Southwark and Lambeth Integrated Care Evaluation of the Older People’S Programme
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Appointment Brief Chief Operating Officer August 2020
Appointment brief Chief Operating Officer August 2020 Introduction South London and Maudsley NHS Foundation Trust (SLaM) is an exceptional organisation. Everything we do as a Trust is to support people to recover from mental illness and to help them improve their lives. Benefitting from world-class research and innovation, award-winning services and a world-renowned brand, we are uniquely placed to provide the best possible services to our local communities and beyond. Our biggest asset is our passionate and highly skilled workforce, who are dedicated to providing the best quality care to the people who use our services, often in difficult circumstances. We have managed the many challenges that COVID-19 has presented with great success and this has only been possible through the hard work and commitment of our staff. We are pleased with our internal patient experience survey results, where 96% of respondents said they found staff kind and caring and 87% of respondents to the NHS Friends and Families Test said that they would recommend the Trust to their friends and families based on their experience of the services provided. Operating across more than 90 sites, including Bethlem Royal Hospital and Maudsley Hospital, we provide a staggering range of services, ranging from core mental health services to our local boroughs, and more than 50 specialist mental health services across the UK. We are rated ‘Good’ overall by the Care Quality Commission, including for the ‘Well Led’ domain. With our strong commitment to working in partnership with our service users, carers and local communities, and to quality improvement, we believe we are capable of delivering truly outstanding services across all our teams We know that we will only achieve this if SLaM truly is a great place to work, where all our staff feel valued, developed and supported. -

Records of Patients in London Hospitals
RESEARCH GUIDE 35 - Records of Patients in London Hospitals CONTENTS Introduction Hospital Archives Guides to Hospital Records Lying In Hospitals Access to Patients Records Other sources of information about hospital patients Registers of patients in psychiatric hospitals Introduction Many of the monastic hospitals which had cared for the sick poor of medieval London were suppressed on the dissolution of the monasteries in the 1530s and 1540s. St. Bartholomew's Hospital, St. Thomas' Hospital, and Bethlem Royal Hospital were saved by the City of London Corporation, which obtained grants of the hospitals and their endowments from King Henry VIII and from his son, Edward VI. The hospitals were refounded as secular institutions, St. Bartholomew's and St. Thomas' caring for the physically sick and Bethlem for the insane. Over time they established their virtual independence from the City of London. Thomas Guy, a London publisher and bookseller, left the fortune which he made out of the South Sea Bubble, to found Guy's Hospital which opened in 1725. Other major London hospitals, including the Westminster, Royal London, Middlesex, and St. George's Hospitals, were established in the 18th century on the voluntary principle. Medical men gave their services free while wealthy subscribers gave money each year to support the hospitals, in return for which they gained a share in the government of the hospital and the right to nominate patients. Medical schools developed in association with the hospitals. Many categories of the sick, including pregnant women, the mentally ill, and patients suffering from incurable or infectious diseases were excluded from most hospitals. -

Patient Transfers & Conveyanc E
