IMPF Newsletter, Budget Session 2017 Issue
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download 383.61KB
For private circulation only Newsletter Vol. 5, No. 3 Winter Session Issue Nov-Dec 2015 Dear Friends, At a glance: On behalf of the IMPF, it is our pleasure to present the Winter lProf. Ranjit Roy Chaudhury: Session 2015 edition of the IMPF Newsletter. The Monsoon A Tribute Session Issue focused on crucial health issues plaguing India lOsteoporosis – 'The Silent Disease’ such as substance abuse, multi drug resistant (MDR) TB, public lClinical Trials: Secret Regime? health facilities, the importance of family planning, etc. The lSurrogacy in India issue was widely circulated, prompting discussions and lHealth for All – Learning from the deliberations into looking for sustainable solutions to the above World mentioned problems. lNIKSHAY lAnti-Microbial Resistance We dedicate this issue to Prof. Ranjit Roy Chaudhury, who lDiabetes recently passed away. Prof. Chaudhury was a renowned public health advocate and educationist, who contributed to the field of modern medical education, pharmacological science, research ethics, health policy, etc. In this issue, we are highlighting some of the health challenges of osteoporosis, surrogacy, issues related to clinical trials, etc. The issue is also emphasizing the need of addressing the concerns that civil society and parliamentarians must collaboratively work and delve on to improve the health planning, policy and implementation. IMPF is committed to bringing the issues to the notice of the policy makers and leaders and thereby to improve the health sector. We express our sincere thanks to all the contributors who have made this newsletter significant and informative for parliamentarians across political parties. We appreciate the comments and suggestions received from our supporters, and look forward to working with you to carry forward our responsibilities. -

List of Successful Candidates
11 - LIST OF SUCCESSFUL CANDIDATES CONSTITUENCY WINNER PARTY Andhra Pradesh 1 Nagarkurnool Dr. Manda Jagannath INC 2 Nalgonda Gutha Sukender Reddy INC 3 Bhongir Komatireddy Raj Gopal Reddy INC 4 Warangal Rajaiah Siricilla INC 5 Mahabubabad P. Balram INC 6 Khammam Nama Nageswara Rao TDP 7 Aruku Kishore Chandra Suryanarayana INC Deo Vyricherla 8 Srikakulam Killi Krupa Rani INC 9 Vizianagaram Jhansi Lakshmi Botcha INC 10 Visakhapatnam Daggubati Purandeswari INC 11 Anakapalli Sabbam Hari INC 12 Kakinada M.M.Pallamraju INC 13 Amalapuram G.V.Harsha Kumar INC 14 Rajahmundry Aruna Kumar Vundavalli INC 15 Narsapuram Bapiraju Kanumuru INC 16 Eluru Kavuri Sambasiva Rao INC 17 Machilipatnam Konakalla Narayana Rao TDP 18 Vijayawada Lagadapati Raja Gopal INC 19 Guntur Rayapati Sambasiva Rao INC 20 Narasaraopet Modugula Venugopala Reddy TDP 21 Bapatla Panabaka Lakshmi INC 22 Ongole Magunta Srinivasulu Reddy INC 23 Nandyal S.P.Y.Reddy INC 24 Kurnool Kotla Jaya Surya Prakash Reddy INC 25 Anantapur Anantha Venkata Rami Reddy INC 26 Hindupur Kristappa Nimmala TDP 27 Kadapa Y.S. Jagan Mohan Reddy INC 28 Nellore Mekapati Rajamohan Reddy INC 29 Tirupati Chinta Mohan INC 30 Rajampet Annayyagari Sai Prathap INC 31 Chittoor Naramalli Sivaprasad TDP 32 Adilabad Rathod Ramesh TDP 33 Peddapalle Dr.G.Vivekanand INC 34 Karimnagar Ponnam Prabhakar INC 35 Nizamabad Madhu Yaskhi Goud INC 36 Zahirabad Suresh Kumar Shetkar INC 37 Medak Vijaya Shanthi .M TRS 38 Malkajgiri Sarvey Sathyanarayana INC 39 Secundrabad Anjan Kumar Yadav M INC 40 Hyderabad Asaduddin Owaisi AIMIM 41 Chelvella Jaipal Reddy Sudini INC 1 GENERAL ELECTIONS,INDIA 2009 LIST OF SUCCESSFUL CANDIDATE CONSTITUENCY WINNER PARTY Andhra Pradesh 42 Mahbubnagar K. -

