District Health Action Plan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Final BLO,2012-13
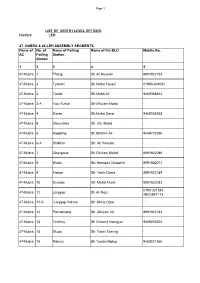
Page 1 LIST OF BOOTH LEVEL OFFICER . District: LEH 47- NUBRA & 48-LEH ASSEMBLY SEGMENTS. Name of No. of Name of Polling Name of the BLO Mobile.No. AC Polling Station Station 1 3 3 4 5 47-Nubra 1 Thang Sh.Ali Hussain 8991922153 47-Nubra 2 Tyakshi Sh.Mohd Yousuf 01980-248031 47-Nubra 3 Turtuk Sh.Mohd Ali 9469368812 47-Nubra 3-A Youl Turtuk Sh:Ghulam Mohd - 47-Nubra 4 Garari Sh.Mohd Omar 9469265938 47-Nubra 5 Chulunkha Sh: Gh. Mohd - 47-Nubra 6 Bogdang Sh.Ibrahim Ali 9469732596 47-Nubra 6-A Shilkhor Sh: Ali Hassain - 47-Nubra 7 Changmar Sh.Ghulam Mehdi 8991922086 47-Nubra 8 Waris Sh: Namgail Chosphel 8991922073 47-Nubra 9 Fastan Sh: Tashi Dawa 8991922149 47-Nubra 10 Sunudo Sh: Mohd Anvar 8991922082 0190-221344 47-Nubra 11 Largyap Sh Ali Rozi /9622957173 47-Nubra 11-A Largyap Yokma Sh: Nima Otzer - 47-Nubra 12 Pachathang Sh. Ghulam Ali 8991922182 47-Nubra 13 Terchey Sh Chemet Namgyal 9469266204 47-Nubra 14 Skuru Sh; Tashi Tsering - 47-Nubra 15 Rakuru Sh Tsetan Motup 9469221366 Page 2 47-Nubra 16 Udamaru Sh:Mohd Ali 8991922151 47-Nubra 16-A Shukur Sh: Sonam Tashi - 47-Nubra 17 Hunderi Sh: Tashi Nurbu 8991922110 47-Nubra 18 Hunder Sh Ghulam Hussain 9469177470 47-Nubra 19 Hundar Dok Sh Phunchok Angchok 9469221358 47-Nubra 20 Skampuk Sh: Lobzang Thokmed - 47-Nubra 21 Partapur Smt. Sari Bano - 47-Nubra 22 Diskit Sh: Tsering Stobdan 01980-220011 47-Nubra 23 Burma Sh Tuskor Tagais 8991922100 47-Nubra 24 Charasa Sh Tsewang Stobgais 9469190201 47-Nubra 25 Kuri Sh: Padma Gurmat 9419885156 47-Nubra 26 Murgi Thukje Zangpo 9419851148 47-Nubra 27 Tongsted -

1962 Sino-Indian Conflict : Battle of Eastern Ladakh Agnivesh Kumar* Department of Sociology, University of Mumbai, Mumbai, India
OPEN ACCESS Freely available online Journal of Political Sciences & Public Affairs Editorial 1962 Sino-Indian Conflict : Battle of Eastern Ladakh Agnivesh kumar* Department of Sociology, University of Mumbai, Mumbai, India. E-mail: [email protected] EDITORIAL protests. Later they also constructed a road from Lanak La to Kongka Pass. In the north, they had built another road, west of the Aksai Sino-Indian conflict of 1962 in Eastern Ladakh was fought in the area Chin Highway, from the Northern border to Qizil Jilga, Sumdo, between Karakoram Pass in the North to Demchok in the South East. Samzungling and Kongka Pass. The area under territorial dispute at that time was only the Aksai Chin plateau in the north east corner of Ladakh through which the Chinese In the period between 1960 and October 1962, as tension increased had constructed Western Highway linking Xinjiang Province to Lhasa. on the border, the Chinese inducted fresh troops in occupied Ladakh. The Chinese aim of initially claiming territory right upto the line – Unconfirmed reports also spoke of the presence of some tanks in Daulat Beg Oldi (DBO) – Track Junction and thereafter capturing it general area of Rudok. The Chinese during this period also improved in October 1962 War was to provide depth to the Western Highway. their road communications further and even the posts opposite DBO were connected by road. The Chinese also had ample animal In Galwan – Chang Chenmo Sector, the Chinese claim line was transport based on local yaks and mules for maintenance. The horses cleverly drawn to include passes and crest line so that they have were primarily for reconnaissance parties. -

