Generalized Anxiety Disorder: Practical Assessment and Management MICHAEL G
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Specificity of Psychosis, Mania and Major Depression in A
Molecular Psychiatry (2014) 19, 209–213 & 2014 Macmillan Publishers Limited All rights reserved 1359-4184/14 www.nature.com/mp ORIGINAL ARTICLE Specificity of psychosis, mania and major depression in a contemporary family study CL Vandeleur1, KR Merikangas2, M-PF Strippoli1, E Castelao1 and M Preisig1 There has been increasing attention to the subgroups of mood disorders and their boundaries with other mental disorders, particularly psychoses. The goals of the present paper were (1) to assess the familial aggregation and co-aggregation patterns of the full spectrum of mood disorders (that is, bipolar, schizoaffective (SAF), major depression) based on contemporary diagnostic criteria; and (2) to evaluate the familial specificity of the major subgroups of mood disorders, including psychotic, manic and major depressive episodes (MDEs). The sample included 293 patients with a lifetime diagnosis of SAF disorder, bipolar disorder and major depressive disorder (MDD), 110 orthopedic controls, and 1734 adult first-degree relatives. The diagnostic assignment was based on all available information, including direct diagnostic interviews, family history reports and medical records. Our findings revealed specificity of the familial aggregation of psychosis (odds ratio (OR) ¼ 2.9, confidence interval (CI): 1.1–7.7), mania (OR ¼ 6.4, CI: 2.2–18.7) and MDEs (OR ¼ 2.0, CI: 1.5–2.7) but not hypomania (OR ¼ 1.3, CI: 0.5–3.6). There was no evidence for cross-transmission of mania and MDEs (OR ¼ .7, CI:.5–1.1), psychosis and mania (OR ¼ 1.0, CI:.4–2.7) or psychosis and MDEs (OR ¼ 1.0, CI:.7–1.4). -

Which Is It: ADHD, Bipolar Disorder, Or PTSD?
HEALINGHEALINGA PUBLICATION OF THE HCH CLINICIANS’ HANDSHANDS NETWORK Vol. 10, No. 3 I August 2006 Which Is It: ADHD, Bipolar Disorder, or PTSD? Across the spectrum of mental health care, Anxiety Disorders, Attention Deficit Hyperactivity Disorders, and Mood Disorders often appear to overlap, as well as co-occur with substance abuse. Learning to differentiate between ADHD, bipolar disorder, and PTSD is crucial for HCH clinicians as they move toward integrated primary and behavioral health care models to serve homeless clients. The primary focus of this issue is differential diagnosis. Readers interested in more detailed clinical information about etiology, treatment, and other interventions are referred to a number of helpful resources listed on page 6. HOMELESS PEOPLE & BEHAVIORAL HEALTH Close to a symptoms exhibited by clients with ADHD, bipolar disorder, or quarter of the estimated 200,000 people who experience long-term, PTSD that make definitive diagnosis formidable. The second chronic homelessness each year in the U.S. suffer from serious mental causative issue is how clients’ illnesses affect their homelessness. illness and as many as 40 percent have substance use disorders, often Understanding that clinical and research scientists and social workers with other co-occurring health problems. Although the majority of continually try to tease out the impact of living circumstances and people experiencing homelessness are able to access resources comorbidities, we recognize the importance of causal issues but set through their extended family and community allowing them to them aside to concentrate primarily on how to achieve accurate rebound more quickly, those who are chronically homeless have few diagnoses in a challenging care environment. -

Mood Disorders and Trauma- What Are the Associations? Yael Dvir M.D., Michael Hill B.S, Steven M Hodge M.A., Jean a Frazier M.D
Mood Disorders and Trauma- What are the Associations? Yael Dvir M.D., Michael Hill B.S, Steven M Hodge M.A., Jean A Frazier M.D. University of Massachusetts Medical School, Child and Adolescent psychiatry [email protected] Background Results Mood dysregulation in traumatized children may be misdiagnosed as bipolar disorder (BD) TABLE 1: Demographic data and conversely, the diagnosis of BD overlooked. Note: test statistic is p-value of Chi-square test for categorical data or t-test for continuous data (corrected for unequal variance) BP MD-NOS Statistic* Our aim is to characterize the relationship between trauma and mood dysregulation and Group size (N) 10 10 . pediatric BD by describing the clinical correlates and demographics of children with Gender (number of Females) 4 4 1.0 trauma/abuse and comorbid mood disorders in a community mental health setting. Ethnicity (% Caucasian) 100 78 0.07 Age at time of Interview (mean (SD)) 13.2 (2.5) 12.5 (3.1) 0.6 Number of Siblings (mean (SD)) 2.2 (1.5) 1.8 (1.4) 0.6 Such distinctions may be especially important among individuals with BD given the disproportionably high prevalence of childhood trauma histories (reported in about half of TABLE 2: Types of trauma experienced and the number of incidents by group adult patients with BD, across several studies) coupled with frequent prepubertal onset of Type of Trauma BP MD-NOS affective symptoms (1-4), significantly younger age at bipolar illness onset, as well as Witnessed violence 8 7 Sexual assault or abuse 7 5 higher severity level of symptoms (3). -

