Lisker Book.Book
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

FOOD Fesnval State Health Department
. As . A - ; 7 ■ '• ’ .X -, ■) PAGE TWENTY-POU* THURSDAY. OCTOBER 17, 1967 liattflfgHlgr lEofttittg IJwalii Average Daily Net Prras Run The Weather Far the Week Ended October 12, 1067 Faraeant af D. 8. Wsatbar t m a a Supper and Fair. I t will open at !> The Little Flower of Jesus Moth Buckingham Church men will at The second of three Thursday sale a t the Legion Home.set for About Towd 1:30 p.m. and continue to 8:30, ers Circle-wrill hold a regular meet tend the,first laymen's supper of eyentng meeting will be held to Wednesday, Oct, 28. with aupper served at three sit- ing tomorrow night at 7:4S at the the season of the Hartford East night at Center Congregational 12,690 OcTBsloMBl ratal loalghL Law Th« LjuUes Aid Society of the tinga, S, 6 and 7 p.m. Urs. Alvah home of Mrs. James Murphy, 22 Asoociation of • Congregational Church in the Felowship room at The Manchester Community Play- SO to 55. Rnliaday, littia eaotar, B u c k in g h a fh CTongregatiorul. A. Rusaell, Mountain Rd. may be Waddell Rd. A toy demonstration Churches tomorrow at 6:45 p.m. 8 o'clock. Thd Rey.b Clifford O. era will meet at the home of their TOMORROW S ? Member of the Audit Mgh near 00.- Church h u eet the date of Satur called for reservations. MrsT Fred. will., follow the meeting. The co- at the F irst Congregational Simpson is conducting the series president Philip Russell, 33 Cham > Bureau of drcnlatton day, Not. -

Iprhent of FABRIC CLOVES On
rf ■ . -f ■ / I. 'X'- X ( ^AGE THIRTY-TWO 'X .» WEDNESDAY, OCTOBER 17, 19W X. Hwalh 'jl^T^R^.'Dany Net Press Run ■'Fur •tiik'vSJ’eek Ended The Weather det^Uev>l$. I9S6 Foraeaat of D. 8. WeatiMr I Gradual Vlearing, little chasg* In temperatdr^ tonight. ^977.near k MenkteVv of the ' M. Fair and cool Friday, high Bureau (^.^Cirrulatioit ; S lit BIRTHDAY SALE ■ X*,- near To. _ ■ /■ "Manchenter^A City o f Village Charm > 01-. LXXVI, NO. 16 (TWENTfiiepUR PAGES—TWO SfitTlONSl)' FABRIC CLOVES MANCHESTER, CONN., THURSDAY, OCTOBER 18, 1956 (Claulflad Advertiibif on Page $2) PRICE FIVE CENTS \ MANCHCfTER C0 NN*i Waahahle fsbric jfloVM in alip-on atylea with plain or tnm back. Double woven cotton or nylon. All white. Strikes Hit .'N.. THURSDAY - - FRIDAY - - SATURDAY Re,'. $2.00 N O W $ |* 5 9 p A iR Cited in Award P la n ts in East Reich SPECIAL SALE! U.S. Work in a Berlin, Oct. 18 {JP)— Labor unrest has erupted into slow Hand Mirrors Wa.shington, Oct. 18 (/P)— The former project manager'for down strikes in three Com- a $43 million expansion of a governpi^nt nickel plant testified niunist East German qities, a today that “ political pre.ssure” came into the 1954 award of West Berlin newspaper re the contract. Randall Cremer* who worked on the Nicaro, ported today. ' $ |.49 EACH Cuba, project as a vice president-^ ------------------------------------:------------- The Inde.iendent paper Der Tag ! of PYederick Share Co>-p., a con- SI Id 2,000 Red police had been Durite handle with mirror on stnirtion firm, told a House Gov ru.shed from East Beilin to the Nij^on in State both aides. -

