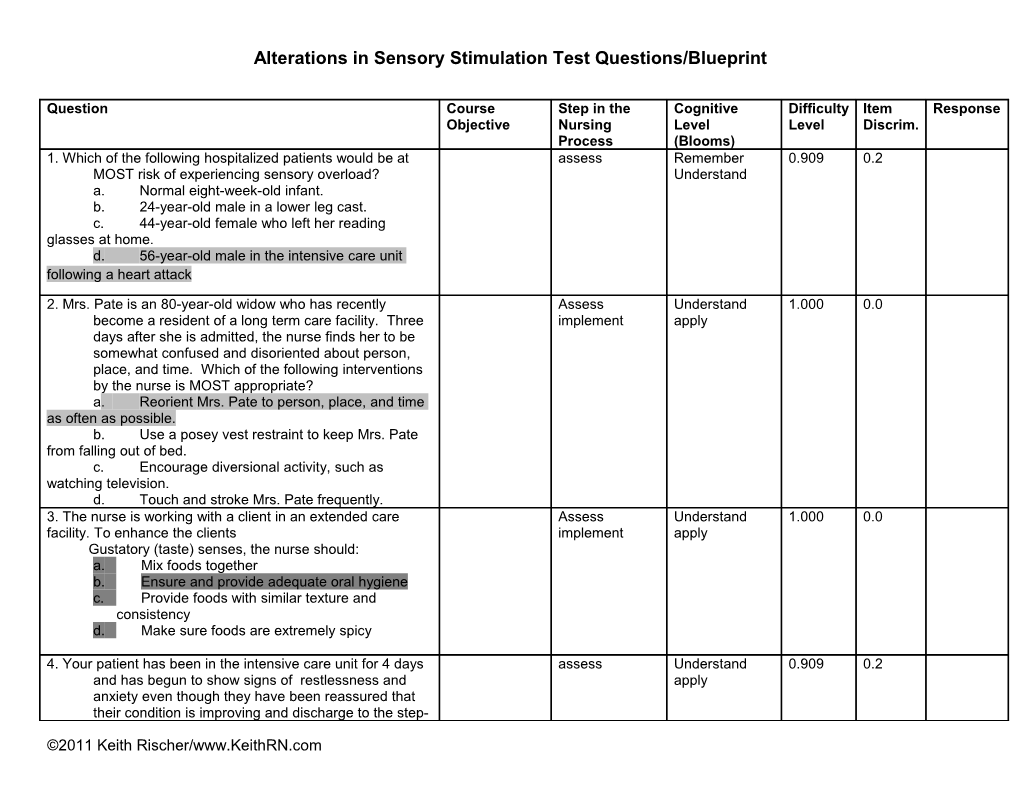
Alterations in Sensory Stimulation Test Questions/Blueprint
Question Course Step in the Cognitive Difficulty Item Response Objective Nursing Level Level Discrim. Process (Blooms) 1. Which of the following hospitalized patients would be at assess Remember 0.909 0.2 MOST risk of experiencing sensory overload? Understand a. Normal eight-week-old infant. b. 24-year-old male in a lower leg cast. c. 44-year-old female who left her reading glasses at home. d. 56-year-old male in the intensive care unit following a heart attack
2. Mrs. Pate is an 80-year-old widow who has recently Assess Understand 1.000 0.0 become a resident of a long term care facility. Three implement apply days after she is admitted, the nurse finds her to be somewhat confused and disoriented about person, place, and time. Which of the following interventions by the nurse is MOST appropriate? a. Reorient Mrs. Pate to person, place, and time as often as possible. b. Use a posey vest restraint to keep Mrs. Pate from falling out of bed. c. Encourage diversional activity, such as watching television. d. Touch and stroke Mrs. Pate frequently. 3. The nurse is working with a client in an extended care Assess Understand 1.000 0.0 facility. To enhance the clients implement apply Gustatory (taste) senses, the nurse should: a. Mix foods together b. Ensure and provide adequate oral hygiene c. Provide foods with similar texture and consistency d. Make sure foods are extremely spicy
4. Your patient has been in the intensive care unit for 4 days assess Understand 0.909 0.2 and has begun to show signs of restlessness and apply anxiety even though they have been reassured that their condition is improving and discharge to the step-
©2011 Keith Rischer/www.KeithRN.com down unit will be occurring soon. The cause of the client’s emotional state is likely a result of: a. Fear of death b Social isolation c Sensory overload d Anxiety disorder
5. . When obtaining a health history from a patient, assess Understand 0.987 0.1 which statement will be of most concern to the nurse? apply a. “My vision seems blurry now when I read the last few weeks” b. “I have noticed that my eyes are drier now” c. “It’s hard for me to see when I drive at night” d. “The middle part of my vision has decreased suddenly today”
6. The nurse is obtaining a health history for a 64-year-old assess Understand 0.935 -0.2 patient with glaucoma who is a apply new patient at the eye clinic. Which information given by the patient will have the most implications for which eye drops will be used to treat her? a. “I use aspirin when I have a sinus headache” b. “I have not had an eye examination for at least 10 years” c. “I take metoprolol daily for angina” d. “I have had frequent episodes of conjunctivitis” 6. 7. Carbonic anhydrase inhibitors such as Diamox may be assess Understand 0.558 0.3 given to patients with glaucoma to: apply a. Constrict the pupil to open the angle. b. Draw fluid from the eye into vascular circulation. c. Decrease production of aqueous humor. d. Increase outflow of aqueous humor. 