Narcolepsy and Other Disorders of Excessive Sleepiness
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Case of Recurrent Sleep Paralysis: Beyond Narcolepsy
Open Access Austin Journal of Clinical Neurology A Austin Full Text Article Publishing Group Case Report A Case of Recurrent Sleep Paralysis: Beyond Narcolepsy Vijaya Yelisetty and Kanika Bagai* Abstract Department of Neurology, Vanderbilt University School of Medicine, Tennessee, USA Isolated episodes of sleep paralysis can occur in healthy people at least *Corresponding author: Kanika Bagai, Department of once in their lifetime; however recurrent isolated sleep paralysis (RISP) events Neurology, Vanderbilt Sleep Disorders Center, Vanderbilt are less common and often worrisome. Recurrent episodes of sleep paralysis University School of Medicine, A- 0118 Medical Center are often seen in patients with narcolepsy. Here, we present a unique case of North, Nashville, TN 37232, Tennessee, USA, Tel: 615- a middle-aged woman who presents with symptoms of RISP in her fifth decade 322-0283; Fax: 615-936-0223; Email: kanika.bagai@ that was not associated with narcolepsy. Vanderbilt.Edu Received: June 20, 2014; Accepted: August 20, 2014; Published: August 22, 2014 Introduction Laboratory data including complete blood count, complete metabolic panel, TSH, Vit B12, Vit D levels were within normal limits We describe a case of a 52-year-old woman who presents with as below: initial symptoms of recurrent isolated sleep paralysis. Complete blood count: WBC: 5.7k/ul; Hemoglobin 12.6 gm/dl, Case Presentation hematocrit 37%, platelets count 258k/ul. A 52 year-old woman presented to the sleep clinic with complaints Chemistries: Sodium 141 mmol/l, potassium 4.1 mmol/l, chloride of sleep difficulties and symptoms of “unable to move her body while 107 mmol/l, bicarbonate 25 mmol/l, glucose 213 mg/dl, BUN 19 mg/ in bed”. -

Sleep Disorders Preeti Devnani
SPECIAL ISSUE 1: INVITED ARTICLE Sleep Disorders Preeti Devnani ABSTRACT Sleep disorders are an increasingly important and relevant burden faced by society, impacting at the individual, community and global level. Varied presentations and lack of awareness can make accurate and timely diagnosis a challenge. Early recognition and appropriate intervention are a priority. The key characteristics, clinical presentations and management strategies of common sleep disorders such as circadian rhythm disorders, restless legs syndrome, REM behavior disorder, hypersomnia and insomnia are outlined in this review. Keywords: Hypersomnia, Insomnia, REM behavior International Journal of Head and Neck Surgery (2019): 10.5005/jp-journals-10001-1362 INTRODUCTION Department of Neurology and Sleep Disorder, Cleveland Clinic, Abu Sleep disorders are becoming increasingly common in this modern Dhabi, United Arab Emirates era, resulting from several lifestyle changes. These complaints may Corresponding Author: Preeti Devnani, Department of Neurology present excessive daytime sleepiness, lack of sleep or impaired and Sleep Disorder, Cleveland Clinic, Abu Dhabi, United Arab Emirates, quality, sleep related breathing disorders, circadian rhythm disorder e-mail: [email protected] misalignment and abnormal sleep-related movement disorders.1 How to cite this article: Devnani P. Sleep Disorders. Int J Head Neck They are associated with impaired daytime functioning, Surg 2019;10(1):4–8. increased risk of cardiovascular and cerebrovascular disease, poor Source of support: Nil glycemic control, risk of cognitive decline and impaired immunity Conflict of interest: None impacting overall morbidity and mortality. Diagnosis of sleep disorders is clinical in many scenarios, The following circadian rhythm sleep–wake disorders adapted polysomnography is a gold standard for further evaluation of from the ICSD-3: intrinsic sleep disorder such as obstructive sleep apnea (OSA) • Delayed sleep–wake phase disorder and periodic limb movement disorder (PLMD). -

