Pericarditis – Clinical Features and Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Guidelines on the Diagnosis and Management of Pericardial
European Heart Journal (2004) Ã, 1–28 ESC Guidelines Guidelines on the Diagnosis and Management of Pericardial Diseases Full Text The Task Force on the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology Task Force members, Bernhard Maisch, Chairperson* (Germany), Petar M. Seferovic (Serbia and Montenegro), Arsen D. Ristic (Serbia and Montenegro), Raimund Erbel (Germany), Reiner Rienmuller€ (Austria), Yehuda Adler (Israel), Witold Z. Tomkowski (Poland), Gaetano Thiene (Italy), Magdi H. Yacoub (UK) ESC Committee for Practice Guidelines (CPG), Silvia G. Priori (Chairperson) (Italy), Maria Angeles Alonso Garcia (Spain), Jean-Jacques Blanc (France), Andrzej Budaj (Poland), Martin Cowie (UK), Veronica Dean (France), Jaap Deckers (The Netherlands), Enrique Fernandez Burgos (Spain), John Lekakis (Greece), Bertil Lindahl (Sweden), Gianfranco Mazzotta (Italy), Joa~o Morais (Portugal), Ali Oto (Turkey), Otto A. Smiseth (Norway) Document Reviewers, Gianfranco Mazzotta, CPG Review Coordinator (Italy), Jean Acar (France), Eloisa Arbustini (Italy), Anton E. Becker (The Netherlands), Giacomo Chiaranda (Italy), Yonathan Hasin (Israel), Rolf Jenni (Switzerland), Werner Klein (Austria), Irene Lang (Austria), Thomas F. Luscher€ (Switzerland), Fausto J. Pinto (Portugal), Ralph Shabetai (USA), Maarten L. Simoons (The Netherlands), Jordi Soler Soler (Spain), David H. Spodick (USA) Table of contents Constrictive pericarditis . 9 Pericardial cysts . 13 Preamble . 2 Specific forms of pericarditis . 13 Introduction. 2 Viral pericarditis . 13 Aetiology and classification of pericardial disease. 2 Bacterial pericarditis . 14 Pericardial syndromes . ..................... 2 Tuberculous pericarditis . 14 Congenital defects of the pericardium . 2 Pericarditis in renal failure . 16 Acute pericarditis . 2 Autoreactive pericarditis and pericardial Chronic pericarditis . 6 involvement in systemic autoimmune Recurrent pericarditis . 6 diseases . 16 Pericardial effusion and cardiac tamponade . -
General Physical Examination Skills for Ahps
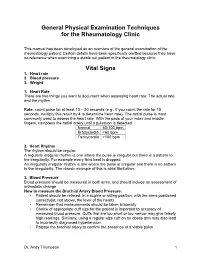
General Physical Examination Techniques for the Rheumatology Clinic This manual has been developed as an overview of the general examination of the rheumatology patient. Certain details have been specifically omitted because they have no relevance when examining a stable out patient in the rheumatology clinic. Vital Signs 1. Heart rate 2. Blood pressure 3. Weight 1. Heart Rate There are two things you want to document when assessing heart rate: The actual rate and the rhythm. Rate: count pulse for at least 15 – 30 seconds (e.g., if you count the rate for 15 seconds, multiply this result by 4 to determine heart rate). The radial pulse is most commonly used to assess the heart rate. With the pads of your index and middle fingers, compress the radial artery until a pulsation is detected. Normal 60-100 bpm Bradycardia <60 bpm Tachycardia >100 bpm 2. Heart Rhythm The rhythm should be regular. A regularly irregular rhythm is one where the pulse is irregular but there is a pattern to the irregularity. For example every third beat is dropped. An irregularly irregular rhythm is one where the pulse is irregular and there is no pattern to the irregularity. The classic example of this is atrial fibrillation. 3. Blood Pressure Blood pressure should be measured in both arms, and should include an assessment of orthostatic change How to measure the Brachial Artery Blood Pressure: • Patient should be relaxed, in a supine or sitting position, with the arms positioned correctly(at, not above, the level of the heart) • Remember that measurements should be taken bilaterally • Choice of appropriate cuff size for the patient is important to accuracy of measured blood pressure. -

