Maternal and Child Health in Jimma Zone, Ethiopia: Predictors, Barriers and Strategies for Improvement
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
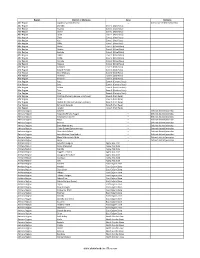
Districts of Ethiopia
Region District or Woredas Zone Remarks Afar Region Argobba Special Woreda -- Independent district/woredas Afar Region Afambo Zone 1 (Awsi Rasu) Afar Region Asayita Zone 1 (Awsi Rasu) Afar Region Chifra Zone 1 (Awsi Rasu) Afar Region Dubti Zone 1 (Awsi Rasu) Afar Region Elidar Zone 1 (Awsi Rasu) Afar Region Kori Zone 1 (Awsi Rasu) Afar Region Mille Zone 1 (Awsi Rasu) Afar Region Abala Zone 2 (Kilbet Rasu) Afar Region Afdera Zone 2 (Kilbet Rasu) Afar Region Berhale Zone 2 (Kilbet Rasu) Afar Region Dallol Zone 2 (Kilbet Rasu) Afar Region Erebti Zone 2 (Kilbet Rasu) Afar Region Koneba Zone 2 (Kilbet Rasu) Afar Region Megale Zone 2 (Kilbet Rasu) Afar Region Amibara Zone 3 (Gabi Rasu) Afar Region Awash Fentale Zone 3 (Gabi Rasu) Afar Region Bure Mudaytu Zone 3 (Gabi Rasu) Afar Region Dulecha Zone 3 (Gabi Rasu) Afar Region Gewane Zone 3 (Gabi Rasu) Afar Region Aura Zone 4 (Fantena Rasu) Afar Region Ewa Zone 4 (Fantena Rasu) Afar Region Gulina Zone 4 (Fantena Rasu) Afar Region Teru Zone 4 (Fantena Rasu) Afar Region Yalo Zone 4 (Fantena Rasu) Afar Region Dalifage (formerly known as Artuma) Zone 5 (Hari Rasu) Afar Region Dewe Zone 5 (Hari Rasu) Afar Region Hadele Ele (formerly known as Fursi) Zone 5 (Hari Rasu) Afar Region Simurobi Gele'alo Zone 5 (Hari Rasu) Afar Region Telalak Zone 5 (Hari Rasu) Amhara Region Achefer -- Defunct district/woredas Amhara Region Angolalla Terana Asagirt -- Defunct district/woredas Amhara Region Artuma Fursina Jile -- Defunct district/woredas Amhara Region Banja -- Defunct district/woredas Amhara Region Belessa -- -

Midterm Survey Protocol
Protocol for L10K Midterm Survey The Last 10 Kilometers Project JSI Research & Training Institute, Inc. Addis Ababa, Ethiopia October 2010 Contents Introduction ........................................................................................................................................................ 2 The Last Ten Kilometers Project ............................................................................................................ 3 Objective one activities cover all the L10K woredas: .......................................................................... 4 Activities for objectives two, three and four in selected woredas ...................................................... 5 The purpose of the midterm survey ....................................................................................................... 6 The midterm survey design ...................................................................................................................... 7 Annex 1: List of L10K woredas by region, implementation strategy, and implementing phase ......... 10 Annex 2: Maps.................................................................................................................................................. 11 Annex 3: Research questions with their corresponding study design ...................................................... 14 Annex 4: Baseline survey methodology ........................................................................................................ 15 Annex 5: L10K midterm survey -