Oram, Shri Jual
For official use only LOK SABHA DEBATES ON THE CONSTITUTION (ONE HUNDRED AND TWENTY FIRST AMENDMENT) BILL, 2014 (Insertion of new articles 124A, 124B and 124C) AND THE NATIONAL JUDICIAL APPOINTMENTS COMMISSION BILL, 2014 (Seal) LOK SABHA SECRETARIAT NEW DELHI EDITORIAL BOARD P.K. Grover Secretary General Lok Sabha R.K. Jain Joint Secretary Vandna Trivedi Director Parmjeet Karolia Additional Director J.B.S. Rawat Joint Director Pratibha Kashyap Assistant Editor © 2014 Lok Sabha Secretariat None of the material may be copied, reproduced, distributed, republished, downloaded, displayed, posted or transmitted in any form or by any means, including but not limited to, electronic, mechanical, photocopying, recording, or otherwise, without the prior permission of Lok Sabha Secretariat. However, the material can be displayed, copied, distributed and downloaded for personal, non-commercial use only, provided the material is not modified and all copyright and other proprietary notices contained in the material are retained. CONTENTS Tuesday/Wednesday, August 12/13, 2014/Shravana 21/22, 1936 (Saka) Pages THE CONSTITUTION (ONE HUNDRED AND TWENTY- 1-105 FIRST AMENDMENT) BILL, 2014 (Insertion of new articles 124A, 124B and 124C) AND THE NATIONAL JUDICIAL APPOINTMENTS COMMISSION BILL, 2014 Motion to consider 1-2 Shri Ravi Shankar Prasad 2-13, 77-99 Shri M. Veerappa Moily 16-26 Shri S.S. Ahluwalia 26-31 Dr. M. Thambidurai 31-38 Shri Kalyan Banerjee 39-46 Shri Bhartruhari Mahtab 46-52 Shri Anandrao Adsul 52-53 Shri B. Vinod Kumar 53-55 Dr. A. Sampath 55-59 Shri Ram Vilas Paswan 60-63 Shri Dharmendra Yadav 63-64 Shri Rajesh Ranjan 65-66 Dr. -

Standing Committee Report
REPORT NO. 85 PARLIAMENT OF INDIA RAJYA SABHA DEPARTMENT-RELATED PARLIAMENTARY STANDING COMMITTEE ON HEALTH AND FAMILY WELFARE EIGHTY-FIFTH REPORT On THE HUMAN IMMUNODEFICIENCY VIRUS AND ACQUIRED IMMUNE DEFICIENCY SYNDROME (PREVENTION AND CONTROL) BILL, 2014 (Ministry of Health and Family Welfare) (Presented to the Rajya Sabha on 29 th April, 2015) (Laid on the Table of Lok Sabha on 29 th April , 2015 ) Rajya Sabha Secretariat, New Delhi April, 2015/ Vaisakha, 1937 (SAKA) PARLIAMENT OF INDIA RAJYA SABHA DEPARTMENT-RELATED PARLIAMENTARY STANDING COMMITTEE ON HEALTH AND FAMILY WELFARE EIGHTY-FIFTH REPORT On THE HUMAN IMMUNODEFICIENCY VIRUS AND ACQUIRED IMMUNE DEFICIENCY SYNDROME (PREVENTION AND CONTROL) BILL, 2014 (Ministry of Health and Family Welfare) (Presented to the Rajya Sabha on 29 th April, 2015) (Laid on the Table of Lok Sabha on 29 th April , 2015 ) Rajya Sabha Secretariat, New Delhi April, 2015/ Vaisakha, 1937 (SAKA) CONTENTS PAGES 1. C OMPOSITION OF THE COMMITTEE ......................................................................................... (i)-(ii) 2. P REFACE ............................................................................................................................... (iii) *3. L IST OF ACRONYMS ................................................................................................................ (iv) 4. R EPORT ................................................................................................................................... 1 *5. O BSERVATIONS /R ECOMMENDATIONS — AT A -