8. When administering Timolol (timoptic) eye gtts, it is assess Understand 0.766 0.2 important for the nurse to do, or educate the patient to apply do this after administering: a. Assess heart rate before administering b. Maintain pressure over the lacrimal sac to prevent ©2011 Keith Rischer/www.KeithRN.com systemic absorption c. Administer at bedtime to decrease side effects d. a & b 9. The nurse is caring for a patient with conjunctivitis of the implement Understand 1.000 0.0 left eye who apply has Sulfacetamide eye drops prescribed for use in the affected eye. The nurse explains that to help prevent the spread of infection, the patient should: a. Apply an occlusive dressing to the affected eye b. Avoid touching the eyes and wash hands frequently c. Use the eye drops in both eyes as a prophylactic measure d. Apply corticosteroid ointment to the right eye to decrease the risk of inflammation
10. A patient is prepared for discharge following outpatient Implement Understand 0.935 0.0 cataract surgery. To evaluate apply whether the patient understands the postoperative regimen and procedures, the nurse asks the patient: a. To use the 0 to 10 pain scale to rate eye pain b. To demonstrate administration of prescribed eye drops c. To state how good the vision is in the operative eye d. Why staying on bed rest for 24 hours is needed
11. A patient who had cataract extraction and intraocular lens Assess Understand 0.740 0.5 implantation the previous Apply day calls the eye clinic and gives the nurse the evaluate following information. Which information is of most concern to the nurse? a. The patient has rated their eye pain at a 5 (on a 0-10 scale) b. The patient complains that their vision has not improved tremendously c. The patient has poor depth perception when wearing an eye patch d. The patient has questions about the ordered ©2011 Keith Rischer/www.KeithRN.com eye drops 12. . A patient who has heart failure and has been assess Understand 0.779 0.3 receiving large doses if IV furosemide apply (Lasix) tells the nurse, “I cannot hear very well. My ears are ringing” The most appropriate action by the nurse is to a. Arrange for the patient to have a hearing test b. Withhold the ordered dose of furosemide and notify the physician c. Tell the patient that these symptoms are temporary d. Add the nursing diagnosis of disturbed auditory perception related to ototoxicity to the patient’s care plan 13. 1120-XI-9 A patient with Meniere’s disease is admitted implementation Understand 0.883 0.3 with vertigo, nausea, and vomiting. Which apply nursing intervention will be included in the care plan? a. Encourage oral fluids to 3000mL daily b. Change the patient’s position every 2 hours c. Keep the head of the bed elevated 15 degrees d. Keep the patient’s room darkened 14. The most appropriate nursing action for a patient with implement Understand 0.805 0.2 epistaxis is: apply a. Decrease exposure to allergens. b. Heated mist and saline irrigation. c. Application of ice or cool compresses to the nasal bridge. d. Direct pressure to the lower portion of nose. e. c & d 15. The use of a hearing aid is most effective for which of the assess Understand 0.935 0.0 following conditions? apply a. Conductive hearing loss b. Serous otitis media c. Tinnitis d. Sensorineural hearing loss 16 The patient you are caring for has dysarthria. Which Assess Understand 0.701 0.5 nursing action is most implement apply appropriate? a. Place objects within the patient’s reach on the non-affected side. b. Provide a supportive device for ambulation.