Aethiopica 19 (2016) International Journal of Ethiopian and Eritrean Studies
Aethiopica 19 (2016) International Journal of Ethiopian and Eritrean Studies ________________________________________________________________ MINAKO ISHIHARA, Nanzan University Article Change in the Significance of Affiliation to Ṭarīqa The Case of Tiǧāniyya in and around Ǧimma Aethiopica 19 (2016), 149–164 ISSN: 2194–4024 ________________________________________________________________ Edited in the Asien-Afrika-Institut Hiob Ludolf Zentrum für Äthiopistik der Universität Hamburg Abteilung für Afrikanistik und Äthiopistik by Alessandro Bausi in cooperation with Bairu Tafla, Ulrich Braukämper, Ludwig Gerhardt, Hilke Meyer-Bahlburg and Siegbert Uhlig Editorial The present issue of AETHIOPICA, like the preceding one, is partly monograph- ic, with a section containing the proceedings of the Panel on Islamic Literature in Ethiopia: New Perspectives of Research, from the ‘19th International Con- ference of Ethiopian Studies’, held in Warsaw, Poland, on 24–28 August 2015. Starting from this issue, the annual bibliography on Ethiopian Semitic and Cushitic linguistics held from its inception in 1998 for eighteen years by Rainer Voigt is handed over, on Voigt’s own will, to a pool of younger scholars, with the substantial support of the AETHIOPICA editorial team. I would like on this occasion to express the deep gratitude of the editorial board of AETHIOPICA and of all scholars in Ethiopian Semitic and Cushitic linguistics to Rainer Voigt for his fundamental and valuable contribution. Bibliographical abbreviations used in this volume AÉ Annales d’Éthiopie, Paris 1955ff. ÄthFor Äthiopistische Forschungen, 1–35, ed. by E. HAMMERSCHMIDT, 36–40, ed. by S. UHLIG (Stuttgart: Franz Steiner (1–34), 1977–1992; Wiesbaden: Harrassowitz (35–40), 1994–1995). AethFor Aethiopistische Forschungen, 41–73, ed. by S. -

Historical Survey of Limmu Genet Town from Its Foundation up to Present
INTERNATIONAL JOURNAL OF SCIENTIFIC & TECHNOLOGY RESEARCH VOLUME 6, ISSUE 07, JULY 2017 ISSN 2277-8616 Historical Survey Of Limmu Genet Town From Its Foundation Up To Present Dagm Alemayehu Tegegn Abstract: The process of modern urbanization in Ethiopia began to take shape since the later part of the nineteenth century. The territorial expansion of emperor Menelik (r. 1889 –1913), political stability and effective centralization and bureaucratization of government brought relative acceleration of the pace of urbanization in Ethiopia; the improvement of the system of transportation and communication are identified as factors that contributed to this new phase of urban development. Central government expansion to the south led to the appearance of garrison centers which gradually developed to small- sized urban center or Katama. The garrison were established either on already existing settlements or on fresh sites and also physically they were situated on hill tops. Consequently, Limmu Genet town was founded on the former Limmu Ennarya state‘s territory as a result of the territorial expansion of the central government and system of administration. Although the history of the town and its people trace many year back to the present, no historical study has been conducted on. Therefore the aim of this study is to explore the history of Limmu Genet town from its foundation up to present. Keywords: Limmu Ennary, Limmu Genet, Urbanization, Development ———————————————————— 1. Historical Background of the Study Area its production. The production and marketing of forest coffee spread the fame and prestige of Limmu Enarya ( The early history of Limmu Oromo Mohammeed Hassen, 1994). The name Limmu Ennarya is The history of Limmu Genet can be traced back to the rise derived from a combination of the name of the medieval of the Limmu Oromo clans, which became kingdoms or state of Ennarya and the Oromo clan name who settled in states along the Gibe river basin. -