Photographic Archives in Paris and London Pascale Dollfus
Photographic archives in Paris and London Pascale Dollfus To cite this version: Pascale Dollfus. Photographic archives in Paris and London. European bulletin of Himalayan research, University of Cambridge ; Südasien-Institut (Heidelberg, Allemagne)., 1999, Special double issue on photography dedicated to Corneille Jest, pp.103-106. hal-00586763 HAL Id: hal-00586763 https://hal.archives-ouvertes.fr/hal-00586763 Submitted on 10 Feb 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. EBHR 15- 16. 1998- 1999 PHOTOGRAPHIC ARCHIVES IN PARIS AND epal among the Limbu. Rai. Chetri. Sherpa, Bhotiya and Sunuwar. LONDO ' Both these collections encompa'\s pictures of land flY PA CALE DOLL FUSS scapes. architecture. techniques. agriculture. herding, lrade, feslivals. shaman practices. rites or passage. etc. In addition to these major collecti ons. once can find I. PUOTOGRAPfIIC ARCIUVES IN PARIS 350 photographs taken in 1965 by Jaeques Millot. (director of the RCP epal) in the Kathmandu Valley. Photographic Library ("Phototheque"), Musee de approx. 110 photographs (c. 1966-67) by Mireille Helf /'lIommc. fer. related primari Iy to musicians caSles, 45 photo 1'1. du Trocadero. Paris 750 16. graphs (1967-68) by Marc Gaborieau. -

O Level ST Candidates (Leh)
NATIONAL INSTITUTE OF ELECTRONICS & INFORMATION TECHNOLOGY,NIELIT J&K SUB CENTRE LEH LIST OF 'O'LEVEL STUDENTS BATCH:-DECEMBER (2013) S.NO App.No. Regn.No Level Name Father/Guardian Name Category Date of Birth Address 1 ROIT0614001604 964750 O KANIS FATIMA HASSAN ALI ST 29-जनवर -89 CHUCHOT LEH 2 ROIT0614002115 964759 O HASSINA BANO GHULAM HUSSAIN ST 02-अगत -92 SHEY SHEY 3 ROIT0614002075 964604 O NAMGYAL DOLMA SONAM THUKJEE ST 11-माच -95 HUNDER NUBRA LEH 4 ROIT0614002131 964610 O GULNAZ FATIMA MIRZA ASSADULLAH ST 11-मई -90 SHEY LEH 5 ROIT0614002113 964758 O SALEEM RAZA MOHD BAQIR ST 06-जनवर -89 SHEY SHEY 6 ROIT0614001595 964748 O HALIMA BANO GHULAM MOHD ST 13-मई -96 BASHAKA CHUCHOT YOKMA LEH 7 ROIT0614002061 964829 O ESHEY DOLMA TASHI WANGAIL ST 03-दसबर -89 TSATI SUMOOR NUBRA 8 ROIT0614002117 964608 O DEACHEN DOLMA TSERING NORBOO ST 21-माच -90 ZUNGPA CHAMSHEN SUMOOR NUBRA 9 ROIT0614001927 964600 O DORJAY DOLMA THUGJAY TUNDUP ST 05-जून -93 SHARA SHARA 10 ROIT0614001931 964602 O RIGZEN DOLMA TSEWANG CHONJOR ST 10-फरवर -92 SHANG LEH 11 ROIT0614002124 964834 O TSERING ANGMO TSEWANG DORJAY ST 28-जून -94 SUMOOR NUBRA LEH 12 ROIT0614002103 964832 O RIGZIN YANGDOL TASHI WANGIAL ST 01-नवबर -92 CHOGLAMSAR ZAMPA LEH 13 ROIT0614002131 964610 O KANIZ FATIMA MEHDI ALI ST 11-मई -90 SHEY LEH 14 ROIT0614002111 964607 O SONAM YANGCHAN TONDUP NAMGAIL ST 01-मई -93 PHUKPOCHEY SUMOOR NUBRA 15 ROIT0614002123 964760 O SHAHEEN KOUSAR MOHD YASSIN ST 20-फरवर -84 THASGAN THLINA KARGIL 16 ROIT0614002071 964603 O ANWAR HUSSAIN MIRZA HADI ST 03-जनवर -84 CHUCHOT YOKMA -

Course Report Adventure Cum Cultural Guide Course W.E.F 01 Oct 2009 to 15 Oct 2009
