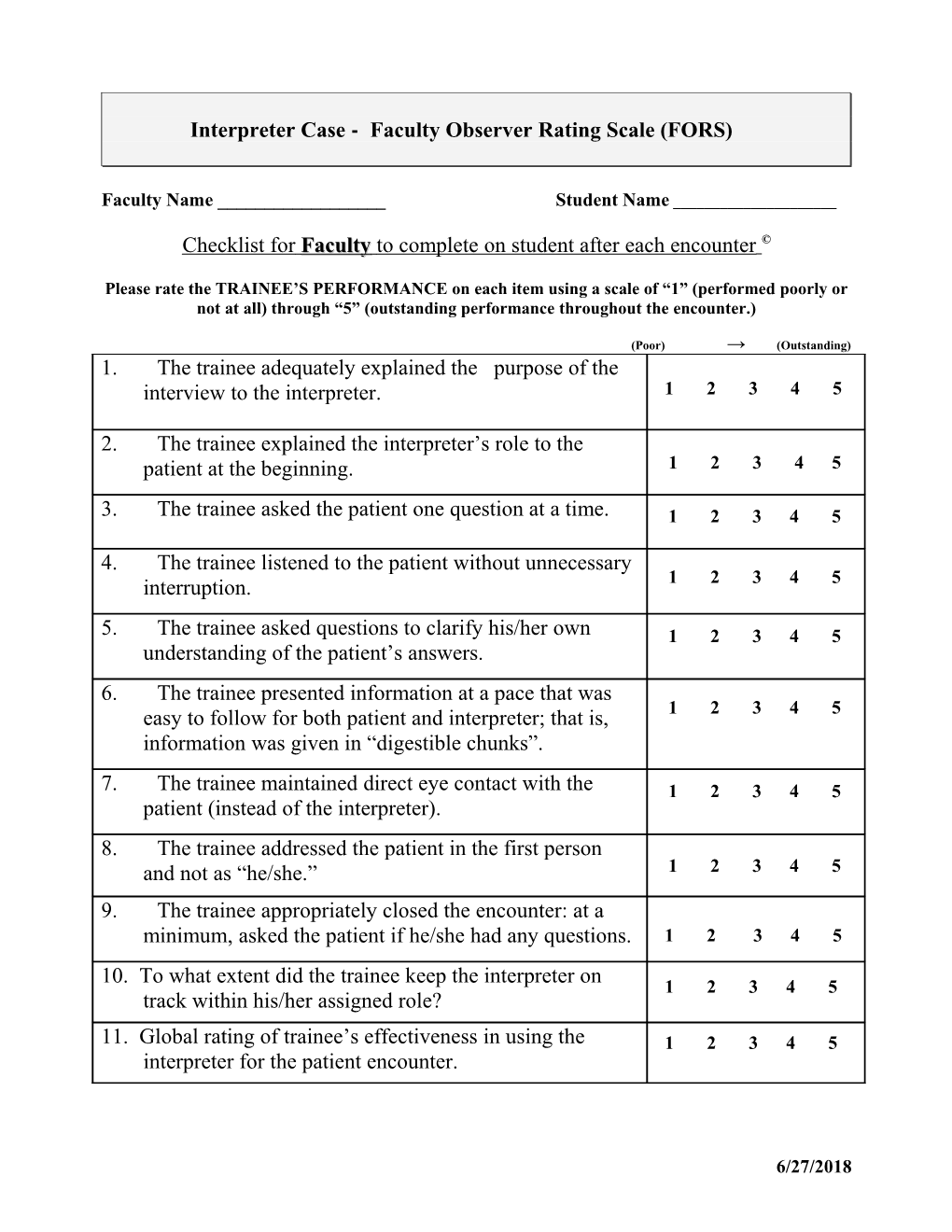
Interpreter Case - Faculty Observer Rating Scale (FORS)
Faculty Name ______Student Name ______
Checklist for Faculty to complete on student after each encounter ©
Please rate the TRAINEE’S PERFORMANCE on each item using a scale of “1” (performed poorly or not at all) through “5” (outstanding performance throughout the encounter.)