London METROPOLITAN Working together for a safer London South POLICE and Maudsley t TERRITORIAL POLICING NHS Foundation Trus Joint Protocols Working in Partnership with Mental Health Issue s South London & Maudsley NHS Foundation Trus t & Metropolitan Police ; Lambeth, Southwark, Lewisham, Croydon & Bromley The protocols describe the roles and responsibilities of each agency when dealing with the following incidents 1 . Disturbances on hospital wards and other mental health facilitie s 2. Gu idance re: restraini ng patients by Po lice and med icating patients by nursing staff 3. Offences committed by people suffering from mental illnes s 4. Guidance re: custody procedures and case disposal options 5 . Absence without Leave (The reporting of patients who are found to be missing from the wa rd or who do not return at the agreed time) 6 . The retu rning of patients reported as missin g 7. Detain ing people requiri ng i mmediate ca re and control in a pub lic p l ace (s136 Menta l Health Act 1983) 8. Mental health assessments within the communit y 9 . Patient transfers & conveyanc e Effective Date : September 2012 Review Date : February 2013 1 Stuart Bell - Borough Commander Signature . Lewisham Metropo litan Police Borough Commande r Signature . .. So u thwark Metropolitan Police David Musker - Borough Commander Signature . .. Croydon Metropolitan Police Stephanie Roberts - Borough Commander Signature . .. Bromley Metropol itan Police Matthew Bell - Borough Commander Signature . Lam be th Metropolitan Po lice Gus Heafield - Acting Chief Executive Signature . So u th London and Ma u dsley N HS Fo u ndatio n London Ambulance Service Signature 2 Introduction to Joint Police Protocols The police are often the first point of contact for a person in a mental health crisis . -

An Independent Investigation Into the Care and Treatment of Mr R
An Independent Investigation into the Care and Treatment of Mr R February 2012 A report for Undertaken by Niche Health & Social Care Consulting Contents 1.0 INTRODUCTION......................................................................................................................1 2.0 PURPOSE AND SCOPE OF INVESTIGATION ..............................................................................1 3.0 SUMMARY OF THE INCIDENT .................................................................................................1 4.0 CONDOLENCES TO THE FAMILY OF MR Q ...............................................................................3 5.0 ACKNOWLEDGEMENT OF PARTICIPANTS................................................................................3 6.0 TERMS OF REFERENCE............................................................................................................3 7.0 THE INDEPENDENT INVESTIGATION TEAM .............................................................................6 8.0 INVESTIGATION METHODOLOGY............................................................................................6 9.0 SOURCES OF INFORMATION...................................................................................................9 10. CHRONOLOGY......................................................................................................................10 11.0 REVIEW OF THE MENTAL HEALTH CARE AND TREATMENT PROVIDED BY THE TRUST TO MR R FROM HIS FIRST CONTACT TO THE TIME OF THE OFFENCE AND THE SUITABILITY OF -

A & C Black Ltd, 35 Bedford Row, London WC IR 4JH (01-242-0946
365 A A & C Black Ltd, 35 Bedford Row, London WC IR 4JH (01-242-0946) Academy of Sciences, Frescati, s-10405 Stockholm 50, Sweden Accepting Houses Committee, I Crutched Friars, London EC3 (0 1-481-2120) Access, 7 StMartin's Place, London WC2 (01-839-7090) Acupuncture Association and Register Ltd, 34 Alderney St, London SWIV 4EU (01-834-1012) Advertising Standards Authority, 15-17 Bridgemount St, London WCIE 7AW (01-580--0801) Advisory, Conciliation and Arbitration Service, Head Office, Cleland House, Page St, London SW 1P 4ND (01-222-4383) Advisory, Conciliation and Arbitration Service Regional Offices --Midlands, Alpha Tower, Suffolk St Queensway, Birmingham Bl ITZ (021-643-9911) --North West, Boulton House, 17-21 Charlton St, Manchester Ml 3HY (061-228-3222) --Northern, Westgate House, Westgate Rd, Newcastle-upon-Tyne NEI ITJ (0632-612191) --Scotland, 109 Waterloo St, Glasgow, G2 ?BY (041-221-6832) --South East, Hanway House, Red Lion Sq, London WCIR 4NH (01-405-8454) --South West, 16 Park Place, Clifton, Bristol BS8 IJP (0272-211921) --Wales, 2-4 Park Grove, CardiffCFl 3QY (0222-45231) --Yorkshire and Humberside, City House, Leeds LSI 4JH (0532-38232) Advisory Council on Public Records, Public Record Office, Chancery Lane, London WC2A ILR (01-405-0741) Advisory Welsh Translations Panel, Oxford House, Cardiff(0222-44171) Afghanistan, Embassy of the Republic of, 31 Prince's Gate, London SW7 1QQ (0 1-589-8891) African Violet Society of America, 4988 Schollmeyer Ave, StLouis, Mo 63109, USA Agricultural Credit Corporation Ltd, Agricultural -