Myocarditis, Pericarditis and Other Pericardial Diseases
Heart 2000;84:449–454 Diagnosis is easiest during epidemics of cox- GENERAL CARDIOLOGY sackie infections but diYcult in isolated cases. Heart: first published as 10.1136/heart.84.4.449 on 1 October 2000. Downloaded from These are not seen by cardiologists unless they develop arrhythmia, collapse or suVer chest Myocarditis, pericarditis and other pain, the majority being dealt with in the primary care system. pericardial diseases Acute onset of chest pain is usual and may mimic myocardial infarction or be associated 449 Celia M Oakley with pericarditis. Arrhythmias or conduction Imperial College School of Medicine, Hammersmith Hospital, disturbances may be life threatening despite London, UK only mild focal injury, whereas more wide- spread inflammation is necessary before car- diac dysfunction is suYcient to cause symp- his article discusses the diagnosis and toms. management of myocarditis and peri- Tcarditis (both acute and recurrent), as Investigations well as other pericardial diseases. The ECG may show sinus tachycardia, focal or generalised abnormality, ST segment eleva- tion, fascicular blocks or atrioventricular con- Myocarditis duction disturbances. Although the ECG abnormalities are non-specific, the ECG has Myocarditis is the term used to indicate acute the virtue of drawing attention to the heart and infective, toxic or autoimmune inflammation of leading to echocardiographic and other investi- the heart. Reversible toxic myocarditis occurs gations. Echocardiography may reveal segmen- in diphtheria and sometimes in infective endo- -

Essentials of Bedside Cardiology CONTEMPORARY CARDIOLOGY
Essentials of Bedside Cardiology CONTEMPORARY CARDIOLOGY CHRISTOPHER P. CANNON, MD SERIES EDITOR Aging, Heart Disease and Its Management: Facts and Controversies, edited by Niloo M. Edwards, MD, Mathew S. Maurer, MD, and Rachel B. Wellner, MD, 2003 Peripheral Arterial Disease: Diagnosis and Treatment, edited by Jay D. Coffman, MD, and Robert T. Eberhardt, MD, 2003 Essentials ofBedside Cardiology: With a Complete Course in Heart Sounds and Munnurs on CD, Second Edition, by Jules Constant, MD, 2003 Primary Angioplasty in Acute Myocardial Infarction, edited by James E. Tcheng, MD,2002 Cardiogenic Shock: Diagnosis and Treatment, edited by David Hasdai, MD, Peter B. Berger, MD, Alexander Battler, MD, and David R. Holmes, Jr., MD, 2002 Management of Cardiac Arrhythmias, edited by Leonard I. Ganz, MD, 2002 Diabetes and Cardiovascular Disease, edited by Michael T. Johnstone and Aristidis Veves, MD, DSC, 2001 Blood Pressure Monitoring in Cardiovascular Medicine and Therapeutics, edited by William B. White, MD, 2001 Vascular Disease and Injury: Preclinical Research, edited by Daniell. Simon, MD, and Campbell Rogers, MD 2001 Preventive Cardiology: Strategies for the Prevention and Treatment of Coronary Artery Disease, edited by JoAnne Micale Foody, MD, 2001 Nitric Oxide and the Cardiovascular System, edited by Joseph Loscalzo, MD, phD and Joseph A. Vita, MD, 2000 Annotated Atlas of Electrocardiography: A Guide to Confident Interpretation, by Thomas M. Blake, MD, 1999 Platelet Glycoprotein lIb/IlIa Inhibitors in Cardiovascular Disease, edited by A. Michael Lincoff, MD, and Eric J. Topol, MD, 1999 Minimally Invasive Cardiac Surgery, edited by Mehmet C. Oz, MD and Daniel J. Goldstein, MD, 1999 Management ofAcute Coronary Syndromes, edited by Christopher P. -