COURSE REPORT ADVENTURE CUM CULTURAL GUIDE COURSE W.E.F 01 OCT 2009 TO 15 OCT 2009 GENERAL COURSE REPORT ADVENTURE COURSE CONDUCTED AT, LEH (LADAKH) INSTITUTE: JAWAHAR INSTITUTE OF MOUNTAINEERING & WINTER SPORTS (JIM & WS) PAHALGAM VENUE: LEH, LADAKH REPORT ON: ADVENTURE CUM CULTURAL GUIDE COURSE COURSE SERIAL NO: ADVENTURE CUM CULTURAL GUIDE COURSE- 58 DURATION OF COURSE: 01 Oct 2009 to 15 Oct 2009 (15 DAYS) INTRODUCTION 1. Jawahar Institute of Mountaineering & Winter Sports, (JIM & WS) conducted one Adventure Cum Cultural Guide Course for 40 students of Ladakh region w.e.f 01 Oct 09 to 15 Oct 09 sponsored by Ministry of Tourism, Govt of India, New Delhi. The Course was inaugurated by Lt. Col Virnider Singh, Principal, JIM & WS on 01 Oct 2009. The list of students is attached at Appendix “P”. OPENING ADDRESS BY LT. COL VIRINDER SINGH, PRINCIPAL, JIM & WS 2 AIM 2. To expose the youth to nature, kindling the spirit of adventure, development of personality, character, courage and confidence through adventure activities and sports as well as to boost adventure tourism in J & K State (Leh, Ladakh). STANDARD TO BE ACHIEVED 3. The competence levels expected from students upon completion of the camps are as follows:- (a) Empowered & well development adolescents. (b) National Integrity. (c) Adventurous attitude. (d) High Standard of youth activities & techniques. OBJECTIVES 4. (a) Promotion adventure activities in the state. (b) Impart training on technical aspects of Mountaineering. (c) Hone Mountaineering skills of individuals. (d) Create environment awareness amongst youth. (e) Character building. (f) To train the locals as cultural guide to tourists. -
H E M I S - T S O K a R , Par Le K H a R N a K
Treks avec assistance - 323 H E M I S - T S O K A R , par le K H A R N A K C'est un très beau trek pour les amateurs de solitude et d'espaces vierges. Mis à part le départ et l'arrivée, on voit rarement quelqu'un sur ce parcours. La rencontre imprévisible des nomades et de leurs troupeaux de chèvres et de yaks est un grand moment. Aucun permis n'est nécessaire, et tôt ou tard il faudra payer le droit de place de 100 Rs2011 par jour, soit au moine de Dat, soit aux nomades. période : de juin à septembre, possible en octobre avec des nuits froides et quelques centimètres de neige. durée : 8-9 jours. On peut gagner un jour en faisant Dat-Pangchen dans la journée. D'autre part, le hasard de la rencontre des nomades mérite de passer une journée sur place. équipement : chaussures étanches et bon duvet. agence : indispensable, ne serait-ce que pour porter la nourriture, et appréciable pour le portage du matériel de camping et de cuisine. à voir : tout. L'agence qui organise le trek s'occupe du pré-acheminement en taxi jusqu'à Shang Sumdo près d'Hemis. En fonction du temps disponible, on peut profiter de la journée pour visiter quelques monastères en cours de route : Matho, Stakna et/ou Hemis par exemple, avant de passer la nuit à Shang Sumdo. Sinon, on peut rejoindre l'équipe au petit matin, directement depuis Leh et commencer l'ascension du Konmaru La immédiatement. Mais attention, de ce côté le col est très difficile, et il est plus facile de partir de Chiling et remonter la Markha Valley. -

Last Post Indian War Memorials Around the World