(Poor) → (Outstanding) 1. The trainee adequately explained the purpose of the interview to the interpreter. 1 2 3 4 5
2. The trainee explained the interpreter’s role to the patient at the beginning. 1 2 3 4 5
3. The trainee asked the patient one question at a time. 1 2 3 4 5
4. The trainee listened to the patient without unnecessary 1 2 3 4 5 interruption.
5. The trainee asked questions to clarify his/her own 1 2 3 4 5 understanding of the patient’s answers. 6. The trainee presented information at a pace that was 1 2 3 4 5 easy to follow for both patient and interpreter; that is, information was given in “digestible chunks”.
7. The trainee maintained direct eye contact with the 1 2 3 4 5 patient (instead of the interpreter). 8. The trainee addressed the patient in the first person and not as “he/she.” 1 2 3 4 5
9. The trainee appropriately closed the encounter: at a minimum, asked the patient if he/she had any questions. 1 2 3 4 5
10. To what extent did the trainee keep the interpreter on 1 2 3 4 5 track within his/her assigned role?
11. Global rating of trainee’s effectiveness in using the 1 2 3 4 5 interpreter for the patient encounter.
6/27/2018 Interpreter Case - Faculty Observer Rating Scale (FORS) Guide to the Checklist
Remember: the fundamental purpose of health care interpreters is to facilitate communication between two parties who do not speak the same language and may not share the same culture. In most situations, interpreters support and reinforce the primary relationship between the patient and provider.
1. The trainee adequately explained the purpose of the interview to the interpreter. Purpose: Trainee informs the interpreter on the background on the case at hand, done in the beginning of the encounter. OUTSTANDING: To interpreter (whether at once or over several exchanges): “Hello, I am X and I understand that you will interpret for us today. Thank you! I would ask that you interpret word-for-word what I and the patient say, and please let me know if something is unclear”or “According to my charts, Ms. Jones has been here in the past and used interpreter services, and today we will discuss her coughing” To patient: “As the interpreter will interpret, my understanding is that you have been here in the past and today we will discuss your coughing” AVERAGE: “I am X and this is Y, the interpreter. I see you’re here for your coughing today Ms. Jones.” POOR: If the trainee does not explain why the patient is visiting the clinic. “Hello, how are you today?’ without any introduction of the interpreter.
2. The trainee explained the interpreter’s role to the patient in the beginning Purpose: Set goals and create guidelines for the interpreter during the encounter in order for the interpreter to accurately facilitate the information exchange between the physician and the patient; indicate transparent interpreting. Informs the patient about how the interpreted encounter will proceed. OUTSTANDING: The trainee explains what is expected of the interpreter to the patient during the encounter, such as interpreting word for word and speaking in first person. Speaking to the patient: “Good morning/afternoon, Mr./Mrs Jones, I am Dr. Smith and will be spending 20 minutes interviewing today to help you. This is the interpreter Mr./Mrs. Zhu. Are you comfortable having him/her interpret? The interpreter will interpret the entire conversation for us word for word. Everything that I say and everything that you say will be interpreted to each other so that we can communicate clearly. The information will be confidential.” AVERAGE: The trainee makes mention to follow guidelines, but does not specify more than one category: “The interpreter will be here during the encounter” POOR: The trainee does not set guidelines during the encounter, begins the encounter without explaining what the interpretation expectation is.