(Coffea Arabica L.) Accessions Collected from Limmu Coffee
American Journal of BioScience 2021; 9(3): 79-85 http://www.sciencepublishinggroup.com/j/ajbio doi: 10.11648/j.ajbio.20210903.12 ISSN: 2330-0159 (Print); ISSN: 2330-0167 (Online) Phenotypic Diversity of Ethiopian Coffee ( Coffea arabica L.) Accessions Collected from Limmu Coffee Growing Areas Using Multivariate Analysis Lemi Beksisa *, Tadesse Benti, Getachew Weldemichael Ethiopian Institute of Agricultural Research, Jimma Agricultural Research Center, Jimma, Ethiopia Email address: *Corresponding author To cite this article: Lemi Beksisa, Tadesse Benti, Getachew Weldemichael. Phenotypic Diversity of Ethiopian Coffee ( Coffea arabica L.) Accessions Collected from Limmu Coffee Growing Areas Using Multivariate Analysis. American Journal of BioScience . Vol. 9, No. 3, 2021, pp. 79-85. doi: 10.11648/j.ajbio.20210903.12 Received : April 17, 2021; Accepted : May 11, 2021; Published : May 20, 2021 Abstract: Forty seven Coffea arabica L. germplasm accessions collected from Limmu district were field evaluated from 2004/5 to 2013/14 with two commercial check varieties at Agaro Agricultural Research sub center in single plot. The objective of the experiment was to assess the variability among the accessions using quantitative traits. Data for about eight quantitative traits were recorded only once in experimental period, while the yield data were recorded for six consecutive cropping seasons. Cluster, genetic divergence, and principal component analysis were used to assess the variability among the genotypes. The results revealed that average linkage cluster analysis for nine traits grouped the germplasm accessions in to three clusters. The number of accessions per cluster ranged from three in cluster III to 25 in cluster II. The clustering pattern of the coffee accessions revealed that the prevalence of moderate genetic diversity in Limmu coffee for the characters studied. -

Ethiopia Round 6 SDP Questionnaire
Ethiopia Round 6 SDP Questionnaire Always 001a. Your name: [NAME] Is this your name? ◯ Yes ◯ No 001b. Enter your name below. 001a = 0 Please record your name 002a = 0 Day: 002b. Record the correct date and time. Month: Year: ◯ TIGRAY ◯ AFAR ◯ AMHARA ◯ OROMIYA ◯ SOMALIE BENISHANGUL GUMZ 003a. Region ◯ ◯ S.N.N.P ◯ GAMBELA ◯ HARARI ◯ ADDIS ABABA ◯ DIRE DAWA filter_list=${this_country} ◯ NORTH WEST TIGRAY ◯ CENTRAL TIGRAY ◯ EASTERN TIGRAY ◯ SOUTHERN TIGRAY ◯ WESTERN TIGRAY ◯ MEKELE TOWN SPECIAL ◯ ZONE 1 ◯ ZONE 2 ◯ ZONE 3 ZONE 5 003b. Zone ◯ ◯ NORTH GONDAR ◯ SOUTH GONDAR ◯ NORTH WELLO ◯ SOUTH WELLO ◯ NORTH SHEWA ◯ EAST GOJAM ◯ WEST GOJAM ◯ WAG HIMRA ◯ AWI ◯ OROMIYA 1 ◯ BAHIR DAR SPECIAL ◯ WEST WELLEGA ◯ EAST WELLEGA ◯ ILU ABA BORA ◯ JIMMA ◯ WEST SHEWA ◯ NORTH SHEWA ◯ EAST SHEWA ◯ ARSI ◯ WEST HARARGE ◯ EAST HARARGE ◯ BALE ◯ SOUTH WEST SHEWA ◯ GUJI ◯ ADAMA SPECIAL ◯ WEST ARSI ◯ KELEM WELLEGA ◯ HORO GUDRU WELLEGA ◯ Shinile ◯ Jijiga ◯ Liben ◯ METEKEL ◯ ASOSA ◯ PAWE SPECIAL ◯ GURAGE ◯ HADIYA ◯ KEMBATA TIBARO ◯ SIDAMA ◯ GEDEO ◯ WOLAYITA ◯ SOUTH OMO ◯ SHEKA ◯ KEFA ◯ GAMO GOFA ◯ BENCH MAJI ◯ AMARO SPECIAL ◯ DAWURO ◯ SILTIE ◯ ALABA SPECIAL ◯ HAWASSA CITY ADMINISTRATION ◯ AGNEWAK ◯ MEJENGER ◯ HARARI ◯ AKAKI KALITY ◯ NEFAS SILK-LAFTO ◯ KOLFE KERANIYO 2 ◯ GULELE ◯ LIDETA ◯ KIRKOS-SUB CITY ◯ ARADA ◯ ADDIS KETEMA ◯ YEKA ◯ BOLE ◯ DIRE DAWA filter_list=${level1} ◯ TAHTAY ADIYABO ◯ MEDEBAY ZANA ◯ TSELEMTI ◯ SHIRE ENIDASILASE/TOWN/ ◯ AHIFEROM ◯ ADWA ◯ TAHTAY MAYCHEW ◯ NADER ADET ◯ DEGUA TEMBEN ◯ ABIYI ADI/TOWN/ ◯ ADWA/TOWN/ ◯ AXUM/TOWN/ ◯ SAESI TSADAMBA ◯ KLITE -