Sleep Disturbances in Patients with Persistent Delusions: Prevalence, Clinical Associations, and Therapeutic Strategies
Review Sleep Disturbances in Patients with Persistent Delusions: Prevalence, Clinical Associations, and Therapeutic Strategies Alexandre González-Rodríguez 1 , Javier Labad 2 and Mary V. Seeman 3,* 1 Department of Mental Health, Parc Tauli University Hospital, Autonomous University of Barcelona (UAB), I3PT, Sabadell, 08280 Barcelona, Spain; [email protected] 2 Department of Psychiatry, Hospital of Mataró, Consorci Sanitari del Maresme, Institut d’Investigació i Innovació Parc Tauli (I3PT), CIBERSAM, Mataró, 08304 Barcelona, Spain; [email protected] 3 Department of Psychiatry, University of Toronto, #605 260 Heath St. West, Toronto, ON M5T 1R8, Canada * Correspondence: [email protected] Received: 1 September 2020; Accepted: 12 October 2020; Published: 16 October 2020 Abstract: Sleep disturbances accompany almost all mental illnesses, either because sound sleep and mental well-being share similar requisites, or because mental problems lead to sleep problems, or vice versa. The aim of this narrative review was to examine sleep in patients with delusions, particularly in those diagnosed with delusional disorder. We did this in sequence, first for psychiatric illness in general, then for psychotic illnesses where delusions are prevalent symptoms, and then for delusional disorder. The review also looked at the effect on sleep parameters of individual symptoms commonly seen in delusional disorder (paranoia, cognitive distortions, suicidal thoughts) and searched the evidence base for indications of antipsychotic drug effects on sleep. It subsequently evaluated the influence of sleep therapies on psychotic symptoms, particularly delusions. The review’s findings are clinically important. Delusional symptoms and sleep quality influence one another reciprocally. Effective treatment of sleep problems is of potential benefit to patients with persistent delusions, but may be difficult to implement in the absence of an established therapeutic relationship and an appropriate pharmacologic regimen. -

RBD, Sexsomnia, Sleepwalking, and Sleep Paralysis Comorbidities: Relevance to Pulmonary, Dental, and Behavioral Sleep Medicine
87 EDITORIALRBD, sexsomnia, sleepwalking, and sleep paralysis comorbidities: relevance to pulmonary, dental, and behavioral sleep medicine RBD, sexsomnia, sleepwalking, and sleep paralysis comorbidities: relevance to pulmonary, dental, and behavioral sleep medicine Carlos H. Schenck INTRODUCTION This issue of Sleep Science contains three reports1-3 on diverse REM and NREM parasomnias that serve as illuminating entry points to a broad range of comorbidities that are interlinked with the parasomnias, with relevance to multiple sleep medicine subspecialties. Minnesota Regional Sleep Disorders Center, Departments of Psychiatry, Hennepin Besides the fascinating mechanistic questions raised by this interlinking, there are also County Medical Center and University of important clinical management issues that need to be considered. Parasomnias, to a surprising Minnesota Medical School, Minneapolis, extent, are situated at the core of sleep medicine. The International Classification of Sleep USA Disorders, 3rd Edition (ICSD-3)4 recognizes that instinctual behaviors can be pathologically released with the parasomnias, involving locomotion (sleepwalking), aggression (RBD and NREM parasomnias), eating (sleep related eating disorder), and sex (sexsomnia) that carry the potential for adverse physical, psychological, and interpersonal consequences. Central pattern generators (CPGs) in the brainstem, subserving primitive behaviors, are inappropriately activated with the parasomnias. Figure 1 provides a useful and scientifically sound framework for understanding parasomnia behavioral release and their triggers, based on the seminal work of Tassinari et al. (2005)5 and Tassinari et al. (2009)6 from Bologna related to CPGs, parasomnias, and nocturnal seizures. In regards to the NREM parasomnias, the factors that predispose, prime and precipitate these parasomnias have been comprehensively reviewed by Pressman (2007)7. -

Isolated Sleep Paralysis in a Case of Panic Disorder Avinash De Sousa
IJPP Avinash De Sousa 10.5005/jp-journals-10067-0009 CASE REPORT Isolated Sleep Paralysis in a Case of Panic Disorder Avinash De Sousa ABSTRACT CASE REPORT We present herewith a case of isolated sleep paralysis (ISP) A 33-year-old married man working as a teacher pre- which entails a transient, generalized inability to move or speak, sented to the psychiatry outpatient department with chief i.e., usually seen during the patient’s transitions between sleep complaints of episodes of inability to move his limbs at and wakefulness. We report the case of a 33-year-old man with recurrent ISP and panic disorder. The patient sought help after night while asleep since the past 6 years. The patient nearly 6 years of symptoms as he thought that the symptoms had all these episodes during his sleep at night and the were part of his nocturnal panic attacks. Isolated sleep paralysis event lasted 15 to 20 minutes whereby he was unable to is seen in conjunction with multiple anxiety disorders and the move his limbs or turn in bed or even call for help, all of symptoms may mimic anxiety, thereby confounding the diagno- which he would desperately want to do each time but sis. It is prudent that clinicians keep in mind sleep paralysis as a differential diagnosis in anxiety disorders as all cases of freezing was unable to do so. He had panic disorder for many at night may not be nocturnal panic attacks. years and was on treatment. He thought that these epi- sodes were nocturnal panic attacks. -