©2011 Keith Rischer/www.KeithRN.com c. Place food on the unaffected side of the mouth. d. Provide the patient with alternative methods of communicating.
17. The daughter of a patient admitted unconscious to the assess Understand 0.831 0.3 ER with a possible stroke apply reports that her mother has a history of hypertension that she does not manage well. She has been using estrogen replacement therapy for the past 6 years, and estrogen and her antihypertensive medication are the only drugs she uses. Her only activity is managing her home, and she appears quite overweight. The finding that the nurse recognizes as the most significant risk factor for stroke in this patient is a. Obesity b. Hypertension c. Sedentary lifestyle d. Estrogen replacement therapy
18. A client has been admitted to the hospital after having a assess Understand 0.857 0.3 stroke. What predisposing apply factor in this patient’s history places this client at risk for an embolic stroke? a. A history of hypertension b. A history of psychotropic drug use c. A history of atrial fibrillation d. A history of cerebral aneurysm
19. The nurse identifies the nursing diagnosis of impaired Assess Understand 0.961 0.1 verbal communication for a patient with expressive Implement apply aphasia. An appropriate nursing intervention to help the patient communicate is to: a. Ask simple questions that the patient can answer with “yes” or “no.” b. Develop a list of words that the patient can read and practice reciting. c. Have the patient practice facial and tongue exercises to improve motor control necessary ©2011 Keith Rischer/www.KeithRN.com for speech. d. Prevent embarrassing the patient by changing the subject if the patient does not respond in a timely manner 20. A patient with a stroke has progressive development of Assess Understand 0.468 0.4 neurologic deficits with increasing weakness and implement apply decreased level of consciousness (LOC). The nursing priority that is most relevant to guide your care at this time will be: a. Risk for impaired skin integrity r/t immobility b. Disturbed sensory perception r/t brain injury c. Risk for aspiration r/t inability to protect airway d. Impaired physical mobility r/t weakness
KEY: Cognitive Level: Item Discrimination = how well an item distinguishes between high and low scoring students. Remembering 0 is OK if it’s info that everyone absolutely needs to know, i.e. key content. Understanding .2 to .3 is desirable for most Applying .4 or higher is OK for just a few questions. If all were .4, most of our students would fail the test. Analyzing Negative discrimination means a problem, like a poorly written question, mis-speaking in lecture, not fully clarifying a Evaluating topic, or an error on the answer key. Creating
FINAL EXAM
ALTERATION IN SENSORY STIMULATION (5) assess Understand 0.937 0.2
1. When obtaining a patient’s admission history, the patient states he has been using Timoptic (Timolol) eye drops for several months. The ©2011 Keith Rischer/www.KeithRN.com nurse is aware that this is usually prescribed to treat: a. Macular degeneration b. Cataracts c. Conjunctivitis d. Glaucoma 2. Your patient has a history of vision problems assess Understand 0.734 0.0 including a gradual loss of visual acuity and apply generalized blurry vision. The patient has no pain in the eyes. These symptoms are most usually associated with: a. Macular degeneration b. Conjunctivitis c. Myopia d. Cataracts 3. Your patient has two different eye drops implement Understand 0.835 0.0 ordered for a new diagnosis of glaucoma. How apply long should you teach to wait between successive eye drops in the same eye to achieve adequate eye drop drug retention and absorption? a. 1 minute b. 5 minutes c. c.30 minutes d. d.60 minutes 4. A patient admitted with a stroke is coming to assess Understand 0.949 0.1 your unit from the emergency department. apply What assessment data is indicative of a stroke? a. Facial droop b. Dysarthria c. hemiparesis d. a & b e. a, b, c 5. Your patient who suffered an ischemic stroke implement Understand 0.848 0.1 now has disturbed visual perception (visual apply field cut). What intervention will be required when caring for this patient? a. The patient should be approached on the side where visual perception is intact. b. Attention to the affected side should be minimized. ©2011 Keith Rischer/www.KeithRN.com c. The patient should avoid repetitious turning of his head in the direction of the defective visual field in order to minimize dizziness. d. The patient should be approached on the opposite side of where the visual perception is intact in order to increase perception and vision.
©2011 Keith Rischer/www.KeithRN.com