Administrative Region, Zone and Woreda Map of Oromia a M Tigray a Afar M H U Amhara a Uz N M
35°0'0"E 40°0'0"E Administrative Region, Zone and Woreda Map of Oromia A m Tigray A Afar m h u Amhara a uz N m Dera u N u u G " / m r B u l t Dire Dawa " r a e 0 g G n Hareri 0 ' r u u Addis Ababa ' n i H a 0 Gambela m s Somali 0 ° b a K Oromia Ü a I ° o A Hidabu 0 u Wara o r a n SNNPR 0 h a b s o a 1 u r Abote r z 1 d Jarte a Jarso a b s a b i m J i i L i b K Jardega e r L S u G i g n o G A a e m e r b r a u / K e t m uyu D b e n i u l u o Abay B M G i Ginde e a r n L e o e D l o Chomen e M K Beret a a Abe r s Chinaksen B H e t h Yaya Abichuna Gne'a r a c Nejo Dongoro t u Kombolcha a o Gulele R W Gudetu Kondole b Jimma Genete ru J u Adda a a Boji Dirmeji a d o Jida Goro Gutu i Jarso t Gu J o Kembibit b a g B d e Berga l Kersa Bila Seyo e i l t S d D e a i l u u r b Gursum G i e M Haro Maya B b u B o Boji Chekorsa a l d Lalo Asabi g Jimma Rare Mida M Aleltu a D G e e i o u e u Kurfa Chele t r i r Mieso m s Kegn r Gobu Seyo Ifata A f o F a S Ayira Guliso e Tulo b u S e G j a e i S n Gawo Kebe h i a r a Bako F o d G a l e i r y E l i Ambo i Chiro Zuria r Wayu e e e i l d Gaji Tibe d lm a a s Diga e Toke n Jimma Horo Zuria s e Dale Wabera n a w Tuka B Haru h e N Gimbichu t Kutaye e Yubdo W B Chwaka C a Goba Koricha a Leka a Gidami Boneya Boshe D M A Dale Sadi l Gemechis J I e Sayo Nole Dulecha lu k Nole Kaba i Tikur Alem o l D Lalo Kile Wama Hagalo o b r Yama Logi Welel Akaki a a a Enchini i Dawo ' b Meko n Gena e U Anchar a Midega Tola h a G Dabo a t t M Babile o Jimma Nunu c W e H l d m i K S i s a Kersana o f Hana Arjo D n Becho A o t -

Ethiopia: Governing the Faithful
Ethiopia: Governing the Faithful Crisis Group Africa Briefing N°117 Nairobi/Brussels, 22 February 2016 I. Overview Ethiopia provides a significant example of the struggle governments are undertaking to find and implement effective policy responses to faith-based violent extremism and sectarian conflict. Given both demographic shifts and greater religious freedoms, the management of religious conflict and practice has of necessity been a complex and sometimes fraught task. A changed context has seen the Ethiopian People’s Revolu- tionary Democratic Front (EPRDF) government shift from mediating conflict between faith groups to regulating religious practice, especially where there are political or extremist overtones. Local actors have used the state’s interventionist inclinations in the confessional realm to gain advantage in wider leadership struggles within Ethio- pia’s ethnically based regional states. Opposition groups, not always within formal par- ties, have also used religious issues to score political points. The Ethiopian experience shows not only how faith is an increasing political resource, especially at local levels, but also lessons that can be learned from top-down interventions in the religious sphere. Although often regarded as a predominantly Christian country, the confessional landscape is diverse and evolving, and religion is increasingly politicised by a range of domestic actors, including the state. Faith runs deep, and its religions (particularly the Orthodox Church) have at various times in history been intimately connected to the Ethiopian state and its administration. Always a significant but institutionally dis- advantaged minority, the Muslim population has grown in relative terms in recent decades and is at least as numerous as that in Sudan, Ethiopia’s predominantly Islamic neighbour. -