Australian Institute of Tropical Health and Medicine, JCU
Australian Institute of Tropical Health 2013 Annual Report – December July and Medicine This annual report has been created in line with clause 11 of the Financial Incentive Agreement. This annual report covers the period 30 June 2013 to 31 December 2013 Annual Report For reporting period July 2013 to December 2014 Contents Introduction 1 A Message from the Director 3 Governance 4 Review Committee 5 Governance Structure 5 AITHM Advisory Board 7 AITHM Management Advisory Committee 7 AITHM Business Development Advisory Board 8 AITHM Executive Group 9 Infrastructure 10 Townsville 11 Project Control Group Members 12 Consultant Team 12 Progress 12 Milestone Report 13 Cairns 14 Progress 14 PCG Members 15 User Group Members 15 Torres Strait 16 Progress 16 Highlights 17 Appointment of Advisory Board Independent Chair 18 Development Grants 2014 (AITHM) 18 Faculty Grant Scheme 2013 (AITHM) 19 NHMRC Grants 20 Building Enabling Disciplines 21 Staff Appointments 23 New Equipment 23 Seminar Series 24 Media attention 25 Special Events 26 Sponsorship 26 Breakthroughs 27 Federal Commitment of Matching Funds 28 Appointment of Advisory Board Independent Chair 28 Appointment of Director 28 Townsville Planning 28 Informal Steering Committee 28 Challenges 28 Progress 29 Research Progress 30 Program 1 32 Australia’s Health Security and Biosecurity 32 Program 2 33 Health in Rural, Remote, Indigenous and Tropical Australia 33 Program 3 34 Health in tropics regionally and globally 34 Collaboration 35 Personnel 37 Executive 38 Administration Staff 38 Research Staff 38 Key Performance Indicators 39 Key Performance Indicators and Outcomes 40 Publications 44 Overview 45 Journal Articles 45 Conference Paper 59 Book Chapter 60 Book 60 Consultancy Report 60 Conclusion 61 Introduction 1 AITHM aims to fill a major gap that currently exists at the interface between cutting edge research and scientific expertise, and health service, workforce and policy delivery. -

Histkaiserperm00keenrich.Pdf
66/1 6~7 n&bu^ University of California Berkeley Regional Oral History Office University of California The Bancroft Library Berkeley, California Kaiser Permanente Medical Care Program Oral History Project Clifford H. Keene, M.D. HISTORY OF THE KAISER PERMANENTE MEDICAL CARE PROGRAM An Interview Conducted by Sally Smith Hughes 1985 1986 the Copyright ( by Regents of the University of California All uses of this manuscript are covered by a legal agreement between the University of California and Clifford H. Keene, M.D., dated April 18, 1985. The manuscript is thereby made available for research purposes . All literary rights in the manuscript, including the right to publish, are reserved to The Bancroft Library of the University of California at Berkeley. No part of the manuscript may be quoted for publication without the written permission of the Director of The Bancroft Library of the University of California at Berkeley. Requests for permission to quote for publication should be addressed to the Regional Oral History Office, 486 Library, and should include identification of the specific passages to be quoted, anticipated use of the passages, and identification of the user. The legal agreement with Clifford H. Keene, M.D., requires that he be notified of the request and allowed thirty days in which to respond. It is recommended that this oral history be cited as follows : Clifford H. Keene, M.D. , "History of the Kaiser Permanente Medical Care Program," an oral history conducted in 1985 by Sally Smith Hughes, Regional Oral History Office, The Bancroft Library, University of California, Berkeley, 1986. Copy No. -