Sleep Paralysis: Phenomenology, Neurophysiology and Treatment
Sleep Paralysis: phenomenology, neurophysiology and treatment Elizaveta Solomonova1,2 1Université de Montréal, Individualized program (Cognitive Neuroscience & Philosophy). 2Center for Advanced Research in Sleep Medicine, Dream and Nightmare Laboratory, Montreal, Canada To appear in: The Oxford Handbook of Spontaneous Thought: Mind-Wandering, Creativity, Dreaming, and Clinical Conditions. Fox, K & Christoff, K. Eds. Abstract Sleep paralysis is an experience of being temporarily unable to move or talk during the transitional periods between sleep and wakefulness: at sleep onset or upon awakening. Feeling of paralysis may be accompanied by a variety of vivid and intense sensory experiences, including mentation in visual, auditory, and tactile modalities, as well as a distinct feeling of presence. This chapter discusses a variety of sleep paralysis experiences from the perspective of enactive cognition and cultural neurophenomenology. Current knowledge of neurophysiology and associated conditions is presented, and some techniques for coping with sleep paralysis are proposed. As an experience characterized by a hybrid state of dreaming and waking, sleep paralysis offers a unique window into phenomenology of spontaneous thought in sleep. Introduction “I had a few terrifying experiences a few years ago. I awoke in the middle of the night. I was sleeping on my back, and couldn't move, but I had the sensation I could see around my room. There was a terrifying figure looming over me. Almost pressing on me. The best way I could describe it was that it was made of shadows. A deep rumbling or buzzing sound was present. It felt like I was in the presence of evil... Which sounds so strange to say!” (31 year old man, USA) Sleep paralysis (SP) is a transient and generally benign phenomenon occurring at sleep onset or upon awakening. -

The Co-Occurrence of Sexsomnia, Sleep Bruxism and Other Sleep Disorders
Journal of Clinical Medicine Review The Co-Occurrence of Sexsomnia, Sleep Bruxism and Other Sleep Disorders Helena Martynowicz 1, Joanna Smardz 2, Tomasz Wieczorek 3, Grzegorz Mazur 1, Rafal Poreba 1, Robert Skomro 4, Marek Zietek 5, Anna Wojakowska 1, Monika Michalek 1 ID and Mieszko Wieckiewicz 2,* 1 Department of Internal Medicine, Occupational Diseases and Hypertension, Wroclaw Medical University, 50-367 Wroclaw, Poland; [email protected] (H.M.); [email protected] (G.M.); [email protected] (R.P.); [email protected] (A.W.); [email protected] (M.M.) 2 Department of Experimental Dentistry, Wroclaw Medical University, 50-367 Wroclaw, Poland; [email protected] 3 Department and Clinic of Psychiatry, Wroclaw Medical University, 50-367 Wroclaw, Poland; [email protected] 4 Division of Respiratory Critical Care and Sleep Medicine, Department of Medicine, University of Saskatchewan, Saskatoon, SK S7N 5A2, Canada; [email protected] 5 Department of Periodontology, Wroclaw Medical University, 50-367 Wroclaw, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-660-47-87-59 Received: 3 August 2018; Accepted: 19 August 2018; Published: 23 August 2018 Abstract: Background: Sleep sex also known as sexsomnia or somnambulistic sexual behavior is proposed to be classified as NREM (non-rapid eye movement) parasomnia (as a clinical subtype of disorders of arousal from NREM sleep—primarily confusional arousals or less commonly sleepwalking), but it has also been described in relation to REM (rapid eye movement) parasomnias. Methods: The authors searched the PubMed database to identify relevant publications and present the co-occurrence of sexsomnia and other sleep disorders as a non-systematic review with case series. -