Everything We Do Is to Improve the Lives of the People and Communities We Serve and to Promote Mental Health and Wellbeing for All
Clinical services Everything we do is to improve the lives of the people and communities we serve and to promote mental health and wellbeing for all No. Borough Clinical Academic Group No. Borough Clinical Academic Group No. Borough Clinical Academic Group Bexley Lambeth Southwark 1 Drug and Alcohol Service (Bexley) - 01322 357 940 Addictions 29 Psychosis Promoting Recovery (Lambeth South) - 020 3228 8100 Psychosis 55 Drug and Alcohol Service (Southwark) - 020 3228 9400 Addictions Drug Intervention Programme (Bexley) - 01322 357 940 South Asian Community Mental Health Service (Lambeth) - 020 3228 8100 151 Blackfriars Road, London SE1 8EL Erith Health Centre, 50 Pier Road, Erith DA8 1AT 380 Streatham High Road, London SW16 6HP Southwark Erith Streatham 56 Smoking Service - 020 3228 3848 30 Placements Assessments Monitoring Services - 020 3228 7000 Marina House, 63-65 Denmark Hill, London SE5 8RS Bromley Social Inclusion, Hope and Recovery Project (Lambeth) - 020 3228 7050 Denmark Hill 308 - 312 Brixton Road, London SW9 6AA 2 Bethlem Royal Hospital 57 Forensic Community Service (Southwark) - 020 3228 7168 Behavioural and Monks Orchard Road, Beckenham BR3 3BX Brixton Chaucer Resource Centre, 13 Ann Moss Way, London SE16 2TH Developmental Psychiatry 31 Psychosis Promoting Recovery (Lambeth Central) - 020 3228 6940 Eden Park West Wickham Bromley South then bus 119 East Croydon then bus 119, 194 or 198. Canada Water Surrey Quays Psychosis Promoting Recovery (Lambeth North East) - 020 3228 6940 A bus service runs between Bethlem and Maudsley -

Postgraduate Guide
2017 POSTGRADUATE GUIDE 5 260+ CAMPUSES IN THE SOCIETIES AND 84% HEART OF LONDON STUDENT GROUPS OF RESEARCH IS WORLD-LEADING 6th OR EXCELLENT 250+ 10.5k IN THE UK £1bn Research Excellence COURSES WITH 12 Framework (REF) 2014 NOBEL PRIZE REDEVELOPMENT POSTGRADUATE QS World University PART-TIME OPTIONS Rankings 2016–17 WINNERS PROGRAMME STUDENTS 91% ONE OF THE WORLD’S 4th MASTER’S GRADUATES IN WORK OR FURTHER STUDY OLDEST UNIVERSITY IN ENGLAND Destinations of Leavers from Higher Education (DLHE) 2015 Top 25 300+ UNIVERSITIES PARTNERSHIPS QS World University WORLDWIDE Top 7 LONDONLONDON IS ISTHE THE Rankings 2016–17 IN THE UK FOR RESEARCH EARNINGS 5th REF 2014 BEST STUDENT CITY IN THE WORLD £28k 60 QS Best Student Cities AVERAGE SALARY OF OUR MASTER’S GRADUATES SPORTS 2016 CLUBS 1.2m DLHE 2015 BOOKS AND E-BOOKS IN KING’S LIBRARIES 7th IN THE UK FOR 26,700+ 5th GRADUATE EMPLOYABILITY STUDENTS FROM MORE Times Higher Education 2015 IN THE UK FOR THE QUALITY THAN 150 COUNTRIES OF OUR RESEARCH REF 2014 Contents Why King’s 2 Subject areas – Find your niche 58 London locations 2 Academic Preparation Courses 60 Be part of London 4 Arts, Culture & Media 62 Join a vibrant community 6 Biomedical & Chemical Sciences 66 Academic excellence 8 Computer Science & Engineering 70 Enhance your career 10 Dental Training & Science 74 Connect to arts & sciences 12 Education & Child Studies 78 Connect to health 14 Geography, the Environment 82 & Development Connect to the world 16 Global Health & Social Medicine 86 Build skills & networks 18 Healthcare Management -

South Thames Foundation School Prospectus