3. The trainee asked the patient one question at a time
6/27/2018 Purpose: Manage the flow of communication and pacing the amount of information presented, to be processed by both the interpreter and patient. OUTSTANDING: The trainee generally asks the patient one question at a time: “I see that you have been here on visits before, were any of your previous visits related to similar coughing?” Pause for interpretation and response, when needed, before asking another question. AVERAGE: The trainee “slips” once or twice and asks multiple questions in a row, does not allow for smooth interpretation during the encounter. POOR: The trainee regularly asks multiple questions in one interpretation period: “Have you seen us before? And let me ask you, what did the other doctors tell you at that time? Please let me know if there are any results available”
4. The trainee listened to the patient without unnecessary interruption Purpose: Allows for facilitation of communication, ensures a non-rushed atmosphere OUTSTANDING: The trainee allows the interpretation to occur by attentively waiting patiently during the interpreted encounter, active listening and good non-verbal cues AVERAGE: The trainee is listening but interrupts once or twice, may be focused on other items POOR: The trainee interrupts the interpreter (such as when they add clarifying questions, etc)
5. The trainee asked questions to clarify the his/her understanding of the patient’s answers Purpose: "back interpretation" involves asking the patient to restate their understanding of what is being addressed in the encounter in order for the physician to better understand what the patient knows and also serves as a check on the quality of interpretation OUTSTANDING: The trainee asks one of the following questions: “Ms. Jones, can you please summarize for me your understanding of your treatment plan?” “We’ve gone over quite a bit here, so let me hear how you understand what I have told you about your illness” “Let me summarize what I think is going on and you can tell me if I’m correct …” AVERAGE: The trainee makes an attempt to discern the patient’s understanding “Please summarize our talk” “So, you’re in here for a cough that will not go away, is that correct?” POOR: The trainee does not ask for clarifying statements “OK?” or other close-ended statements do not count
6. The trainee presented information at a pace that was easy to follow for both patient and interpreter; that is, information was given in “digestible chunks”. Purpose: Communication style should be truncated for effective communication using interpreters since the intepreter has the job to relay the information. More information is preserved with “digestible chunks” of 1-2 sentences rather than expecting full paragraphs to be interpreted. OUTSTANDING: The trainee presented information and asked questions that were approximately 1-2 sentences long, allowed for the flow of conversation to occur, rather than having multiple one-sided conversations. AVERAGE: The trainee had a combination of long and reasonable-length conversation pieces. Or, the trainee tended to ask one more sentence (a little bit more) than necessary for comfort for interpreting.
6/27/2018 POOR: The trainee provided long-winded and extended conversation pieces for the interpreter
7. The trainee maintained direct eye contact with the patient (instead of the interpreter) Purpose: Promotes good non-verbal communication, allows for relationship-building between the provider and the patient. Reinforces the conversation between the provider and patient. OUTSTANDING: The trainee looks at the patient when the patient is talking and the trainee looks at the patient while speaking. Note: some “regular” distractions occur (i.e. writing, etc), but the emphasis is clearly concern to maintain eye contact at appropriate times. AVERAGE: The trainee looks at the patient while speaking, while the interpreter is speaking, and while the patient is speaking, but sometimes looks at the interpreter and no longer maintains eye contact with the patient. An “average” score reflects less time of eye contact with the patient than “outstanding” score. POOR: The trainee looks at the interpreter or notepad/etc while speaking, also looks at the interpreter when the patient is responding (and interpreter talking)
8. The trainee addressed the patient in the second-person, not as “he” or “she” Purpose: To facilitate better rapport and communication, the patient must be addressed in the second-person voice (interpreters will interpret word for word and will ask the question in the same “voice” as the original statement), and the trainee refers to themselves in the first-person voice. First- and second-person reinforces the primary relationship between the patient and the provider. Mimics how the patient and provider would speak to each other if they spoke the same language and could directly communicate. OUTSTANDING: The trainee uses the first- and second-person voice, speaks as if conversation does not have an interpreter (directly speaks to patient) “Ms. Jones, do you have any concerns you would like to bring up today?” “I believe that you need this treatment for your cough” AVERAGE: The trainee uses the first- and second-person voice but mixes third-person in irregularly. Some effort is made to maintain first- and second-person voice. POOR: The trainee speaks “through” the interpreter and only occasionally to rarely uses the first- or second-person voice. “Please tell Ms. Jones…” “She [referring to patient] has this problem, can you please tell her?” “She needs this prescription medicine, and she needs to make a follow-up appointment for next week”