A Comparison of Idiopathic Hypersomnia and Narcolepsy-Cataplexy Using Self Report Measures and Sleep Diary Data
57676ournal ofNeurology, Neurosurgery, and Psychiatry 1996;60:576-578 SHORT REPORT J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.60.5.576 on 1 May 1996. Downloaded from A comparison of idiopathic hypersomnia and narcolepsy-cataplexy using self report measures and sleep diary data Dorothy Bruck, J D Parkes Abstract Published data comparing patients with IH Eighteen patients with idiopathic hyper- and patients with NLS outside the sleep labo- somnia (IH) were compared with 50 ratory are scarce. Using self report question- patients with the narcoleptic syndrome of naires and sleep diary data our aim was to cataplexy and daytime sleepiness (NLS) determine the extent of group differences and using self report questionnaires and a which variables best discriminated between IH diary of sleep/wake patterns. The IH and NLS. group reported more consolidated noc- turnal sleep, a lower propensity to nap, greater refreshment after naps, and a Patients and methods greater improvement in excessive day- DIAGNOSTIC CRITERIA time sleepiness since onset than the NLS Idiopathic hypersomnia group. In IH, the onset of excessive day- Patients were selected with a complaint of time sleepiness was predominantly asso- excessive daytime sleepiness without cataplexy ciated with familial inheritance or a viral and with no evidence of any medical, psycho- illness. Two variables-number of logical, drug related, or respiratory disorder. reported awakenings during nocturnal All patients met diagnostic criteria ascertained sleep and the reported change in sleepi- from questionnaire responses: Epworth sleepi- ness since onset-provided maximum ness scale score8 > 13; duration of excessive discrimination between the IH and NLS daytime sleepiness > five years, profile of groups. -

NAMS Regional Symposium on Sleep Medicine CAUSES of HYPERSOMNIA – NARCOLEPSY
NAMS Regional Symposium on Sleep Medicine Speaker : Dr. M.V. Padma Srivastava CAUSES OF HYPERSOMNIA – NARCOLEPSY SYNOPSIS Volitional sleep deprivation and obstructive sleep apnea are the most common causes of hypersomnia. The remaining causes are primarily due to primary central nervous system abnormalities, the most common of which is narcolepsy, a primary disorder of the neural control of wakefulness and sleep. Narcolepsy is the prototypic example of dissociated sleep-wake phenomenon in which components of one state (REM) appear in another ( wakefulness). Narcolepsy is a relatively frequent disorder with a prevalence of 0.09%. A clear genetic component is indicated by the fact that over 90% of individuals with narcolepsy carry the HLA DR15 and HLA DQ6 gene, which is found in less than 30% of the general population. Siblings of individuals with narcolepsy have a 60-fold increased likelihood for developing the disease. Narcolepsy is thought to result also from abnormal neurotransmitter functioning and sensitivity and abnormal immune modulation. Clinical manifestations of normal sleep include (i) Excessive Daytime Somnolence (EDS); (ii) Cataplexy; ( iii) Hypnogogic hallucinations; and (iv) Sleep paralysis. Whenever possible, the diagnosis of narcolepsy should be confirmed by polysomnography (PSG) followed by a multiple sleep latency test (MSLT). Cataplexy: Cataplexy, which occurs in 65% to 70% of the patients of narcolepsy, comprises of sudden loss of muscle tone, typically triggered by emotion such as laughter, anger, excitement, delight or surprise. The muscle weakness of cataplexy may be complete, resulting in the patients falling or being forced to sit; much more commonly, the weakness is milder and more focal, taking the form of facial sagging, slurred speech or localized weakness of an extremity. -
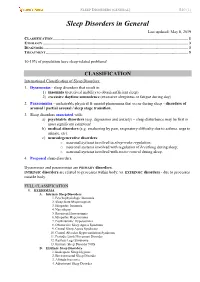
Sleep Disorders in General Last Updated: May 8, 2019 CLASSIFICATION
SLEEP DISORDERS (GENERAL) S40 (1) Sleep Disorders in General Last updated: May 8, 2019 CLASSIFICATION ...................................................................................................................................... 1 ETIOLOGY ................................................................................................................................................ 3 DIAGNOSIS................................................................................................................................................ 3 TREATMENT ............................................................................................................................................. 5 10-15% of population have sleep-related problems! CLASSIFICATION International Classification of Sleep Disorders: 1. Dyssomnias - sleep disorders that result in: 1) insomnia (perceived inability to obtain sufficient sleep) 2) excessive daytime somnolence (excessive sleepiness or fatigue during day) 2. Parasomnias - undesirable physical & mental phenomena that occur during sleep - disorders of arousal / partial arousal / sleep stage transition. 3. Sleep disorders associated with: a) psychiatric disorders (esp. depression and anxiety) – sleep disturbance may be first or most significant symptom! b) medical disorders (e.g. awakening by pain, respiratory difficulty due to asthma, urge to urinate, etc). c) neurodegenerative disorders: o neuronal systems involved in sleep-wake regulation; o neuronal systems involved with regulation of breathing during -