Chapter 2 Mood Disorders
A Report on Mental Illnesses in Canada CHAPTER 2 MOOD DISORDERS Highlights • Mood disorders include major depression, bipolar disorder (combining episodes of both mania and depression) and dysthymia. • Approximately 8% of adults will experience major depression at some time in their lives. Approximately 1% will experience bipolar disorder. • The onset of mood disorders usually occurs during adolescence. • Worldwide, major depression is the leading cause of years lived with disability, and the fourth cause of disability- adjusted life years (DALYs). • Mood disorders have a major economic impact through associated health care costs as well as lost work productivity. • Most individuals with a mood disorder can be treated effectively in the community. Unfortunately, many individuals delay seeking treatment. • Hospitalizations for mood disorders in general hospitals are approximately one and a half times higher among women than men. • The wide disparity among age groups in hospitalization rates for depression in general hospitals has narrowed in recent years, because of a greater decrease in hospitalization rates in older age groups. • Hospitalization rates for bipolar disorder in general hospitals are increasing among women and men between 15 and 24 years of age. • Individuals with mood disorders are at high risk of suicide. 31 A Report on Mental Illnesses in Canada What Are Mood Disorders? Mood disorders may involve depression only with the illness progresses. (also referred to as “unipolar depression”) or Both depressive and manic episodes can they may include manic episodes (as in change the way an individual thinks and bipolar disorder, which is classically known as behaves, and how his/her body functions. -

Fact Sheet About Dysthymia
FACT SHEET 5 L Dysthymia What Is Dysthymia? Between 1 and 2 percent of people experience dysthymia (or dysthymic disorder) at some time during their lives. Dysthymia is a type of low-grade depression that lasts for at least two years. Dysthymia is less severe than major depression, but the chronic symptoms often have negative effects on work, relationships, and family and social interactions. Typically, having dysthymia means feeling mildly or moderately depressed more often than not. This may or may not be intertwined with periods of no symptoms or with periods of extreme symptoms or depressive episodes. Though dysthymia may result in an intense, short-term depressive episode, the symptoms are more constant and long term. People with dysthymia may even believe their depressive symptoms are their normal state of being. What Dysthymia Is Not Dysthymia is not just the typical feelings of sadness or withdrawal from other people that may occur when grieving a loss or while adjusting to a life change such as a divorce or job change. These common reactions usually last for a short time. Dysthymia should also not be confused with the depressant effects of long-term sub- stance use, particularly alcoholism. Sometimes dark and negative moods are associated with withdrawal from or cravings for substances. In early recovery, feelings of guilt, shame, grief, and regret typically arise. These are normal feelings as people come to terms with the consequences of their addiction. Experiencing and facing these feelings are important tasks of early recovery. What Are the Primary Symptoms of Dysthymia? Symptoms of dysthymia often overlap with symptoms of other depressive disorders, but they tend to be less intense. -

The Mood Disorder Questionnaire (MDQ)
The Mood Disorder Questionnaire (MDQ) Scoring Algorithm POSITIVE SCREEN All three of the following criteria must be met: Scoring: Question 1: 7/13 positive (yes) responses + Question 2: Positive (yes) response + Question 3: “moderate” or “serious” response This instrument is designed for screening purposes only and is not to be used as a diagnostic tool. *Derived from Hirschfeld RM. Am J Psychiatry. 2000:157(11):1873-5. The Mood Disorder Questionnaire (MDQ) INSTRUCTIONS: Please answer each question as best you can. YES NO 1. Has there ever been a period of time when you were not your usual self and... ... you felt so good or so hyper that other people thought you were not your normal self or you were so hyper that you got into trouble? ... you were so irritable that you shouted at people or started fights or arguments? ... you felt much more self-confident than usual? ... you got much less sleep than usual and found that you didn’t really miss it? ... you were more talkative or spoke much faster than usual? ... thoughts raced through your head or you couldn’t slow your mind down? ... you were so easily distracted by things around you that you had trouble concentrating or staying on track? ... you had much more energy than usual? ... you were much more active or did many more things than usual? ... you were much more social or outgoing than usual, for example, you telephoned friends in the middle of the night? ... you were much more interested in sex than usual? ... you did things that were unusual for you or that other people might have thought were excessive, foolish or risky? .. -