South Thames Foundation School Prospectus Programmes Commencing August 2018 South Thames Foundation School Introduction 1 Welcome 1 What is a foundation school? 3 The UK Foundation Programme Office (UKFPO) 3 Structure of foundation training 4 Overview of STFS 5 Applying for foundation training 5 Allocation to programmes within STFS 5 Purpose of the Foundation Programme 7 The foundation programme aims to: 7 Outcomes of foundation training 7 Broadening the Foundation Programme (BTFP) 8 Community Placements 8 Dr Toolbox 8 Safe prescribing 9 Doctors with disabilities 9 Map showing location of trusts affiliated to STFS 11 List of trusts affiliated to STFS 12 Glossary of trust staff 13 Educational supervisor 13 Clinical supervisor 13 Medical education manager (MEM) 13 Curriculum 13 Reference guide 14 e-Portfolio 14 Foundation key documents 14 Information about your training 15 Employment information 15 Time limit on provisional registration 15 Deferring the start of foundation training 15 Extended induction 16 General practice (GP) location and travel allowances 16 Shadowing 16 Transfer of information 16 Travel and relocation expenses 16 Tasters 17 Purpose of SLEs 17 SLE methodology 17 Careers 17 Supervised learning events (SLEs) 17 Educational and development tools 18 Assessment 18 Assessment 19 Self-assessment 19 Feedback and debriefing 19 Annual review of competence progression (ARCP) 19 Prospectus commencing August 2018 www.stfs.org.uk London and South East PGMDE Support Portal lasepgmdesupport.hee.nhs.uk/support/home Special circumstances -

2Nd Despatch
Page 1 Agenda Item 4 JHOSC JHOSC 4: SessionFeedbackandRecommendations Consultation Health Services for Lambeth Services for Health Improving Inpatient Mental Mental Inpatient Improving Page 2 Purpose 2 What we are going to cover 1) Scope of the Consultation A brief refresher of the scope of the public consultation 2) Feedback Report and Key Metrics Key metrics arising from the independent analysis of the consultation feedback 3) Key Feedback Themes and Recommendations Page 3 The main themes that were raised within the consultation, our assessment of those areas and recommendations where appropriate 4) The Decision Making Process An overview of the decision making process and recommendations for the Lambeth Together Strategic Board 5) Further Considerations Arising from the Consultation Key issues raised that are outside of the direct scope of the public consultation but of importance to the be followed through Section 1: Page 4 Consultation Scope 4 Scope of the Consultation • The public consultation The public consultation which ran from March 4th 2020 to May 31st looked at the future of adult acute inpatient wards and a psychiatric intensive care unit currently located at the Lambeth Hospital and proposed two options. • Option 1: Remain as we are (do nothing) • Option 2: [Preferred] Relocate four acute wards and the Psychiatric Intensive Care Unit (PICU) to the Maudsley site • Other engagement not within the scope of the public consultation To ensure that Members had a clear view of the broader programme of changes outside the scope -
Points Asked How Many Times Today
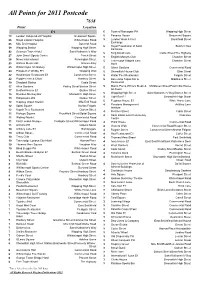
All Points for 2011 Postcode 7638 Point Location E1 6 Town of Ramsgate PH Wapping High Street 73 London Independent Hospital Beaumont Square 5 Panama House Beaumont Square 66 Royal London Hospital Whitechapel Road 5 London Wool & Fruit Brushfield Street Exchange 65 Mile End Hospital Bancroft Road 5 Royal Foundation of Saint Butcher Row 59 Wapping Station Wapping High Street Katharine 42 Guoman Tower Hotel Saint Katharine’s Way 5 King David Lane Cable Street/The Highway John Orwell Sports Centre Tench Street 27 5 English Martyrs Club Chamber Street News International Pennington Street 26 5 Travelodge Aldgate East Chamber Street 25 Wiltons Music Hall Graces Alley Hotel 25 Whitechapel Art Gallery Whitechapel High Street 5 Albert Gardens Commercial Road 24 Prospect of Whitby PH Wapping Wall 5 Shoreditch House Club Ebor Street 22 Hawksmoor Restaurant E1 Commercial Street 5 Water Poet Restaurant Folgate Street 22 Poppies Fish & Chips Hanbury Street 5 Barcelona Tapas Bar & Middlesex Street 19 Shadwell Station Cable Street Restaurant 17 Allen Gardens Pedley Street/Buxton Street 5 Marco Pierre White's Steak & Middlesex Street/East India House 17 Bedford House E1 Quaker Street Alehouse Wapping High Street Saint Katharine’s Way/Garnet Street 15 Drunken Monkey Bar Shoreditch High Street 5 Light Bar E1 Shoreditch High Street 13 Hollywood Lofts Quaker Street 5 Pegasus House E1 White Horse Lane 12 Stepney Green Station Mile End Road 5 Pensions Management Artillery Lane 12 Spital Square Norton Folgate 4 Institute 12 Kapok Tree Restaurant Osborn Street -