9. The trainee appropriately closed the encounter: at a minimum, asked the patient if he/she had any questions Purpose: To ensure proper communication and greater comprehension by the patient, serves as a clarifier. Depending on the case, the student also provides information on next steps (i.e. discussing with an attending, offering solutions, etc) OUTSTANDING: The trainee asks one of the following or similar questions: “Ms. Jones, do you have any questions about your treatment?” “Do you have any concerns or questions about what we talked about today?” “Is there anything that we need to clarify or something that concerns you about what we talked about?” AVERAGE: The trainee attempts to discover if the patient has any questions, lesser emphasis than listed statements (above) POOR: The trainee fails to ask if the patient has any questions 6/27/2018 10. To what extent did the trainee keep the interpreter on track within his/her assigned role? Purpose: Physicians are responsible for the encounter that occurs during an office visit and should regularly check interpretation periodically during the visit. An initiation of this checklist item occurs with originally clarifying the role of the interpreter, but this item can be separately coded if the trainee makes recommendations during the encounter. The current SP-SI LEP case consists of an untrained interpreter where the language interpretation “mistakes” occur, such as omissions and abbreviations of responses, side conversations, using third-person voice, and interpreter interjections. The trainee is rated on how well they observe and respond to interpreted “mistakes” in order to effectively manage the encounter. OUTSTANDING: The trainee observes a “mistake” and immediately or shortly responds with: “I want to remind you that during this session I would like for you to interpret word for word so that I can communicate with the patient” “Excuse me, but it seems like you had a side conversation, would you please repeat what you discussed?” “I noticed that the patient had a much longer response. Please remember to interpret word for word during the encounter” AVERAGE: The trainee observes the mistake and allows the “mistake” to occur for a long period of time or responds later in the encounter (i.e. after multiple “mistakes”) POOR: The trainee allows the “mistakes” to occur and never responds with the encounter, or rudely reminds the interpreter what their role is.
13. Rate your OVERALL SATISFACTION with the encounter Purpose: Rate how effectively you believe that the trainee utilized the interpreter during the medical encounter. GOAL: the trainee’s role is to enhance the possibility of communication in the medical encounter using an interpreter. NOTE: The “appropriate scores” are guidelines and the overall satisfaction score is dependent on the overall feeling of the encounter.
MOST (5) / HIGH: The trainee was EXCEPTIONAL in using the interpreter and was able to maintain focus on the patient during the entire medical encounter. The trainee clearly explained the interpreter’s role (you knew the parameters of the encounter as well as the background, introductions occurred) and the trainee made the encounter with the patient feel as close to a same-language encounter as much as possible. This is an appropriate score when the trainee completed well/outstanding most of the checklist as well as external reactions to the encounter. The next lowest score is similar to this, but does not feel exceptional or at the fullest potential.
AVERAGE (3) / MEDIUM: The trainee did a GOOD job using the interpreter, sometimes forgot to speak in the first-person, perhaps made eye contact with the interpreter instead of the patient, and sometimes interrupted either the patient or the interpreter. The trainee was not overwhelmed by the presence of the interpreter, had a friendly demeanor during the encounter, but may have been somewhat distracted by the third person in the room and did not utilize the interpreter or the encounter to the fullest potential. This is an appropriate score when the trainee was GOOD for the majority of the items (ratings approx 3), but NOT EXCEPTIONAL, as well as external reactions to the encounter. The trainee did “just fine” during the encounter. The next lowest score is similar, but has fewer completed checklist items, and the trainee makes little effort to facilitate the interpreted encounter. 6/27/2018 LEAST (1) / LOW: The trainee POORLY used the interpreter during the encounter. The trainee consistently talked about the patient (not to the patient), did not manage the side conversations or changes/omissions in the encounter (or may not have been aware that they occurred). Little eye contact with patient, absolutely no introductions, or poor introductions, with little management during the encounter. This is an appropriate score when the trainee does not appropriately use the interpreter during the encounter, a substantial portion of the checklist items are “poor”, and makes little, if any, effort to facilitate the encounter.
6/27/2018