Last Post Indian War Memorials Around the World Introduction • 1 Rana Chhina Last Post Indian War Memorials Around the World i Capt Suresh Sharma Last Post Indian War Memorials Around the World Rana T.S. Chhina Centre for Armed Forces Historical Research United Service Institution of India 2014 First published 2014 © United Service Institution of India All rights reserved. No part of this publication may be reproduced or transmitted, in any form or by any means, without prior permission of the author / publisher. ISBN 978-81-902097-9-3 Centre for Armed Forces Historical Research United Service Institution of India Rao Tula Ram Marg, Post Bag No. 8, Vasant Vihar PO New Delhi 110057, India. email: [email protected] www.usiofindia.org Printed by Aegean Offset Printers, Gr. Noida, India. Capt Suresh Sharma Contents Foreword ix Introduction 1 Section I The Two World Wars 15 Memorials around the World 47 Section II The Wars since Independence 129 Memorials in India 161 Acknowledgements 206 Appendix A Indian War Dead WW-I & II: Details by CWGC Memorial 208 Appendix B CWGC Commitment Summary by Country 230 The Gift of India Is there ought you need that my hands hold? Rich gifts of raiment or grain or gold? Lo! I have flung to the East and the West Priceless treasures torn from my breast, and yielded the sons of my stricken womb to the drum-beats of duty, the sabers of doom. Gathered like pearls in their alien graves Silent they sleep by the Persian waves, scattered like shells on Egyptian sands, they lie with pale brows and brave, broken hands, strewn like blossoms mowed down by chance on the blood-brown meadows of Flanders and France. -

ERONET Pre Reqst Format.Xlsx
Polling Station wise list of Booth Level Officers (BLO) 26-Constituency of LAHDC, Leh-Ladakh No. of P/S Name of Polling station Name of Booth Level Officer Mobile . No 1 01- Thang Sh Sana Ullah 9419864100 2 02 -Tyakshi Sh Mohs Ayoub 9469552752 3 03Waha Pachathang Sh Abdul Rashid 9419534709 4 04 -Turtuk farool Sh Abdul Hamid 9469277933 5 05 -Turtuk youl Sh Ghulam Mohd 9469462863 6 06 -Garari Sh Mohd Omar 9469265938 7 07 -Chulungkha Sh Mohd Ibrahim 9419388079 8 08 -Bogdang Sh Qurban Ali 9419829393 9 09 -Skilkhor Sh. Shamsher Ali 9419971169 10 10-Changmar Sh Mohd Ali Khan 9469265209 11 11- Waris Sh. Ghulam Mohd 9469515130 12 12 -Fastan Sh Ghulam Mohd 9469531252 13 13- Sunudo Sh. Thoskor Spalgyas 9469176699 14 14 -Largyap Gogma Sh. Ali Akbar 9419440193 15 15 -Largyap Yokma Sh Ibrahim Ali 9469732596 16 16 –Pachathang Sh Mohd Hassan 9419386471 17 17 -Terchay Sh Sonam Nurboo 9419880947 18 18 –Skuru Sh Abdul Rashid 9419515915 19 19 -Rakuru Sh Mohd Mussa 9469212778 20 20 -Udmaroo Sh. Tashi Dawa 9419440625 21 21 -Shukur Sh Tsering Dorjey 9469178364 22 22 -Hundri Sh. Stanzin Dorjay 9469617039 23 23 -Hunder Sh Tashi Wangdus 9419550812 24 24-Awaksha Ms. Shakila Bano 9419448032 25 25 -Hunder Dok Ms. Naheda Akhatar 9469572613 26 26 -Skampuk Sh Tsetan Dorjey 9469362975 27 27 -Partapur Sh. Rehbar Hussain 9469571886 28 28 –Diskit-A Sh Rinchen Dorjey 9469165230 29 29-Diskit-B Sh Stanzin Galik 9469292903 30 30 -Burma Sh Stanzin Wangchok 9469213895 31 31 -Charasa Sh Deldan Namgail 9469387070 32 32 –Kuri Mr Punchok Angchok 9419974947 33 33- Murgi Sh. -

Ground Water Scenario of Himalaya Region, India