Bipolar Disorder Mania and Hypomania Prepared By: Dr
Bipolar Disorder Mania and Hypomania Prepared by: Dr. Anvesh Roy Psychiatry Resident, University of Toronto This is a review of Bipolar disorder focusing primarily upon its defining phenomena of Mania and Hypomania. The following text is envisioned to help case based learning of Bipolar Disorder by providing a background context (the video case). This is designed to show how the scenario may present in real life when you are faced with a similar patient rotating through the ER or in an inpatient unit. Click on the following hyperlinks to arrive at each section with pertinent examples from our video case (commiserate to enabling objectives): . What is Mania and Hypomania? Definition and meaning. Differential Diagnosis . How to get a history and pertinent information . Objective evaluation: Physical Exam and MSE . What are the investigations? . Management . Short Term, including addressing safety concerns and acute agitation . Long Term . References and further reading (for the so inclined) Bipolar Disorder - Mania and Hypomania Prepared by Dr. Anvesh Roy for HUB Psychiatry, Faculty of Medicine, University of Toronto Page 1 of 18 What is Mania (and Hypomania)? An extremely disabling and potentially harmful behavioral syndrome that indicates an underlying central nervous system disorder. Mania can lead to harm to self or others, and may be accompanied by features of psychosis. Hypomania is a less severe form of mania, see later on in the text how to differentiate between the two. Usually, by definition they denote affliction by one of the various forms of Bipolar Disorders or ‘Bipolar Spectrum’ of disorders. They can be secondary to other causes, but then they are not referred to as such, as will be explained. -
What Is Bipolar Disorder? What Is a Manic Episode?
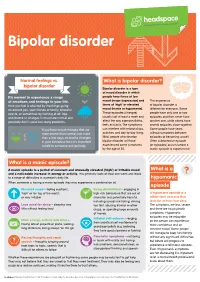
Bipolar disorder Normal feelings vs. What is bipolar disorder? bipolar disorder Bipolar disorder is a type of mood disorder in which It’s normal to experience a range people have times of low of emotions and feelings in your life. mood (major depression) and The experience How you feel is affected by the things going times of ‘high’ or elevated of bipolar disorder is on around you, your friends or family, stressful mood (mania or hypomania). different for everyone. Some events, or sometimes by nothing at all. Ups These episodes (changes) people have only one or two and downs or changes in mood are normal and usually last at least a week and episodes and then never have generally don’t cause too many problems. affect the way a person thinks, another one, while others have feels and acts. The symptoms several episodes close together. If you have mood changes that are can interfere with relationships, Some people have years more severe than normal, last more activities and day-to-day living. without symptoms between than a few days, or lead to changes Most people who develop episodes of becoming unwell. in your behaviour then it’s important bipolar disorder will have Often a depressive episode to talk to someone and get help. experienced some symptoms (or episodes) occurs before a by the age of 25. manic episode is experienced. What is a manic episode? A manic episode is a period of constant and unusually elevated (‘high’) or irritable mood What is a and a noticeable increase in energy or activity. -

An Overview of Mood Disorders/Depression
An Overview of Mood Disorders/Depression Written by Jennifer L. Horn, PhD, HSPP OVERVIEW OF MOOD DISORDERS Mood disorders are biological disorders that affect children, adolescents, and adults. Depression and other mood disorders are not being ‘down in the dumps’ or easily upset, but serious medical disorders that affect thinking, emotions, and behavior for months to even years if left untreated. Research suggests that about 15- 20% of the population will experience a mood disorder at some point in their life. Females are much more likely to develop a mood disorder, yet males are much more likely to go without treatment. Research has demonstrated physical differences in the brain of people affected with mood disorders. No matter the age of the person, mood disorders present with similar symptoms. Symptoms include sad or unhappy mood that lasts for days at a time, vegetative symptoms such as lack of energy or motivation, somatic symptoms such as changes in eating or sleeping habits, feelings of helplessness, irritability/moodiness, and feelings of hopelessness including suicidal thoughts. Although there is no one cause of mood disorders and depression, research clearly reflects a genetic predisposition to develop a mood disorder. Studies have shown that mood disorders and depression are common among close relatives, and twin studies have also shown a strong genetic basis. Additionally, research has shown that people who tend to be more negative and have low self-esteem are more likely to develop a mood disorder. In addition to the genetic causes of mood disorders, studies have also shown that environmental and interpersonal stressors can trigger mood disorders and depression, especially in those who are already thought to be at risk. -