Need to Provide Budgetary Support to the Government of West Bengal for Setting up Madarsas
an> Title: Need to provide budgetary support to the Government of West Bengal for setting up Madarsas. SHRI SUDIP BANDYOPADHYAY (KOLKATA UTTAR): In our State, West Bengal, minorities contribute 2.57 crore, that is 28.1 per cent of the total population. The present Government has increased the budgetary support for development of minorities by five times, from Rs.472 crore in 2010-11 to Rs.2,383 core during the current fiscal year. We met the hon. Minister, Shrimati Najma Heptulla with a delegation just two days back at her residence in the morning and discussed in detail. We have some issues. Firstly, scholarships are offered by the Central Government under the 15 point programme. In West Bengal, it was 20 lakhs, this year we have received applications of near about 30 lakhs. We would like to appeal to the Central Government to consider increase the quota from 20 lakhs to 30 lakhs. Secondly, Multi Sectoral Development Programme during 2015-16, the Government made an appeal for a grant of Rs.415 crore, and only Rs.100 crore has been allotted. The balance may kindly be delivered at the quickest possible time. About the clusters of minority areas outside NCBs, proposals for approval of minorities clusters under the MSDP are pending, approval may be given to the name. About Cyber Gram, the State has proposed to the Minister this. This Government has sanctioned 243 Madrasas, out of 615 Government-aided Madrasas. Balance may be released as per the proposal. The State Government has undertaken the project of Skill Development Programme with a project cost of Rs.86.46 crore under MSDP; Rs.6.02 crore has been sanctioned towards administrative cost for this purpose. -
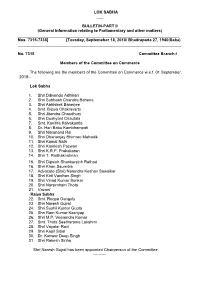
LOK SABHA ___ BULLETIN-PART II (General Information Relating To
LOK SABHA ___ BULLETIN-PART II (General Information relating to Parliamentary and other matters) ________________________________________________________________________ Nos. 7315-7338] [Tuesday, Septemeber 18, 2018/ Bhadrapada 27, 1940(Saka) _________________________________________________________________________ No. 7315 Committee Branch-I Members of the Committee on Commerce The following are the members of the Committee on Commerce w.e.f. 01 September, 2018:- Lok Sabha 1. Shri Dibyendu Adhikari 2. Shri Subhash Chandra Baheria 3. Shri Abhishek Banerjee 4. Smt. Bijoya Chakravarty 5. Shri Jitendra Chaudhury 6. Shri Dushyant Chautala 7. Smt. Kavitha Kalvakuntla 8. Dr. Hari Babu Kambhampati 9. Shri Nityanand Rai 10. Shri Dhananjay Bhimrao Mahadik 11. Shri Kamal Nath 12. Shri Kamlesh Paswan 13. Shri K.R.P. Prabakaran 14. Shri T. Radhakrishnan 15. Shri Dipsinh Shankarsinh Rathod 16. Shri Khan Saumitra 17. Advocate (Shri) Narendra Keshav Sawaikar 18. Shri Kirti Vardhan Singh 19. Shri Vinod Kumar Sonkar 20. Shri Narsimham Thota 21. Vacant Rajya Sabha 22. Smt. Roopa Ganguly 23. Shri Naresh Gujral 24. Shri Sushil Kumar Gupta 25. Shri Ram Kumar Kashyap 26. Shri M.P. Veerendra Kumar 27. Smt. Thota Seetharama Lakshmi 28. Shri Vayalar Ravi 29. Shri Kapil Sibal 30. Dr. Kanwar Deep Singh 31. Shri Rakesh Sinha Shri Naresh Gujral has been appointed Chairperson of the Committee. ---------- No.7316 Committee Branch-I Members of the Committee on Home Affairs The following are the members of the Committee on Home Affairs w.e.f. 01 September, 2018:- Lok Sabha 1. Dr. Sanjeev Kumar Balyan 2. Shri Prem Singh Chandumajra 3. Shri Adhir Ranjan Chowdhury 4. Dr. (Smt.) Kakoli Ghosh Dastidar 5. Shri Ramen Deka 6. -