Hkkjr ds fgeky;h {ks=k dk Hkwty ifjn`'; Ground Water Scenario of Himalayan Region, India laiknu@Edited By: lq'khy xqIrk v/;{k Sushil Gupta Chairman Central Ground Water Board dsanzh; Hkwfe tycksMZ Ministry of Water Resources ty lalk/ku ea=kky; Government of India Hkkjr ljdkj 2014 Hkkjr ds fgeky;h {ks=k dk Hkwty ifjn`'; vuqØef.kdk dk;Zdkjh lkjka'k i`"B 1- ifjp; 1 2- ty ekSle foKku 23 3- Hkw&vkd`fr foKku 34 4- ty foKku vkSj lrgh ty mi;kst~;rk 50 5- HkwfoKku vkSj foorZfudh 58 6- Hkwty foKku 73 7- ty jlk;u foKku 116 8- Hkwty lalk/ku laHkko~;rk 152 9- Hkkjr ds fgeky;h {ks=k esa Hkwty fodkl ds laca/k esa vfHktkr fo"k; vkSj leL;k,a 161 10- Hkkjr ds fgeky;h {ks=k ds Hkwty fodkl gsrq dk;Zuhfr 164 lanHkZ lwph 179 Ground Water Scenario of Himalayan Region of India CONTENTS Executive Summary i Pages 1. Introduction 1 2. Hydrometeorology 23 3. Geomorphology 34 4. Hydrology and Surface Water Utilisation 50 5. Geology and Tectonics 58 6. Hydrogeology 73 7. Hydrochemistry 116 8. Ground Water Resource Potential 152 9. Issues and problems identified in respect of Ground Water Development 161 in Himalayan Region of India 10. Strategies and plan for Ground Water Development in Himalayan Region of India 164 Bibliography 179 ifêdkvks dh lwph I. iz'kklfud ekufp=k II. Hkw vkd`fr ekufp=k III. HkwoSKkfud ekufp=k d- fgeky; ds mRrjh vkSj if'peh [kaM [k- fgeky; ds iwohZ vkSj mRrj iwohZ [kaM rFkk iwoksZRrj jkT; IV. -
Village Code
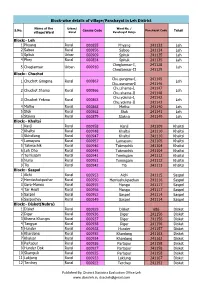
Block-wise details of village/Panchayat in Leh District Name of the Urban/ Ward No. / S.No. Census Code Panchayat Code Tehsil village/Ward Rural Panchayat Halqa Block:- Leh 1 Phyang Rural 000855 Phyang 241133 Leh 2 Saboo Rural 000856 Saboo 241134 Leh 3 Spituk Urban 000909 Spituk 241135 Leh 4 Phey Rural 000854 Spituk 241135 Leh Choglamsar-I, 241128 5 Choglamsar Urban 000910 Leh Choglamsar-II 241129 Block:- Chuchot Chu.gongma-I, 241145 1 Chuchot Gongma Rural 000867 Leh Chu.gongma-II 241146 Chu.shama-I, 241147 2 Chuchot Shama Rural 000866 Leh Chu.shama-II 241148 Chu.yokma-I, 241142 3 Chuchot Yokma Rural 000863 Leh Chu.yokma-II 241143 4 Matho Rural 000868 Matho 241140 Leh 5 Stok Rural 000862 Stok 241141 Leh 6 Stakna Rural 000879 Stakna 241149 Leh Block:- Khaltsi 1 Kanji Rural 000958 Kanji 241109 Khaltsi 2 Khaltsi Rural 000948 Khaltsi 241110 Khaltsi 3 Skindiang Rural 000947 Khaltsi 241110 Khaltsi 4 Lamayuru Rural 000957 Lamayuru 241105 Khaltsi 5 Takmachik Rural 000946 Takmachik 241104 Khaltsi 6 Leh Dho Rural 000945 Takmachik 241104 Khaltsi 7 Temisgam Rural 000941 Temisgam 241112 Khaltsi 8 Nurla Rural 000951 Temisgam 241112 Khaltsi 9 Tia Rural 000942 Tia 241113 Khaltsi Block:- Saspol 1 Alchi Rural 000953 Alchi 241115 Saspol 2 Hemisshukpachan Rural 000950 Hemisshukpachan 241116 Saspol 3 Gera-Mangu Rural 000955 Mangu 241117 Saspol 4 Tar Hepti Rural 000956 Mangu 241117 Saspol 5 Saspol Rural 000952 Saspol 241114 Saspol 6 Saspochey Rural 000949 Saspol 241114 Saspol Block:- Disket(Nubra) 1 Disket Rural 000929 Disket 686 Disket 2 Diger Rural 000936 -

03 Economic Review 2015-16