Ethiopia: Administrative Map (August 2017)
Ethiopia: Administrative map (August 2017) ERITREA National capital P Erob Tahtay Adiyabo Regional capital Gulomekeda Laelay Adiyabo Mereb Leke Ahferom Red Sea Humera Adigrat ! ! Dalul ! Adwa Ganta Afeshum Aksum Saesie Tsaedaemba Shire Indasilase ! Zonal Capital ! North West TigrayTahtay KoraroTahtay Maychew Eastern Tigray Kafta Humera Laelay Maychew Werei Leke TIGRAY Asgede Tsimbila Central Tigray Hawzen Medebay Zana Koneba Naeder Adet Berahile Region boundary Atsbi Wenberta Western Tigray Kelete Awelallo Welkait Kola Temben Tselemti Degua Temben Mekele Zone boundary Tanqua Abergele P Zone 2 (Kilbet Rasu) Tsegede Tselemt Mekele Town Special Enderta Afdera Addi Arekay South East Ab Ala Tsegede Mirab Armacho Beyeda Woreda boundary Debark Erebti SUDAN Hintalo Wejirat Saharti Samre Tach Armacho Abergele Sanja ! Dabat Janamora Megale Bidu Alaje Sahla Addis Ababa Ziquala Maychew ! Wegera Metema Lay Armacho Wag Himra Endamehoni Raya Azebo North Gondar Gonder ! Sekota Teru Afar Chilga Southern Tigray Gonder City Adm. Yalo East Belesa Ofla West Belesa Kurri Dehana Dembia Gonder Zuria Alamata Gaz Gibla Zone 4 (Fantana Rasu ) Elidar Amhara Gelegu Quara ! Takusa Ebenat Gulina Bugna Awra Libo Kemkem Kobo Gidan Lasta Benishangul Gumuz North Wello AFAR Alfa Zone 1(Awsi Rasu) Debre Tabor Ewa ! Fogera Farta Lay Gayint Semera Meket Guba Lafto DPubti DJIBOUTI Jawi South Gondar Dire Dawa Semen Achefer East Esite Chifra Bahir Dar Wadla Delanta Habru Asayita P Tach Gayint ! Bahir Dar City Adm. Aysaita Guba AMHARA Dera Ambasel Debub Achefer Bahirdar Zuria Dawunt Worebabu Gambela Dangura West Esite Gulf of Aden Mecha Adaa'r Mile Pawe Special Simada Thehulederie Kutaber Dangila Yilmana Densa Afambo Mekdela Tenta Awi Dessie Bati Hulet Ej Enese ! Hareri Sayint Dessie City Adm. -

Kerchanshe Trading Plc Addis Ababa,St Gabriel Church Bayne Building, Addis Ababa/ N/S/ Lafto, Ethiopia
SCS Global Services does hereby certify that an independent assessment has been conducted of: Kerchanshe Trading Plc Addis Ababa,St Gabriel church Bayne Building, Addis Ababa/ N/S/ Lafto, Ethiopia Scope of Certificate: Organic Coffee Arabica Washed and Organic Coffee Arabica Natural (organic green coffee) At the following sites: See Annex The facilities are hereby certified to sell products as: Fair Trade Certified The assessment has been conducted by SCS Global Services (SCS) in accordance with the standards and compliance criteria listed below: Fair Trade USA Agricultural Production Standard - Version 1.1.0 Fair Trade USA ID#: 1661106 Valid from 21 July 2020 to 20 July 2023 Jim Knutzon, Vice President SCS Global Services 2000 Powell Street, Ste. 600, Emeryville, CA 94608 USA This is an addendum to certificate #1661106 and must be accompanied by this certificate to be considered valid. This addendum is not a certificate and is not valid as a stand-alone document. Kerchanshe Trading Plc Addis Ababa,St Gabriel church Bayne Building, Addis Ababa/ N/S/ Lafto, Ethiopia Fair Trade USA ID #: 1661106 . Name Address Product Form Beshasha Limmu wet and dry mill Oromia Region, Jimma Zone, Organic Coffee Arabica Washed and Organic Coffee Arabica Gomma Woreda, Bashasha, Natural (organic green coffee) Ethiopia Kochere wet and dry mill SNNPRS, Gedio Zone, Kochore Organic Coffee Arabica Washed and Organic Coffee Arabica Woreda , Kochore, Ethiopia Natural (organic green coffee) Guji Adola wet and dry mill Oromia, Region, Guji Zone, Organic Coffee Arabica -