List of Winning Candidated Final for 16Th
Leading/Winning State PC No PC Name Candidate Leading/Winning Party Andhra Pradesh 1 Adilabad Rathod Ramesh Telugu Desam Andhra Pradesh 2 Peddapalle Dr.G.Vivekanand Indian National Congress Andhra Pradesh 3 Karimnagar Ponnam Prabhakar Indian National Congress Andhra Pradesh 4 Nizamabad Madhu Yaskhi Goud Indian National Congress Andhra Pradesh 5 Zahirabad Suresh Kumar Shetkar Indian National Congress Andhra Pradesh 6 Medak Vijaya Shanthi .M Telangana Rashtra Samithi Andhra Pradesh 7 Malkajgiri Sarvey Sathyanarayana Indian National Congress Andhra Pradesh 8 Secundrabad Anjan Kumar Yadav M Indian National Congress Andhra Pradesh 9 Hyderabad Asaduddin Owaisi All India Majlis-E-Ittehadul Muslimeen Andhra Pradesh 10 Chelvella Jaipal Reddy Sudini Indian National Congress Andhra Pradesh 11 Mahbubnagar K. Chandrasekhar Rao Telangana Rashtra Samithi Andhra Pradesh 12 Nagarkurnool Dr. Manda Jagannath Indian National Congress Andhra Pradesh 13 Nalgonda Gutha Sukender Reddy Indian National Congress Andhra Pradesh 14 Bhongir Komatireddy Raj Gopal Reddy Indian National Congress Andhra Pradesh 15 Warangal Rajaiah Siricilla Indian National Congress Andhra Pradesh 16 Mahabubabad P. Balram Indian National Congress Andhra Pradesh 17 Khammam Nama Nageswara Rao Telugu Desam Kishore Chandra Suryanarayana Andhra Pradesh 18 Aruku Deo Vyricherla Indian National Congress Andhra Pradesh 19 Srikakulam Killi Krupa Rani Indian National Congress Andhra Pradesh 20 Vizianagaram Jhansi Lakshmi Botcha Indian National Congress Andhra Pradesh 21 Visakhapatnam Daggubati Purandeswari -

Parliamentary Bulletin
RAJYA SABHA Parliamentary Bulletin PART-II Nos.: 51236-51237] WEDNESDAY, SEPTEMBER 4, 2013 No. 51236 Committee Co-ordination Section Meeting of the Parliamentary Forum on Youth As intimated by the Lok Sabha Secretariat, a meeting of the Parliamentary Forum on Youth on the subject ‘Youth and Social Media: Challenges and Opportunities’ will be held on Thursday, 05 September, 2013 at 1530 hrs. in Committee Room No.074, Ground Floor, Parliament Library Building, New Delhi. Shri Naman Pugalia, Public Affairs Analyst, Google India will make a presentation. 2. Members are requested to kindly make it convenient to attend the meeting. ——— No. 51237 Committee Co-ordination Section Re-constitution of the Department-related Parliamentary Standing Committees (2013-2014) The Department–related Parliamentary Standing Committees have been reconstituted w.e.f. 31st August, 2013 as follows: - Committee on Commerce RAJYA SABHA 1. Shri Birendra Prasad Baishya 2. Shri K.N. Balagopal 3. Shri P. Bhattacharya 4. Shri Shadi Lal Batra 2 5. Shri Vijay Jawaharlal Darda 6. Shri Prem Chand Gupta 7. Shri Ishwarlal Shankarlal Jain 8. Shri Shanta Kumar 9. Dr. Vijay Mallya 10. Shri Rangasayee Ramakrishna LOK SABHA 11. Shri J.P. Agarwal 12. Shri G.S. Basavaraj 13. Shri Kuldeep Bishnoi 14. Shri C.M. Chang 15. Shri Jayant Chaudhary 16. Shri K.P. Dhanapalan 17. Shri Shivaram Gouda 18. Shri Sk. Saidul Haque 19. Shri S. R. Jeyadurai 20. Shri Nalin Kumar Kateel 21. Shrimati Putul Kumari 22. Shri P. Lingam 23. Shri Baijayant ‘Jay’ Panda 24. Shri Kadir Rana 25. Shri Nama Nageswara Rao 26. Shri Vishnu Dev Sai 27. -