0 1 DISTRICT PROFILE Although, Leh district is one of the largest districts of the country in terms of area, it has the lowest population density across the entire country. The district borders Pakistan occupied Kashmir and Chinese occupied Ladakh in the North and Northwest respectively, Tibet in the east and Lahoul-Spiti area of Himachal Pradesh in the South. The district of Leh forms the Northern tip of the Indian Sub Continent. According to the Geographical experts, the district has several other features, which make it unique when compared with other parts of the Indian sub-continent. The district is the coldest and most elevated inhabited region in the country with altitude ranging from 2300 meters to 5000 meters. As a result of its high altitude locations, annual rainfall is extremely low. This low status of precipitation has resulted in scanty vegetation, low organic content in the soil and loose structure in the cold desert. But large-scale plantation has been going in the district since 1955 and this state of affairs is likely to change. The ancient inhabitants of Ladakh were Dards, an Indo- Aryan race. Immigrants of Tibet, Skardo and nearby parts like Purang, Guge settled in Ladakh, whose racial characters and cultures were in consonance with early settlers. Buddhism traveled from central India to Tibet via Ladakh leaving its imprint in Ladakh. Islamic missionaries also made a peaceful penetration of Islam in the early 16 th century. German Moravian Missionaries having cognizance of East India Company also made inroads towards conversion but with little success. In the 10 th century AD, Skit Lde Nemagon, the ruler of Tibet, invaded Ladakh where there was no central authority. -

Census of India 1981
CENSUS OF INDIA 1981 SERIES-8 JAMMU & KASHMIR Special Paper of 1981 VILLAGE / TOWN WISE POPULATION AND SCHEDULED CASTE POPULATION ABDUL GANI Joint Dil ector of Census Operations Jammu and Kashmir PREFACE This is a special publication presenting the 1981 Census total popu lation and scheduled caste population of the State, districts and Tehsils down to village/urban block level to meet the requirement of data users interested in figures of population at village/ward level. This requirement could have been served by the 1981 District Census Handbooks which contain comprehensive basic information about populatIon by sex including literacy and work partici pation but the printing and publication of these handbooks which is the respon sibility of the State government will take some time. Until these handbooks are published, it is hoped that the present volume will serve a useful purpose to feed the urgent requirement of all data users. The Director of Census Opserations Shri A. H. Khan, under whose guidance the entire census operations were carried out, deserve all cred it for the success of the operations but he had to leave the organisation because of superannuation before this paper could be made ready for the press. I must record my deepest sense of gratitude to Shri V.S. Verma, Registrar General, India and Shri V.P. Pandey, Joint Registrar General, IndIa for their valuable guidance and for having agreed to bring out this specIal paper even in deviation of the approved census publications programme and arrange for its printing on a priority basis through the Printing Divi~ion of the Registrar General's Office under the supervision of Shri Tirath Dass, Joint Director.