Schizoaffective Disorder?
WHAT IS SCHIZOAFFECTIVE DISORDER? BASIC FACTS • SYMPTOMS • FAMILIES • TREATMENTS RT P SE A Mental Illness Research, Education and Clinical Center E C I D F I A C VA Desert Pacific Healthcare Network V M R E E Long Beach VA Healthcare System N T T N A E L C IL L LN A E IC S IN Education and Dissemination Unit 06/116A S R CL ESE N & ARCH, EDUCATIO 5901 E. 7th street | Long Beach, CA 90822 basic facts Schizoaffective disorder is a chronic and treatable psychiatric Causes illness. It is characterized by a combination of 1) psychotic symp- There is no simple answer to what causes schizoaffective dis- toms, such as those seen in schizophrenia and 2) mood symptoms, order because several factors play a part in the onset of the dis- such as those seen in depression or bipolar disorder. It is a psychi- order. These include a genetic or family history of schizoaffective atric disorder that can affect a person’s thinking, emotions, and be- disorder, schizophrenia, or bipolar disorder, biological factors, en- haviors and can impact all aspects of daily living, including work, vironmental stressors, and stressful life events. school, social relationships, and self-care. Research shows that the risk of schizoaffective disorder re- Schizoaffective disorder is considered a psychotic disorder sults from the influence of genes acting together with biological because of its prominent features of hallucinations and delusions. and environmental factors. A family history of schizoaffective dis- Therefore, people with this illness have periods when they have order does not necessarily mean children or other relatives will difficulty understanding the reality around them. -

Irritability, Disruptive Mood Dysregulation Disorder, and Bipolar Disorder
Pediatric Mood Dysregulation: Irritability, Disruptive Mood Dysregulation Disorder, and Bipolar Disorder William P. French, MD March 24, 2018 Disclosure of Potential Conflicts Source Disclosure Pfizer, Shire, & Supernus Research Funding Pharmaceuticals Books, Intellectual Property none Advisor/ Consultant none Speakers’ Bureau Symposia Medicus Employee none In-kind Services (example: travel) Symposia Medicus Stock or Equity none Honorarium or expenses for this Symposia Medicus presentation or meeting Today’s agenda • Irritability • Disruptive Mood Dysregulation Disorder • Severe Mood Dysregulation • Pediatric Bipolar Disorder • Yes, its controversial and rare, but it does exist • DSM 5 diagnostic criteria • Assessment • Medication and non-medication treatments • Take home message Key Points in Today’s Presentation • Irritability and/or “mood swings” don’t equal pediatric bipolar disorder (PBD). Irritability (a potential presenting complaint in bipolar mania) is a non-specific, common symptom present in many childhood psychiatric illnesses. • Multiple factors have led to a significant increase the diagnosis of PBD, leading to inappropriate prescribing of medications (e.g., antipsychotics) with serious side effect burdens. • NIMH research has worked to clarify unique neurobiological substrates and clinical courses in youth presenting with chronic vs. episodic irritability • PBD, while a “zebra” and not a “horse” does occur in youth, especially in the context of a strong family history. • Youth presenting with acute mania, ideally, should -

Management of Major Depressive Disorder(MDD)
ClinicalPracticeGuideline SUMMARY Managementof MajorDepressiveDisorder(MDD) May,2009 VA/DoDEvidenceBasedPractice VA/DoD CLINICAL PRACTICE GUIDELINE FOR MANAGEMENT OF MAJOR DEPRESSIVE DISORDER (MDD) Department of Veterans Affairs Department of Defense SUMMARY QUALIFYING STATEMENTS The Department of Veterans Affairs (VA) and The Department of Defense (DoD) guidelines are based on the best information available at the time of publication. They are designed to provide information and assist in decision-making. They are not intended to define a standard of care and should not be construed as one. Also, they should not be interpreted as prescribing an exclusive course of management. Variations in practice will inevitably and appropriately occur when providers take into account the needs of individual patients, available resources, and limitations unique to an institution or type of practice. Every healthcare professional making use of these guidelines is responsible for evaluating the appropriateness of applying them in any particular clinical situation. Version 2.0 – 2008 VA/DoD Clinical Practice Guideline For Management of Major Depressive Disorder Table of Contents Page Introduction 1 Guideline Update Working Group 3 Key Elements Addressed by the Guideline 4 Algorithms and Annotations 6 Appendices Appendix A: Guideline Development process (See full guideline) Appendix B: Screening and Assessment Instruments B-1. Quick Guide to the Patient Health Questionnaire (PHQ) B-2. Example of Diagnosing MDD & Calculating PHQ-9 Score B-3. PHQ-9 Scores and Proposed Treatment Actions B-4. Nine Symptom Checklist (PHQ-9) Appendix C: Suicidality (See full guideline) Appendix D: Pharmacotherapy D- 1. Antidepressant Dosing and Monitoring D-2. Antidepressant Adverse Effects Appendix E: Participants list (See full guideline) Appendix F: Acronym List Appendix G: Bibliiography (See full guideline) Table of Contents VA/DoD Clinical Practice Guideline For Management of Major Depressive Disorder Introduction Major Depressive Disorder (MDD) Depression is a major cause of disability worldwide.