Wit and Humour, Poetry and Couplet Ninth Session (2016) of Sixteenth Lok Sabha (18.7.2016-12.8.2016)
WIT AND HUMOUR, POETRY AND COUPLET NINTH SESSION (2016) OF SIXTEENTH LOK SABHA (18.7.2016-12.8.2016) Sr. Date Subject Name of Poetry/ N Member/Minist Humour/ o. er Couplet/ Repartee 1. 20.7.2016 Discussion under Rule 193 on Shri Poem the situation arising out of Jyotiraditya M. recent violence in Kashmir Scindia Valley 2. 20.7.2016 Discussion under Rule 193 on Shri Bhagwant Couplet the situation arising out of Mann recent violence in Kashmir Valley 3. 20.7.2016 Discussion under Rule 193 on Shri Badruddin Couplet the situation arising out of Ajmal recent violence in Kashmir Valley 4. 21.7.2016 Discussion under Rule 193 on Shri Rajnath Couplet the situation arising out of Singh recent violence in Kashmir Valley 5. 26.7.2016 Discussion on Child Labour Shrimati Poem (Prohibition & Regulation) Aparupa Amendment Bill Poddar 6. 26.7.2016 Discussion on Child Labour Shri Badruddin Poems (Prohibition & Regulation) Ajmal Amendment Bill 7. 26.7.2016 Discussion on Child Labour Dr. Ratna De Politics is not (Prohibition & Regulation) Nag merely about Amendment Bill next election but a moral obligation to the next generation 8. 26.7.2016 Discussion on Child Labour Shri Rajesh Poem (Prohibition & Regulation) Ranjan Amendment Bill 9. 28.7.2016 Discussion under Rule 193 on Shri Hukum Poems Price Rise Dev Narayan Yadav 10 28.7.2016 Discussion under Rule 193 on Shri Tariq Couplet . Price Rise Anwar 11 28.7.2016 Discussion under Rule 193 on Shri Jai Prakash Poem . Price Rise Narayan Yadav 12 28.7.2016 Discussion under Rule 193 on Shri Rajesh Poem . -

4 (16Th LOK SABHA )
Election Commission of India, General Elections, 2014 (16th LOK SABHA ) 4 - LIST OF SUCCESSFUL CANDIDATES CONSTITUENCY Category WINNER Social Category PARTY PARTY SYMBOL MARGIN Andaman & Nicobar Islands 1 Andaman & GEN Bishnu Pada Ray GEN BJP Lotus 7812 Nicobar Islands ( 4.14 %) Andhra Pradesh 2 Adilabad ST Godam Nagesh ST TRS Car 171290 ( 16.65 %) 3 Amalapuram SC Dr Pandula Ravindra SC TDP Bicycle 120576 Babu ( 10.82 %) 4 Anakapalli GEN Muttamsetti Srinivasa GEN TDP Bicycle 47932 Rao (Avanthi) ( 4.21 %) 5 Anantapur GEN J.C. Divakar Reddi GEN TDP Bicycle 61991 ( 5.15 %) 6 Aruku ST Kothapalli Geetha ST YSRCP Ceiling Fan 91398 ( 10.23 %) 7 Bapatla SC Malyadri Sriram SC TDP Bicycle 32754 ( 2.78 %) 8 Bhongir GEN Dr. Boora Narsaiah GEN TRS Car 30544 Goud ( 2.54 %) 9 Chelvella GEN Konda Vishweshwar GEN TRS Car 73023 Reddy ( 5.59 %) 10 Chittoor SC Naramalli Sivaprasad SC TDP Bicycle 44138 ( 3.70 %) 11 Eluru GEN Maganti Venkateswara GEN TDP Bicycle 101926 Rao (Babu) ( 8.54 %) 12 Guntur GEN Jayadev Galla GEN TDP Bicycle 69111 ( 5.59 %) 13 Hindupur GEN Kristappa Nimmala GEN TDP Bicycle 97325 ( 8.33 %) 14 Hyderabad GEN Asaduddin Owaisi GEN AIMIM Kite 202454 ( 20.95 %) 15 Kadapa GEN Y.S. Avinash Reddy GEN YSRCP Ceiling Fan 190323 ( 15.93 %) 16 Kakinada GEN Thota Narasimham GEN TDP Bicycle 3431 ( 0.31 %) 17 Karimnagar GEN Vinod Kumar GEN TRS Car 204652 Boinapally ( 18.28 %) 18 Khammam GEN Ponguleti Srinivasa GEN YSRCP Ceiling Fan 12204 Reddy ( 1.04 %) 19 Kurnool GEN Butta Renuka GEN YSRCP Ceiling Fan 44131 ( 4.18 %) 20 Machilipatnam GEN Konakalla Narayana GEN TDP Bicycle 81057 Rao ( 7.15 %) 21 Mahabubabad ST Prof. -

Lok Sabha Secretariat
