Qualified Life Event (Qle) Divorce, Legal Separation, Annulment Process
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Legal Separation
Indiana Legal Services, Inc www.indianalegalservices.org Legal Separation I am thinking about divorcing my spouse, but am not sure if I should. Is there anything else I can do? Yes. You can file a legal separation from your spouse. You can do this when you don’t want a divorce, but you cannot currently live with your spouse. What is the difference between divorce and legal separation? Divorce is when a judge legally ends your marriage. Legal separation doesn’t end the marriage. The court can, however, issue orders like the ones issued in a divorce case concerning property, debts, and children. A legal separation is like a “temporary divorce.” How long does a legal separation last? A legal separation can last up to one year. After one year you should be ready to decide if you want to get a divorce or get back together with your spouse. If either spouse files for a divorce during the legal separation period, then the divorce case will take over and the legal separation will end. All orders of a legal separation end when the legal separation ends. What do I have to do to get legally separated from my spouse? You need to file a Petition for Legal Separation. In your petition you will need to tell the judge the reasons why you think you and your spouse cannot currently live together. Either you or your spouse must be a resident of Indiana, and a resident of the County where you file, for six months before you file the petition. -

Separation and Divorce Information
Separation and Divorce Information Separation and Divorce Definitions The Legal Process of Separation and Divorce Divorce Mediation Child Support The Emotional Process of Divorce Selecting and Working with Professionals Children and Divorce Taking Care of Yourself During Separation and Divorce The Fairfax County Commission for Women 12000 Government Center Parkway Suite 339 Fairfax, VA 22035 703-324-5730; 711 TTY © 1991; Revised: June 1997, July 2004, August 2010 TABLE OF CONTENTS Introduction......................................................................................... 1 Separation and Divorce Definitions .................................................... 3 The Legal Process of Separation and Divorce................................... 7 Divorce Mediation............................................................................... 9 Child Support.................................................................................... 11 The Emotional Process of Divorce ................................................... 14 Selecting and Working With Professionals....................................... 16 Children and Divorce........................................................................ 19 Taking Care of Yourself During Separation and Divorce.................. 21 Attorney and Legal Service Referrals............................................... 24 Other Resources .............................................................................. 25 Introduction The Fairfax County Commission for Women developed this information -

Divorce & Legal Separation
Divorce & Legal Separation From annulments to divorce, we are well-versed in all areas regarding divorce and legal separation. Working with the business, tax, litigation, securities, and estate planning practice groups, we handle both simple and complex domestic matters. Areas of practice within this arena include: Child Custody & Visitation Rights We work with clients to ensure the best interests of all children are met. Through interviews and court appearances, we make certain no stone is left unturned in these emotional matters. Child Support We believe it is important for our clients who have children under 18 years of age to receive the proper amount of child support entitled by law. Working with both parties, we are able to negotiate fair child support payments for their clients. Division of Assets & Liabilities We make every effort to ensure that clients' separate assets are identified and protected. In this arena, we offer clients the expertise of attorneys from multiple practice areas to address business and tax concerns which so often accompany marital dissolution. Spousal Support & Alimony We realize spousal support and alimony can be a great discourse among couples who are separated or divorced. We work to obtain the most full and fair amount of spousal support and alimony available. In the News OKC Family Law Attorney Gile Family Featured in Journal Record - Family law, all in the family Nicole Longwell joins Hall Estill as Special Counsel, Bryan Lynch and Natalie Sears join as Associates Hall Estill Divorce Attorney Rick Wagner - Change in tax law hastens divorce settlements www.hallestill.com Awards & Recognition 11 Hall Estill Attorneys named 2022 Best Lawyers in America® “Lawyers of the Year” www.hallestill.com. -