Depression: Relationships to Sleep Paralysis and Other Sleep Disturbances in a Community Sample Mariana Szklo-Coxe Old Dominion University, [email protected]
Old Dominion University ODU Digital Commons Community & Environmental Health Faculty Community & Environmental Health Publications 2007 Depression: Relationships to Sleep Paralysis and Other Sleep Disturbances in a Community Sample Mariana Szklo-Coxe Old Dominion University, [email protected] Terry Young Laurel Finn Emmanuel Mignot Follow this and additional works at: https://digitalcommons.odu.edu/commhealth_fac_pubs Part of the Medical Physiology Commons, Mental and Social Health Commons, and the Sleep Medicine Commons Repository Citation Szklo-Coxe, Mariana; Young, Terry; Finn, Laurel; and Mignot, Emmanuel, "Depression: Relationships to Sleep Paralysis and Other Sleep Disturbances in a Community Sample" (2007). Community & Environmental Health Faculty Publications. 70. https://digitalcommons.odu.edu/commhealth_fac_pubs/70 Original Publication Citation Szklo-Coxe, M., Young, T., Finn, L., & Mignot, E. (2007). Depression: relationships to sleep paralysis and other sleep disturbances in a community sample. Journal of Sleep Research, 16(3), 297-312. doi:10.1111/j.1365-2869.2007.00600.x This Article is brought to you for free and open access by the Community & Environmental Health at ODU Digital Commons. It has been accepted for inclusion in Community & Environmental Health Faculty Publications by an authorized administrator of ODU Digital Commons. For more information, please contact [email protected]. J. Sleep Res. (2007) 16, 297–312 Depression: relationships to sleep paralysis and other sleep disturbances in a community sample MARIANA SZKLO-COXE1 , TERRY YOUNG1 , LAUREL FINN1 and EMMANUEL MIGNOT2 1Department of Population Health Sciences, University of Wisconsin School of Medicine and Public Health, Madison, WI, USA and 2Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine, Palo Alto, CA, USA Accepted in revised form 11 June 2007; received 8 February, 2006 SUMMARY Sleep disturbances are important correlates of depression, with epidemiologic research heretofore focused on insomnia and sleepiness. -

PE1281 Narcolepsy
Narcolepsy Narcolepsy appears to be a disorder of the part of the central nervous system that controls sleep and wakefulness. What is Narcolepsy is a chronic (lifelong) disorder that affects the brain and is narcolepsy? characterized by a permanent and overwhelming feeling of sleepiness. Narcolepsy affects many children, and most cases go undiagnosed and untreated. Although it is a relatively uncommon condition, its impact on a child’s life can be dramatic. It affects children of all genders equally, and symptoms usually develop after puberty, with most people reporting the first symptoms of narcolepsy between the ages of 15 and 30. What are the The symptoms of narcolepsy can appear all at once or they can develop symptoms of slowly over many years. The four most common symptoms are: narcolepsy? • Excessive daytime sleepiness. It is usually the first symptom of narcolepsy, Children with narcolepsy often report feeling tired all the time. They tend to fall asleep not only in situations in which many normal people feel sleepy (after meals or during a dull lecture), but also when most people would remain awake (while talking to someone or writing a letter). Individuals with narcolepsy may also fall asleep at dangerous times (like when driving a car). • Cataplexy. Cataplexy is the sudden, brief loss of muscle control triggered by a strong emotion, such as laughter, anger, or surprise. In children, cataplexy can also occur spontaneously. Cataplexy can range from subtle weakness in the face or slurred speech, to complete collapse. Cataplexy is sometimes the first symptom of narcolepsy but can also develop several years after daytime sleepiness.