Health Behavior Emerging Research Perspectives Health Behavior Emerging Research Perspectives
Health Behavior Emerging Research Perspectives Health Behavior Emerging Research Perspectives Edited by David S. Gochman Raymond S. Kent School of Social Work University of Louisville Louisville, Kentucky SPRINGER SCIENCE+BUSINESS MEDIA, LLC Library of Congress Cataloging in Publication Data Health behavior: emerging research perspectives / edited by David S. Gochman. p. cm. Includes bibliographies and index. 1. Health behavior. I. Gochman, David S. RA776.9.H43 1988 88-19672 613-dcl9 CIP ISBN 978-1-4899-0835-3 ISBN 978-1-4899-0833-9 (eBook) DOI 10.1007/978-1-4899-0833-9 109 8765 © Springer Science+Business Media New York 1998 Originally published by Plenum Press, New York in 1998 Softcover reprint of the hardcover 1st edition 1998 All rights reserved No part of this book may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, microfilming, recording, or otherwise, without written permission from the Publisher This book is dedicated to the cherished memory of my parents, Edward B. and Vesta Gabriel Gochman, who early in my life encouraged me to persevere, to seek quality, and to pursue scholarship; and to Esselyn C. Rudikoff, a psychologist and treasured friend, whose example and insights inspired me to understand behavior. Contributors Arnold Arluke Department of Sociology and Anthropology, Northeastem University, Boston, Massachusetts Alice J. Baumgart School of Nursing, Queen's University, Kingston, Ontario, Canada Zeev Ben-Sira School of Social Work, The Hebrew University of Jerusalem, Mount Sco pus, Jerusalem, Israel Philip K. Berger Martin School of Public Administration, University of Kentucky, Lex ington, Kentucky John G. -

Regional Oral History Office the Bancrof T Library University Of
Regional Oral History Office University of California The Bancrof t Library Berkeley, California Kaiser Permanente Medical Care Program Oral History Project Morris F. Collen, M.D. HISTORY OF THE KAISER PERMANENTE MEDICAL CARE PROGRAM An Interview Conducted by Sally Smith Hughes 1986 Copyright @ 1988 by the Regents of the University of California Since 1954 the Regional Oral History Office has been interviewing leading participants in or well-placed witnesses to major events in the development of Northern California, the West,and the Nation. Oral history is a modern research technique involving an interviewee and an informed interviewer in spontaneous conversation. The taped record is transcribed, lightly edited for continuity and clarity, and reviewed by the interviewee. The resulting manuscript is typed in final form, indexed, bound with photographs and illustrative materials, and placed in The Bancroft Library at the University of California, Berkeley, and other research collections for scholarly use. Because it is primary material, oral history is not intended to present the final, verified, or complete narrative of events. It is a spoken account, offered by the interviewee in response to questioning, and as such it is reflective, partisan, deeply involved, and irreplaceable. All uses of this manuscript are covered by a legal agreement between the University of California and Morris F. Collen, M.D., dated December 3, 1986. The manuscript is thereby made available for research purposes. All literary rights in the manuscript, including the right to publish, are reserved to The Bancroft Library of the University of California, Berkeley. No part of the manuscript may be quoted for publication without the written permission of the Director of The Bancroft Library of the University of California, Berkeley. -