LOK SABHA SECRETARIAT Details of expenditure incurred on HS/HDS/LOP/MP(s)* During the Period From 01/11/2014 To 30/11/2014 Office Salary for Arrears(if SL ICNO Name of MP/ Salary Constituency Travelling/ Expense/ Available) State Allowance Secretarial daily Sumptury Assistant Allowence Allowance 160001 Shri Godam Nagesh 1 50000 45000 15000 30000 0 0 Andhra Pradesh 160002 Shri Balka Suman 2 50000 45000 15000 30000 0 0 Andhra Pradesh 160003 Shri Vinod kumar 3 50000 45000 15000 30000 140605 Boianapalli 0 Andhra Pradesh 160004 Smt. Kalvakuntla Kavitha 4 50000 45000 15000 30000 1064644 0 Andhra Pradesh 160005 Shri Bheemrao 5 50000 45000 15000 30000 498828 Baswanthrao Patil 0 Andhra Pradesh 160006 Shri Kotha Prabhakar 6 50000 45000 15000 75000 0 Reddy 0 Andhra Pradesh 160007 Ch.Malla Reddy 7 50000 45000 15000 30000 25986 0 Andhra Pradesh 160008 Shri Bandaru Dattatreya 8 0 0 0 0 0 0 Andhra Pradesh 160009 Shri Owaisi Asaduddin 9 50000 45000 15000 30000 0 0 Andhra Pradesh 160010 Shri Konda Vishweshar 10 50000 45000 15000 30000 0 Reddy 0 Andhra Pradesh 160011 Shri A.P.Jithender Reddy 11 50000 45000 15000 30000 425466 0 Andhra Pradesh 160012 Shri Yellaiah Nandi 12 50000 45000 15000 30000 0 0 Andhra Pradesh 160013 Shri Guntha Sukender 13 50000 45000 15000 30000 425437 Reddy 0 Andhra Pradesh 160014 Dr.Boora Narsaiah Goud 14 50000 45000 15000 30000 68974 0 Andhra Pradesh 160015 Shri Kadiyam Srihari 15 50000 45000 15000 30000 112775 0 Andhra Pradesh 160016 Prof. Azmeera Seetaram 16 50000 45000 15000 30000 326937 Naik 0 Andhra Pradesh 160017 ShriPonguleti Srinivasa 17 50000 45000 15000 30000 298637 Reddy 0 Andhra Pradesh LOK SABHA SECRETARIAT Details of expenditure incurred on HS/HDS/LOP/MP(s)* During the Period From 01/11/2014 To 30/11/2014 Office Salary for Arrears(if SL ICNO Name of MP/ Salary Constituency Travelling/ Expense/ Available) State Allowance Secretarial daily Sumptury Assistant Allowence Allowance 160018 Smt. -

Annual Report 2015-2016
MEMBERS OF PARLIAMENT LOCAL AREA DEVELOPMENT SCHEME (MPLADS) ANNUAL REPORT 2015-16 GOVERNMENT OF INDIA MINISTRY OF STATISTICS AND PROGRAMME IMPLEMENTATION EAST BLOCK-6, R.K. PURAM, NEW DELHI-110066 Website: www.mplads.gov.in INDEX PART- I Background and Policy 1 1.1 Background 3 1.2 Salient features of the Scheme 3 1.3 Procedure for Release of funds 6 1.4 Transparency and Accountability 8 PART- II National Implementation Status 9 2.1 Release of funds 11 2.2 Performance and Achievements 12 2.2.1 Cumulative Achievements (till 31.03.2016) 12 2.2.2 Achievements during 2015-16 13 2.3 Other Achievements 13 2.3.1 Rehabilitation works in flash flood and landslide affected areas of 13 Jammu and Kashmir 2.3.2 Uttarakhand flash floods/landslides and cloudburst 13 2.3.3 Hudhud Cyclone – Andhra Pradesh (Year 2014) 13 2.3.4 Rehabilitation Works in Tamil Nadu 13 2.3.5 Integrated MPLADS Portal 14 2.3.6 All India Review Meetings on MPLADS 16 2.3.7 Training of District Officials 16 PART- III State/UT wise Implementation Status 17 3.1 Andhra Pradesh 19 3.2 Arunachal Pradesh 22 3.3 Assam 24 3.4 Bihar 27 3.5 Chhattisgarh 31 3.6 Goa 34 3.7 Gujarat 36 3.8 Haryana 40 3.9 Himachal Pradesh 43 3.10 Jammu & Kashmir 45 3.11 Jharkhand 47 3.12 Karnataka 50 3.13 Kerala 54 3.14 Madhya Pradesh 57 3.15 Maharashtra 61 3.16 Manipur 66 3.17 Meghalaya 68 3.18 Mizoram 70 3.19 Nagaland 72 3.20 Odisha 74 3.21 Punjab 77 3.22 Rajasthan 80 3.23 Sikkim 83 3.24 Tamil Nadu 85 3.25 Telangana 90 3.26 Tripura 93 3.27 Uttar Pradesh 95 3.28 Uttarakhand 102 3.29 West Bengal 104 3.30 Andman