepsico/Frito-Lay Texas PWICS Association Blue Bell Creameries, Inc. iGPS Petco Texas Retailers Education Foundation Bodega Latina dba El Super Jim's Supermarket PetSmart Three Brothers Bakery Book People Hops & Grain Brewery Co. -

T. Mary Tral Farrowing Unit Is Utilized
Thifchfrs teifer 473 @ 400 e heifers 353@ bwf hfrs 395 e heifers 39426 e heifers orn hfrs 4088 leifers 365 @ i6; 453@: e heifers 1114 418@ 41, lei fe rs orn hfrs 485 @ 494 15th year no. 1 COWS March 4, 1969 rl cow 1325 e cow 880C441 11 COW 1230@ 141 e cows 1257C cows 181 1145 e cow 1240@ e cow 181. 960 C 3 COW 18p 1340 CIB COWS 97081 COWS 980811; ow 985 0. II cow 1060 cow 11800.11 ows 912 @ 11 cow G&G area farm folk can't 1030 0 wait for the mud to dry 11 out for cow activities to resume. 990 0 P Cattle found themselves belly-high in mud in ows the worst of the mudholes 897 in feedlots, but still cattlemenhad to ow 910 feed them.Cattle were trucked in, 16 and livestock auctionswere ow 975 held as usual. I The show must cow 8608 go on as well for other activities.One of sev- eral G&G area banksto promote ambitious farm tours isthe Union AMISSIO State Bank at Clay Center.Its "livestock roundup"was held de- spite a rainy day anda winter's accumulation of thawed mud. The tour included stops NY at two hog farrowing operations-- one at the Roy Anderson farm, where individual farrowingunits are used, and the other at the Benson Brothersfarm, where acen- t. Mary tral farrowing unit is utilized. These pictures belowwere taken at the Anderson farm. Kan Slogging Weather Farmers and construction workersgot the worst ed the bottomss of feedlotsand construction sites last fSalimweek. -

Are Retailing Mergers Anticompetitive? an Event Study Analysis
Are Retailing Mergers Anticompetitive? An Event Study Analysis Abstract We examine the abnormal returns of rival firms to determine whether four retailing mergers that occurred during the late 1980s reduced competition. We use the stock returns of retailers in geographic markets unaffected by the merger to control for the efficiency-signaling effect of the merger. Using this methodology, we find that rival firms experienced positive abnormal returns from May Company’s 1986 acquisition of Associated Dry Goods and American Stores’ 1988 acquisition of Lucky Stores. These results offer some evidence that retailing mergers that lead to large increases in concentration in already concentrated markets may lessen competition and lead to higher product market prices. John David Simpson Federal Trade Commission and Daniel Hosken Federal Trade Commission January 1998 I) Introduction Antitrust enforcement of retailing mergers has varied over time. In the 1960s, the antitrust agencies and the courts pursued a very aggressive antitrust policy. For example, the Supreme Court blocked a 1960 merger between Von’s Grocery and Shopping Bag Food Stores that would have given the merged firm a 7.5 percent share of the grocery retailing business in Los Angeles.1 In contrast, the antitrust agencies followed a much more relaxed antitrust policy in the 1980s. For instance, the Federal Trade Commission did not challenge May Department Stores Company’s 1986 acquisition of Associated Dry Goods which would have given the combined firm control of nearly all of the traditional department stores in the Pittsburgh area.2 More recently, the antitrust agencies and the courts have adopted a more moderate position with respect to retailing mergers.