Effects of the 2010 Civil Code on Trends in Joint Physical Custody in Catalonia
EFFECTS OF THE 2010 CIVIL CODE ON TRENDS IN JOINT PHYSICAL CUSTODY IN CATALONIA. A COMPARISON WITH THE Document downloaded from www.cairn-int.info - Universitat Autònoma de Barcelona 158.109.138.45 09/05/2017 14h03. © I.N.E.D REST OF SPAIN Montserrat Solsona, Jeroen Spijker I.N.E.D | « Population » 2016/2 Vol. 71 | pages 297 - 323 ISSN 0032-4663 ISBN 9782733210666 This document is a translation of: -------------------------------------------------------------------------------------------------------------------- Montserrat Solsona, Jeroen Spijker, « Influence du Code civil catalan (2010) sur les décisions de garde partagée. Comparaisons entre la Catalogne et le reste de Espagne », Population 2016/2 (Vol. 71), p. 297-323. -------------------------------------------------------------------------------------------------------------------- Available online at : -------------------------------------------------------------------------------------------------------------------- http://www.cairn-int.info/article-E_POPU_1602_0313--effects-of-the-2010-civil-code- on.htm -------------------------------------------------------------------------------------------------------------------- How to cite this article : -------------------------------------------------------------------------------------------------------------------- Montserrat Solsona, Jeroen Spijker, « Influence du Code civil catalan (2010) sur les décisions de garde partagée. Comparaisons entre la Catalogne et le reste de Espagne », Population 2016/2 (Vol. 71), p. 297-323. -------------------------------------------------------------------------------------------------------------------- -

Debunking Texas' Family Law Myths
Debunking Texas’ Family Law Myths 1. You can only get a divorce in Texas if you were married parties is community property until the spouse claiming in Texas. FALSE. Texas courts have jurisdiction over a the funds as his or her separate property proves the divorce action if either spouse resided in Texas for a funds are separate in nature by clear and convincing continuous six-month period prior to the filing of the evidence. If separate property funds are commingled divorce petition. with community property funds, it is the separate property owner’s burden to trace the funds to show the 2. In custody actions, the law favors mothers. FALSE. Texas original source and the current value of the separate law expressly provides that a family court shall not property funds. consider a parent’s gender in making decisions regarding custody. Judges must determine what is in the best 6. Parties are required to have a hearing if a petition is filed. interest of the child, taking all facts and circumstances TRUE and FALSE. If the parties reach an agreement on of the child and the parties into consideration. Judges all issues in a divorce case, one party must attend an presume that both parents should be named joint uncontested hearing to testify about the elements of the managing conservators with relatively equal rights and agreement and request that the agreement be signed and duties. The parent who has historically been the primary made into an order. In non-divorce cases, agreements caregiver of the child is usually granted the exclusive can be submitted to the court for signature by filing and right to designate the primary residence of the child. -

Separation, Adultery, Children Born out of Wedlock
COI QUERY Country of Origin Philippines Main subject Separation, adultery, children born out of wedlock Question(s) 1) Legal framework of divorce in the Philippines, and its implementation/enforcement in practice; 2) Legal framework of adultery in the Philippines, and its implementation/enforcement in practice; 3) Societal consequences of adultery; 4) Separation Agreements in the Philippines and their legal effects; 5) Legal status of children born out of the wedlock and/or as result of adultery; 6) Societal attitude towards a child born out of wedlock and/or as result of adultery Date of completion 6 March 2020 Query Code Q5-2020 Contributing EU+ COI n/a units (if applicable) Disclaimer This response to a COI query has been elaborated according to the Common EU Guidelines for Processing COI and EASO COI Report Methodology. The information provided in this response has been researched, evaluated and processed with utmost care within a limited time frame. All sources used are referenced. A quality review has been performed in line with the above mentioned methodology. This document does not claim to be exhaustive neither conclusive as to the merit of any particular claim to international protection. If a certain event, person or organisation is not mentioned in the report, this does not mean that the event has not taken place or that the person or organisation does not exist. Terminology used should not be regarded as indicative of a particular legal position. The information in the response does not necessarily reflect the opinion of EASO and makes no political statement whatsoever. The target audience is caseworkers, COI researchers, policy makers, and decision making authorities. -