Canned Hams Butter
‘ * •r-’* 7 - 4 S i x t e e n MONDAY; MAY A 1964 Drty>Net PreM San jPatiflffalgr * For m , Wwik ilmfad I... May 3, 1964 The Daughters of the Union Daughters of Liberty No. 136 CShbomi Assembly, Catholic are reminded to bring rummage 15% Y es Vote About I'own Vstomns o f the Civil War will of Cdumbus will 13,961 M r eool. toaigbt, Rw meat tonight'at 8 at the home articles to Orange HaU tomor Us* hnnual installation Wsdn(«^l 0OO Attend StJlifarys Priest Accepts of Mrs. James M. Shearer, 113 row evening at 7 pm. to be day at 6:30 pm. at Needed to Pats ' J**"!!;® 9f th, AuiUt to 48.' Wedwme.maeri Iflipak Qreto oC South M«th- Bu h S i of Circulation Ad&rt Church wiU. moet at Su> Russell St. used at the sale Wednesday a f Restaurant, Walmtt RL Aiiyons^ M R A SHOW / Call of Torrington Church warm, high T8 M 09. aaanah Wesley Hall tomorrow 9 am . at the same place. who desires to attsM but hss Qiarter Items Maneheater • 4 City of Village Charm at 13:30. Mrs. Oscar Oronlund The Motherhood of Mary’s not been oont^Md may contact Mother’s Circle will meet at 8. will praaent ‘The Glory of WUd Circle 12 groi^iL of WSCS of M rs.' Jamas BlanchflekI, 81 On Renevoajk The R«v. William V. Q«nder,< »wtiat we have learned from his Yhs tripia quastlcwa to be VOL. LXXXDL NO. 184 Flowers,” ^ t h colored slides tonight at the home of Mrs. -
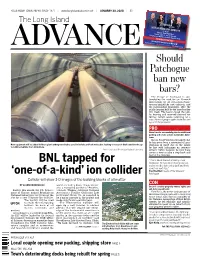
BNL Tapped for 'One-Of-A-Kind' Ion Collider
YOUR HOMETOWN PAPER SINCE 1871 | www.longislandadvance.net | JANUARY 30, 2020 | $1 VOTE ON WEDNESDAY, MARCH 18 RE-ELECT Mayor Paul Pontieri Trustee John A. (Jack) Krieger Trustee Lori Devlin • Trustee Thomas Ferb EXPERIENCE YOU CAN TRUST FOLLOW @PATCHOGUE2020 ON #PATCHOGUE2020 Paid for by Friends of PAtchogue PATCHOGUE2020.COM Should Patchogue ban new bars? The Village of Patchogue is con- templating the need for an 18-month moratorium on all restaurants/bars/ taverns/nightclubs and cabarets, and the surrounding downtown, after the public hearing held by the board earlier this week. The board closed the pub- lic hearing and reserved decision for further review before returning for a vote. Several people spoke both for and against the proposal. PRO Gives time to successfully plan for additional parking and create a more sustainable down- town Mayor Paul Pontieri proclaimed that he has never been a proponent of mor- New equipment will be added to these giant underground tubes used to isolate and test molecules, leading to research that could involve up atoriums in itself due to the issues to 1,000 scientists from 30 nations. he has with infringing on property Photos courtesy of Brookhaven National Laboratory owners’ rights; however, he said, there comes a time to take a step back and look at the situation. “This is about the sustainability of our BNL tapped for downtown. We have been moving too fast, and we need to take a step back and think about our next step.” Paul Pontieri, mayor of the Village of ‘one-of-a-kind’ ion collider Patchogue Collider will show 3-D images of the building blocks of all matter BY GLENN ROHRBACKER world, including Stony Brook Univer- CON sity, a managing partner of Brookha- Doesn’t consider property owners’ rights and Earlier this month, the U.S. -

Transhistmedprog00lewirich.Pdf
University of California Berkeley REGIONAL ORAL HISTORY OFFICE Regional Oral History Office University of California The Bancroft Library Berkeley, California Kaiser Permanente Medical Care Program Oral History Project Benjamin Lewis, M.D. HISTORY OF THE KAISER PERMANENTE MEDICAL CARE PROGRAM An Interview Conducted by Ora Huth 1986 Copyright (cj 1990 by the Regents of the University of California Since 1954 the Regional Oral History Office has been interviewing leading participants in or well -placed witnesses to major events in the development of Northern California, the West, and the Nation. Oral history is a modern research technique involving an interviewee and an informed interviewer in spontaneous conversation. The taped record is transcribed, lightly edited for continuity and clarity, and reviewed by the interviewee. The resulting manuscript is typed in final form, indexed, bound with photographs and illustrative materials, and placed in The Bancroft Library at the University of California, Berkeley, and other research collections for scholarly use. Because it is primary material, oral history is not intended to present the final, verified, or complete narrative of events. It is a spoken account, offered by the interviewee in response to questioning, and as such it is reflective, partisan, deeply involved, and irreplaceable. ************************************ All uses of this manuscript are covered by a legal agreement between the University of California and M.D. dated June 1986. The Benjamin Lewis, , 2, manuscript is thereby made available for research purposes. All literary rights in the manuscript, including the right to publish, are reserved to The Bancroft Library of the University of California, Berkeley. No part of the manuscript may be quoted for publication without the written permission of the Director of The Bancroft Library of the University of California, Berkeley. -