Knowledge, Attitudes and Practices Towards Rabies in Dedo District of Jimma Zone, Southwestern Ethiopia: a Community Based Cross-Sectional Study
Vol. 9(5), pp. 61-71, May 2017 DOI: 10.5897/IJMMS2017.1302 Article Number: 2DCB3CC64168 International Journal of Medicine ISSN 2006-9723 Copyright © 2017 and Medical Sciences Author(s) retain the copyright of this article http://www.academicjournals.org/IJMMS Full Length Research Paper Knowledge, attitudes and practices towards rabies in Dedo district of Jimma zone, southwestern Ethiopia: A community based cross-sectional study Nejash Abdela1*, Boru Midekso1, Jemal Jabir1 and Wezir Abdela2 1School of Veterinary Medicine, College of Agriculture and Veterinary Medicine, Jimma University, P. O. Box. 307, Jimma, Ethiopia. 2School of Public Health, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia. Received 20 March, 2017: Accepted 19 April, 2017 Rabies is a fatal neglected viral zoonosis which causes encephalitis in many warm-blooded animals and humans. It is an incurable disease once the clinical signs appear. However, it can be prevented via vaccination and community awareness. This study was therefore designed to determine the level of community knowledge, attitude and practices (KAP) regarding rabies. Cross sectional study was conducted from December 2016 to January 2017 in Dedo district, Jimma zone, southwestern Ethiopia. Multistage sampling technique was employed for selection of sample unit and data were collected from 135 household by face-to-face interview using a semi structured and validated questionnaire. Logistic regression was used for assessing the association of independent variable with KAP score. Out of 135 participants interviewed, 71.1% were urban and 57% were male respondents. All (100%) participants had heard about rabies and 88.9% were aware that rabies is zoonotic. -

Medicinal Plants Use and Conservation Practices in Jimma Zone, South West Ethiopia
Vol. 7(3), pp. 202-210, March, 2015 DOI: 10.5897/IJBC2015.0822 Article Number: 65A316D51947 International Journal of Biodiversity ISSN 2141-243X Copyright © 2015 and Conservation Author(s) retain the copyright of this article http://www.academicjournals.org/IJBC Full Length Research Paper Medicinal plants use and conservation practices in Jimma Zone, South West Ethiopia Debela Hunde Feyssa, Chemeda Abdeta, Techale Berhan* and Manju Sharma College of Agriculture & Veterinary Medicine, Jimma University, Ethiopia. Received 2 February, 2015; Accepted 16 March, 2015 Traditional medicine has continued to be the most affordable and easily accessible source of treatment in the primary healthcare system of Ethiopia. However, the medicinal plants used for such treatments are becoming increasingly rare and vulnerable to extinction because of improper utilization and conservation practices. Hence, this paper was initiated with the aim to assess the use, management and conservation practices of medicinal plants in some selected districts of Jimma Zone, south west Ethiopia. Ethnobotanical methods such as focus group discussions, key informant interview, semistructured interview and field walks were used to collect ethnobotanical data on use and management practices of medicinal plants in the study area. Data collected were classified into the use of the plants and management practice. Data of the semistructured interview was analyzed using SPSS version 16 software. The result revealed that a total of 69 plant species were identified in the study area, of which 30 are nutraceuticals, 30 are collected at wild habitat and 39 are cultivated. Source of medicinal plants include: cultivation in home gardens, live fences, crop fields and wild collection from the nearby environment.