COURT of the DISTRICT of COLUMBIA FAMILY COURT Domestic Relations Branch
COURT OF THE DISTRICT OF COLUMBIA FAMILY COURT Domestic Relations Branch _ _______________________________________ PRINT YOUR SPOUSE’S NAME _ _______________________________________ S TREET ADDRESS _ _______________________________________ C ITY, STATE AND ZIP CODE DR _____________________ PLAINTIFF , v. Related Cases: ________________________________________ P RINT YOUR NAME _____________________________ ________________________________________ _____________________________ S TREET ADDRESS ________________________________________ C ITY, STATE AND ZIP CODE SUBSTITUTE ADDRESS: CHECK BOX IF YOU HAVE WRITTEN SOMEONE ELSE’S ADDRESS BECAUSE YOU FEAR HARASSMENT OR HARM. DEFENDANT. CONTESTED ANSWER TO COMPLAINT FOR LEGAL SEPARATION AND COUNTERCLAIM I, _______________________________, am the Defendant in this case. PRINT YOUR NAME 1. With regard to this Court’s authority to decide my spouse’s request for legal separation and related issues, I answer and state that [CHECK ONE] F I agree with my spouse’s statement that this Court has the authority to decide my spouse’s request for legal separation and related issues. F I disagree with my spouse’s statement that this Court has the authority to decide my spouse’s request for legal separation and related issues. DC Bar Pro Bono Program (revised 9-2011) Complaint for Legal Separation (Contested Answer and Counterclaim) Page 1 of 8 2. With regard to my marriage to my spouse, I answer and state that [CHECK ONE] F I agree with my spouse’s statement about how, when and where we were married. F I disagree with my spouse’s statement about how, when and where we were married. 3. With regard to my separation from my spouse, I answer and state that [CHECK ONE] F I agree with my spouse’s statement about when we separated. -
How to Ask for a Legal Separation for Parties That Agree
FLIC 1.4 How to Ask for a Legal Separation For spouses/registered domestic partners who agree Use this packet only if: • You and your spouse or registered domestic partner agree on the terms of your legal separation, and • Your spouse or registered domestic partner will sign the court papers to show that s/he agrees. WARNINGS! • If one of you is pregnant, or a child was born before the legal separation, the other spouse is considered the legal parent. If you do not think the other spouse/registered domestic partner is the parent, you may need to file a parentage case before you finalize the case. If you are in this situation, talk to a lawyer. • Due to COVID-19, all hearings are being done by phone or video and most offices are only providing remote services. You should consult the King County Superior Court webpage for the most up to date information. https://www.kingcounty.gov/courts/superior-court.aspx. Talk to a lawyer, if you can These instructions have been developed by the King County Superior Court Family Law Information Center. They are not intended to be a substitute for legal advice. They provide only legal information. It’s a good idea to talk to a lawyer before you file any forms. If you cannot afford a lawyer, you can: • You can obtain a list of low-cost and free legal resources. https://kingcounty.gov/~/media/courts/superior- court/docs/family/facilitator/family-law-resources.ashx?la=en • Get help from the Family Law Facilitators office. You can get information about their services at https://kingcounty.gov/courts/superior-court/family/facilitator.aspx. -

Domestic Partnership Edition
Family Law Handbook Understanding the Legal Implications of Domestic Partnerships and Dissolution in Washington State JULY 2019 Dear Reader, Our Washington State law requires that the Administrative Office of the Courts provide the attached family law handbook to individuals entering into a domestic partnership, those seeking to terminate their domestic partnership and those responding to a dissolution action. If you are receiving this book after entering into a domestic partnership, we would like to offer our sincere congratulations. Our supportive relationships can enrich our lives and help bring out the best parts, and best versions, of ourselves. This is truly something to celebrate. If you are receiving this handbook during a more trying time, when your relationship is ending, this can certainly be an incredibly painful and stressful experience. This handbook can provide answers to some of the basic questions you may have regarding the law and the court processes you may encounter. It is our hope that even during these very challenging transitions, families are able to strive toward civility and show one another mutual respect. This may mean keeping an open mind, disagreeing respectfully, and seeking mutual ground if and when it is possible and appropriate. For families with children, modeling respect, reflection, and self-awareness can help ease them into new transitions. Parental conflict is deeply troubling to children. How a child adapts to separation can be very dependent upon the response of their parents. If your partnership is ending due to violence or assault, we encourage you to read through this handbook for information and resources to help you safely navigate your next steps and to identify the ways in which the court system may be able to assist you. -