A Stylish Addition
July 2016 | No.163 | ISSN 1322-3771 CEO TO RETIRE AFL FINALS ARRANGEMENTS FUNCTION NEWS MCC News A stylish addition Our new and improved facilities are proving popular with members. CLUB NEWS Tiger legend “KB” to join MCG sporting greats ormer Richmond Football Club premiership as a Bulldogs supporter in those champion, Kevin Bartlett, will be days and then having the honour of playing Fimmortalised with a bronze statue in five Richmond grand finals at the MCG. outside the MCG as the latest addition to "I played my first game here, I played my the Australia Post Avenue of Legends. milestones here, my 100th, 200th, 300th, The statue of the five-time premiership 400th games and I played my last game here player will be created by sculptor Lis as well and also my first game as coach and Johnson, following her outstanding previous my last game as coach. work on the Norm Smith, John Coleman, “So the MCG has had a big bearing on Neil Harvey and Jim Stynes statues situated my life, it's played a big part in my life and in Yarra Park between MCG Gate 2 and I'm absolutely thrilled. It's a great honour." Jolimont station. It is expected that the Bartlett’s 778 career goals tally is still Bartlett statue will be completed and the 12th highest in VFL/AFL history. He unveiled prior to the start of the AFL season kicked 379 of them at the MCG, a then next March. record at the venue that has since only been During a 403-game career with surpassed by Matthew Richardson (464), Richmond between 1965 and 1983, Matthew Lloyd (461), David Neitz (386) including 27 finals, Bartlett was a highly and Wayne Carey (380). -

Pegasus January 1943
THE PEGASUS THE JOURNAL OF THE GEELONG COLLEGE Vol. XXXIII JANUARY 1943 No. 2. Contents : page School Officers .. .. .. .. .. .. .. .. .. 2 Editorial .. .. .. .. .. .... .. .. .. 3 School Items .. .. .. .. .. .. .. .. .. 4 Salvete et Valete .. .. .. .. .. .. .. .. .. 6 Speech Day .. .. .. .. .. .. .. .. 7 Debating Society .. .. .. .. .. 14 Music Notes .. .. .. .. .. .. .. .. .. 15 House of Guilds .. .. .. .. .. .. .. .. .. 21 Cadet Notes .. .. .. .. .. .. .. .. .. 22 Air Training Corps . .. .. .. .. .. 24 House Competition .. .. .. .. .. .. .. .. 25 First Aid . .. .. .. .. .. .. .. 25 Sports Awards .. .. .. .. .. .. .. .. .. 26 Football .. ., 28 Athletics .. .. .. .. .. .. .. .. .. 34 Rowing Notes .. .. .. .. .. .. .. .. .. 39 Tennis Notes .. .. .. .. .. .. .. .. .. 39 Cricket . .. .. .. .. .. .. .. .. 42 Preparatory School Notes .. .. .. .. .. 44 Kindergarten Notes .. .. .. .. .. .. .. .. 47 Preparatory School Speech Night .. .. .. .. .. 48 Old Boys' Section .. .. .. .. .. .. .. .. 50-64 Association News .. .. .. .. .. .. .. .. 50 A Message from the Principal .. .. .. .. .. .. 51 War Service .. .. .. .. .. .. .. .. .. 52-57 Letters from Old Boys .. .. .. .. .. .. .. .. 57 Mess-Hut Gossip .. .. .. .. .. .. .. .. .. 59 The Ormond Letter .. .. .. .. .. .. .. .. 60 Personal Notes 61-64 HENRY THACKER, PRINTERS, GEELONG 2 THE PEGASUS, School Officers, Term HI, 1942. Captain of School—J. A. C. McDonald. Prefects—J. K. Buchanan, T. B. Howells, D. G. Hope Johnstone, B. A. Johnson, K. B. Kelsall, D. H. King, L. W. McBean, J. A. C. McDonald, K. S. Nail, D. B. Rolland, J. N. Souter, D. S. Vanrenen. House Captains—Calvert: D. G. Hope Johnstone, vice-captain, B. A. Johnson; Morrison: S. K. Pearson, vice-captain, N. L. Davidson; Shannon: L. W. McBean, vice-captain, R. P. Charles; Warrinn: K. S. Nail, vice-captain, D. S. Vanrenen. "The Pegasus" Committee—J. A. C. McDonald, I. A. Gordon (co-editors), G. I. Cherry, G. R. Cook, N. L. Davidson, K. S. Nail; Old Collegians, Mr. B. R. Keith. Music Committee—Mr. G. Logie Smith, D. M. Drury, G. H. Harclie, K. B. Kelsall, K. S.