Improving Acute Inpatient Facilities in Lambeth for People with Mental
Improving acute inpatient facilities in Lambeth for people with mental health needs Pre consultation research around proposals for move and new build of inpatient facilities Feedback on Location and Design Mike Rogers Feb 2020 Healthwatch Lambeth Contents Introduction 1 Methodology 2 Findings, What people told us - Summary of key findings 4 - Location - Outside gardens and fresh air - Design and appearance 8 - Visitors, carers & families 14 - New facilities for staff 14 - Other issues 15 Appendix Simplified lay out of proposed Douglas Bennett House development used to support discussions. Healthwatch Lambeth 1. Introduction Healthwatch Lambeth undertook independent pre-consultation research to support South London and Maudsley Mental Health Trust around improving acute in patient services for Lambeth residents. The purpose of the work was to support the Trust in the design and delivery of effective formal consultation around proposals to move acute inpatient facilities to a new purpose block on the site of Douglas Bennet House within the grounds of the Maudsley Hospital at Denmark Hill, closing all services on the Lambeth Hospital site in Landor Road. We appreciate the importance of understanding and communicating the context for the proposed changes. We emphasised the following key points to participants in the research: • The Trust acknowledge feedback from patient, carers, staff and CQC and others about improvements needed to acute in patient services. • The Trust has a commitment to make improvements for everyone (from all boroughs) this plan will include some refurbishment of existing wards and building some new wards • There will be no reduction in the number of beds. • All new wards will meet the strict national standards designed to ensure patient safety and positive experience. -
Improving Inpatient Mental Health Services for Lambeth Joint HOSC Meeting Briefing Pack Section 1 Recap of the Previous JHOSC Session on 27Th March 2020
Improving Inpatient Mental Health Services for Lambeth Joint HOSC Meeting Briefing Pack Section 1 Recap of the previous JHOSC session on 27th March 2020 2 What we want to achieve 1. We must improve the quality and safety of our inpatient 2. We are committed to supporting people in Lambeth who wards to meet the most basic needs of our patients are experiencing mental illness or distress To improve patient care and experience 3. There is an opportunity to build a new purpose built mental 4. Together with our partners, as a health economy, we are health unit planning for the future and recognise the need to consider all patients, across all our boroughs 3 The current vs proposed ward 4 The preferred option The public consultation will specifically seek views on options for the Lambeth Hospital site wards with other services being managed through concurrent separate engagement processes. The options are: • Option 1: Remain as we are (do nothing) • Option 2: [Preferred] Relocate four acute wards and the Psychiatric Intensive Care Unit (PICU) to the Maudsley site • Rosa Parkes (acute admission ward) • Leo (early intervention inpatient ward) • Nelson (acute admission ward) • Eden (PICU) – into new DBH • Luther King (acute admission ward) An option to develop a new high-quality facility on the Lambeth Hospital site was also looked at. However, this failed to meet for two key tests: • Was the option realistic? This option requires additional capital of between £30m and £35m due to additional infrastructure and loss of capital receipts which is coupled with a need to decant at least one ward to Bethlem and another to Maudsley causing significant disruption making the option unrealistic.