Comparison of Traditional and Plethysmographic Methods for Measuring Pulsus Paradoxus
ARTICLE Comparison of Traditional and Plethysmographic Methods for Measuring Pulsus Paradoxus Jeff A. Clark, MD, FAAP; Mary Lieh-Lai, MD, FAAP; Ron Thomas, PhD; Kalyani Raghavan, MD; Ashok P. Sarnaik, MD, FAAP, FCCM Background: In the evaluation of patients with acute (PPpleth) on the pulse oximeter. Mean difference and asthma, pulsus paradoxus (PP) is an objective and non- 95% confidence intervals were calculated for each invasive indicator of the severity of airway obstruction. method. The 2 methods were also analyzed for correla- However, in children PP may be difficult or impossible tion and agreement using the Pearson product moment to measure. Indwelling arterial catheters facilitate the mea- correlation and a Bland and Altman plot. surement of PP, but they are invasive and generally re- served for critically ill patients. Results: Patients with status asthmaticus had higher PPausc and PPpleth readings compared with nonasthmatic pa- Objective: To determine the utility of the plethysmo- tients. Pulsus paradoxus measured by plethysmography graphic waveform (PPpleth) of the pulse oximeter in mea- in patients with and without asthma was similar to PPausc suring PP. readings (mean difference, 0.6 mm Hg; 95% confidence interval, −0.6 to 2.1 mm Hg). Individual PPpleth readings Methods: Patients from the pediatric intensive care showed significant correlation and agreement with PPausc unit, emergency department, and inpatient wards of a readings in patients both with and without asthma. tertiary care pediatric hospital were eligible for the study. A total of 36 patients (mean age [SD], 11.2 [4.7] Conclusion: Measurement of PP using the pulse oxim- years) were enrolled in the study. -

Constrictive Pericarditis Causing Ventricular Tachycardia.Pdf
EP CASE REPORT ....................................................................................................................................................... A visually striking calcific band causing monomorphic ventricular tachycardia as a first presentation of constrictive pericarditis Kian Sabzevari 1*, Eva Sammut2, and Palash Barman1 1Bristol Heart Institute, UH Bristol NHS Trust UK, UK; and 2Bristol Heart Institute, UH Bristol NHS Trust UK & University of Bristol, UK * Corresponding author. Tel: 447794900287; fax: 441173425926. E-mail address: [email protected] Introduction Constrictive pericarditis (CP) is a rare condition caused by thickening and stiffening of the pericar- dium manifesting in dia- stolic dysfunction and enhanced interventricu- lar dependence. In the developed world, most cases are idiopathic or are associated with pre- vious cardiac surgery or irradiation. Tuberculosis remains a leading cause in developing areas.1 Most commonly, CP presents with symptoms of heart failure and chest discomfort. Atrial arrhythmias have been described as a rare pre- sentation, but arrhyth- mias of ventricular origin have not been reported. Figure 1 (A) The 12 lead electrocardiogram during sustained ventricular tachycardia is shown; (B and C) Case report Different projections of three-dimensional reconstructions of cardiac computed tomography demonstrating a A 49-year-old man with a striking band of calcification around the annulus; (D) Carto 3DVR mapping—the left hand panel (i) demonstrates a background of diabetes, sinus beat with late potentials at the point of ablation in the coronary sinus, the right hand panel (iii) shows the hypertension, and hyper- pacemap with a 89% match to the clinical tachycardia [matching the morphology seen on 12 lead ECG (A)], and cholesterolaemia and a the middle panel (ii) displays the three-dimensional voltage map. -

J Wave Syndromes
Review Article http://dx.doi.org/10.4070/kcj.2016.46.5.601 Print ISSN 1738-5520 • On-line ISSN 1738-5555 Korean Circulation Journal J Wave Syndromes: History and Current Controversies Tong Liu, MD1, Jifeng Zheng, MD2, and Gan-Xin Yan, MD3,4 1Tianjin Key Laboratory of Ionic-Molecular Function of Cardiovascular disease, Department of Cardiology, Tianjin Institute of Cardiology, The Second Hospital of Tianjin Medical University, Tianjin, 2Department of cardiology, The Second Hospital of Jiaxing, Jiaxing, China, 3Lankenau Institute for Medical Research and Lankenau Medical Center, Wynnewood, Pennsylvania, USA, 4The First Affiliated Hospital, Medical School of Xi'an Jiaotong University, Xi'an, China The concept of J wave syndromes was first proposed in 2004 by Yan et al for a spectrum of electrocardiographic (ECG) manifestations of prominent J waves that are associated with a potential to predispose affected individuals to ventricular fibrillation (VF). Although the concept of J wave syndromes is widely used and accepted, there has been tremendous debate over the definition of J wave, its ionic and cellular basis and arrhythmogenic mechanism. In this review article, we attempted to discuss the history from which the concept of J wave syndromes (JWS) is evolved and current controversies in JWS. (Korean Circ J 2016;46(5):601-609) KEY WORDS: Brugada syndrome; Sudden cardiac death; Ventricular fibrillation. Introduction History of J wave and J wave syndromes The concept of J wave syndromes was first proposed in 2004 The J wave is a positive deflection seen at the end of the QRS by Yan et al.1) for a spectrum of electrocardiographic (ECG) complex; it may stand as a distinct “delta” wave following the QRS, manifestations of prominent J waves that are associated with a or be partially buried inside the QRS as QRS notching or slurring. -