How to Begin Your Action for Dissolution, Legal Separation, Or Nullity
HOW TO BEGIN YOUR ACTION FOR DISSOLUTION, LEGAL SEPARATION, OR NULLITY 1. COMPLETE THE FORMS (Type or print in black ink) Summons Petition (with Declaration under the UCCJEA if minor children) 2. MAKE COPIES You will need to make two additional copies of each form, front and back. 3. FILE THE PAPERS Take the originals and two copies to the Family Law Filing Window, in Ventura, Room 208. You will have to pay a filing fee. The Fee Schedule may be obtained from the Clerk. If you cannot afford the fee, you may be able to have that fee “waived”. You will need to complete the FEE WAIVER PACKET. The clerk will keep the originals and return both copies to you, stamped to show that they have been “filed”. One copy is for you and one copy is to be “served” on the other party, your spouse. 4. “SERVE” THE PAPERS “Service” means that someone other than you, over the age of 18, must personally deliver a copy of the filed papers to the other party. The other party also gets a package of blank forms so that they can file their Response. Those blank forms are at the back of the Forms packet. If you wish you can arrange for the Sheriff to serve your spouse. If the other party is out of state or if you don’t know their whereabouts, you may want to speak to the Family Law Facilitator about other ways to serve the papers. 5. FILE THE PROOF OF SERVICE The person who “serves” the papers must complete and sign the “Proof of Service”. -
How to Ask for a Legal Separation There ARE Dependent Children of This Marriage the Parties ARE Signing the Papers Together the Parties ARE in Agreement
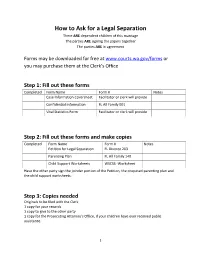
How to Ask for a Legal Separation There ARE dependent children of this marriage The parties ARE signing the papers together The parties ARE in agreement Forms may be downloaded for free at www.courts.wa.gov/forms or you may purchase them at the Clerk’s Office Step 1: Fill out these forms Completed Form Name Form # Notes Case Information Coversheet Facilitator or clerk will provide Confidential Information FL All Family 001 Vital Statistics Form Facilitator or clerk will provide Step 2: Fill out these forms and make copies Completed Form Name Form # Notes Petition for Legal Separation FL Divorce 203 Parenting Plan FL All Family 140 Child Support Worksheets WSCSS -Worksheet Have the other party sign the joinder portion of the Petition, the proposed parenting plan and the child support worksheets. Step 3: Copies needed Originals to be filed with the Clerk 1 copy for your records 1 copy to give to the other party 1 copy for the Prosecuting Attorney’s Office, if your children have ever received public assistance. 1 Step 4: File your originals with the Clerk’s office and pay the filing fee If you cannot afford to pay the fee, Fill out these forms Completed Form Name Form # Notes Motion and Declaration for Waiver of Civil WPF GR Fees and Surcharges 34.0100 Financial Statement (each party must fill one WPF GR Each Party must fill out if joinder signed) 34.0300 one out Order re Waiver of Civil Fees and Surcharges WPF GR 34.0500 The forms are also available for download at www.courts.wa.gov/forms. -

REGISTERED DOMESTIC PARTNERSHIPS (RDP) *Serve This Form on the Other Party in Contested Cases for Clerk Only – Do Not Serve
DOCUMENT CHART: DISSOLUTION/LEGAL SE PARATION/INVALIDITY OF REGISTERED DOMESTIC PARTNERSHIPS (RDP) *Serve this form on the other party in contested cases For Clerk only – do not serve Agreed Contested Document or Form With No With No Form Name Number Children Children Children Children Confidential Information Form FL All Family 001 P P P P Case Information Cover Sheet Cover Sheet P P P P Certificate of Dissolution Health form P P P P Summons: Notice about a Marriage or FL Divorce 200 Domestic Partnership P* P* Petition (choose only one:) to end RDP (Dissolution) FL Divorce 203 for Legal Separation (RDP), OR FL Divorce 204 P P P* P* to Invalidate (Annul) RDP FL Divorce 206 Parenting Plan (Proposed) FL All Family 140 P* Child Support Worksheets (Proposed) WSCSS Schedule and (or see Facilitator or use on-line calculator) WSCSS Worksheets P* Kitsap County Local Form: Note for Motion Docket Exhibit E P P Proof of Personal Service FL All Family 101 P P Declaration: Personal Service Could Not be Made in Washington FL All Family 102 P P (if applicable) FINAL DOCUMENTS Parenting Plan FL All Family 140 P P Residential Time Summary Report FL Divorce 243 P P Child Support Worksheets WSCSS Schedule and (or see Facilitator or use on-line calculator) WSCSS Worksheets P P Order of Child Support FL All Family 130 P P Findings and Conclusions about a FL Divorce 232 Registered Domestic Partnership P P P P Final Order Ending RDP/ Legal Separation Order/ FL Divorce 242 P P P P Invalid RDP Order F:\COMMON\Facilitator, General\Charts and Checklists\Document