Blood Pressure (BP) Measurements in Adults
Page 5 Blood Pressure (BP) Measurements in Adults Ramesh Khanna, MD Karl D. Nolph, MD Chair in Nephrology Professor of Medicine Director, Division of Nephrology University of Missouri-Columbia Uncontrolled high blood pressure is present in every 3rd person in the American community and is attributed to be a major risk factor for progression of chronic kidney disease, coronary artery disease, and stroke. Therefore, blood pressure recording is the most common measurements at home and by healthcare professionals in all of clinical medicine. It might come as a surprise that majority of recordings are done in a less than ideal circumstances and consequently performed inaccurately. BP measurements using mercury sphygmomanometer by a trained health care professional is the gold standard for clinical assessment of blood pressures. The appearance of the 1st Korotkoff sound signals the systolic blood pressure and the disappearance of the 5th sound denotes the diastolic blood pressure. The hypertension experts believe and have increasing evidence to suggest that this method frequently either over diagnose hypertension or fail to recognize masked hypertension (blood pressure that is normal in the physician’s office setting but high at other times including at home). The four commonly recognized reasons for this are: Avoidable inaccuracies in the methods, The inherent variability of blood pressure; and The tendency for blood pressure to increase in the presence of a health care professional (the so-called white coat effect). Failure to standardize blood pressure measurement dos and don’ts. It is believed and also to some extent evidence based that the health care providers including physicians often do not follow established guidelines for blood pressure measurement. -

Blood Pressure Year 1 Year 2 Core Clinical/Year 3+
Blood Pressure Year 1 Year 2 Core Clinical/Year 3+ Do Do • Patient at rest for 5 minutes • Measure postural BP and pulse in patients with a • Arm at heart level history suggestive of volume depletion or • Correct size cuff- bladder encircles 80% of arm syncope • Center of cuff aligns with brachial artery -Measure BP and pulse in supine position • Cuff wrapped snugly on bare arm with lower -Slowly have patient rise and stand (lie them down edge 2-3 cm above antecubital fossa promptly if symptoms of lightheadedness occur) • Palpate radial artery, inflate cuff to 70 mmHg, -Measure BP and pulse after 1 minute of standing then increase in 10 mmHg increments to 30 mmHg above point where radial pulse disappears. Know Deflate slowly until pulse returns; this is the • Normally when a person stands fluid shifts to approximate systolic pressure. lower extremities causing a compensatory rise in • Auscultate the Korotkoff sounds pulse by up to 10 bpm with BP dropping slightly -place bell lightly in antecubital fossa • Positive postural vital signs are defined as -inflate BP to 20-30mmHg above SBP as determined symptoms of lightheadedness and/or a drop in by palpation SBP of 20 mmHg with standing -deflate cuff at rate 2mmHg/second while auscultating • Know variations in BP cuff sizes -first faint tapping (Phase I Korotkoff) = SBP; • A lack of rise in pulse in a patient with an Disappearance of sound (Phase V Korotkoff)=DBP orthostatic drop in pressure is a clue that the Know cause is neurologic or related or related to -Korotkoff sounds are lower pitch, better heard by bell medications (eg. -

Pericardial Effusion
Pericardial Effusion ABOUT THE DIAGNOSIS are incurable, and treatment is designed to extend life and keep Pericardial effusion refers to an accumulation of fluid around the heart, the pet comfortable. Other underlying causes may be correctable, within the pericardium. The pericardium is a membranous sac that such as foreign bodies or coagulation disorders. surrounds the heart. When fluid accumulates slowly, the pericardium stretches and enlarges to accommodate the fluid, meaning that symp- TREATMENT toms are absent or delayed. A more rapid accumulation can cause If cardiac tamponade is present, the fluid must be drained promptly immediate symptoms, even with relatively small amounts of pericardial by a procedure called pericardiocentesis. Using local anesthetic, your fluid accumulation. The presence of fluid causes symptoms because veterinarian passes a catheter between the ribs into the pericardial the fluid compresses the heart and interferes with normal filling of the sac, and the fluid is drawn off. Alleviating the fluid accumulation that heart with blood. Less blood filling the heart means that less blood compresses the heart will rapidly stabilize a pet’s circulation and is pumped to the body with each heartbeat. Pericardial effusion can cardiovascular status in the vast majority of cases. Treatment then increase the external pressure on the heart to the point that delivery of depends upon the cause of the condition. If the underlying condition blood to the body is severely compromised, a condition called cardiac cannot be corrected, sometimes a procedure called pericardiectomy tamponade. Severe cardiac tamponade is a life-threatening condition. is performed. This is a surgery of the chest in which the pericardial Pericardial effusion is more common in older, large breed dogs. -

Screening for Peripheral Artery Disease and Cardiovascular Disease Risk Assessment with Ankle Brachial Index in Adults the U.S
Understanding Task Force Recommendations Screening for Peripheral Artery Disease and Cardiovascular Disease Risk Assessment with Ankle Brachial Index in Adults The U.S. Preventive Services Task Force (Task The Task Force reviewed the use of ABI to screen for Force) has issued a final recommendation statement PAD and to predict a person’s risk of heart attacks on Screening for Peripheral Artery Disease (PAD) and stroke. The final recommendation statement and Cardiovascular Disease (CVD) Risk Assessment summarizes what the Task Force learned about with Ankle Brachial Index (ABI) in Adults. the potential benefits and harms of this screening: There is not enough evidence to judge the benefits This final recommendation statement applies to and harms of using ABI for this purpose. adults who do not have signs or symptoms of PAD and who have not been diagnosed with PAD, CVD, This fact sheet explains the recommendation and severe chronic kidney disease, or diabetes. what it might mean for you. PAD is a disease in which fatty deposits called plaque build up in What is peripheral the arteries, especially those in the legs. Over time, the plaque can block the flow of blood to the legs often artery disease? leading to pain with walking. What is Cardiovascular disease affects the heart and blood vessels. It is caused by a build up of plaque in arteries that supply the heart, brain, and cardiovascular other parts of the body. When the build up is in the legs it is called disease? PAD. Heart attacks and strokes are other common types of CVD. Facts About CVD and PAD Cardiovascular disease is the leading killer of both men and women in the United States. -

Pulsus Paradoxus
ERJ Express. Published on December 6, 2012 as doi: 10.1183/09031936.00138912 Pulsus paradoxus Olfa Hamzaoui1, Xavier Monnet2,3, Jean‐Louis Teboul2,3 1. Hôpitaux Universitaires Paris‐Sud, Hôpital Antoine Béclère, Service de Réanimation Médicale, 157, rue de la Porte de Trivaux, 92141 Clamart, France. 2. Hôpitaux Universitaires Paris‐Sud, Hôpital de Bicêtre, service de réanimation médicale, 78, rue du Général Leclerc, Le Kremlin‐Bicêtre, F‐94270 France. 3. Université Paris‐Sud, Faculté de médecine Paris‐Sud, EA4533, Le Kremlin‐Bicêtre, 63, rue Gabriel Péri, F‐94270 France. Address for correspondence: Prof. Jean‐Louis Teboul Service de réanimation médicale Centre Hospitalier Universitaire de Bicêtre 78, rue du Général Leclerc 94 270 Le Kremlin‐Bicêtre France e‐mail: jean‐[email protected] Phone: + 33 1 45 21 35 47 Fax: + 33 1 45 21 35 51 1 Copyright 2012 by the European Respiratory Society. Abstract Systolic blood pressure normally falls during quiet inspiration in normal individuals. Pulsus paradoxus is defined as a fall of systolic blood pressure of more than 10 mmHg during the inspiratory phase. Pulsus paradoxus can be observed in cardiac tamponade and in conditions where intrathoracic pressure swings are exaggerated or the right ventricle is distended, such as severe acute asthma or exacerbations of chronic obstructive pulmonary disease. Both the inspiratory decrease in left ventricular stroke volume and the passive transmission to the arterial tree of the inspiratory decrease in intrathoracic pressure contribute to the occurrence of pulsus paradoxus. During cardiac tamponade and acute asthma, biventricular interdependence (series and parallel) plays an important role in the inspiratory decrease in left ventricular stroke volume.