Female Reproductive System IUSM – 2016 I
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

In Hardening of the Zona Pellucida K
Disulfide formation in bovine zona pellucida glycoproteins during fertilization: evidence for the involvement of cystine cross-linkages in hardening of the zona pellucida K. Kwamoto, K. Ikeda, N. Yonezawa, S. Noguchi, K. Kudo, S. Hamano, M. Kuwayama and M. Nakano department ofChemistry, Faculty ofScience and 2Graduate School ofScience and Technology, Chiba University, 1-33 Yayoi-cho, Inage-ku, Chiba 263-8522, Japan; and3Animal Bio-Technology Center, Livestock Improvement Association, Tokyo, Japan The time for solubilization of the bovine zona pellucida in a hypotonic buffer containing 5% (v/v) \g=b\-mercaptoethanoland 7 mol urea l\m=-\1 increased by 10% after fertilization. Coupling with a specific fluorescent thiol probe, monobromobimane (mBBr), was markedly greater in the zona pellucida of ovarian eggs compared with fertilized eggs, indicating that the cysteine residues in the zona pellucida of unfertilized eggs are oxidized to cystines during fertilization. After endo-\g=b\-galactosidasedigestion to remove N-acetyllactosamine repeats of the carbohydrate chains, three zona pellucida glycoproteins (ZPA, ZPB and ZPC) coupled with the fluorescent bimane groups were fractionated efficiently by reverse-phase HPLC. Estimation of bimane groups in the three components and SDS-PAGE revealed that intramolecular disulfide bonds in ZPA and intra- and intermolecular disulfide bonds in ZPB were formed during fertilization, but oxidation of cysteine residues in ZPC was low. Specific proteolysis of ZPA during fertilization was also observed. These results indicate that the formation of disulfide linkages together with specific proteolysis result in the construction of a rigid zona pellucida structure, which is responsible for hardening of the zona pellucida. Introduction cross-linkages between tyrosine residues of the zona pellucida proteins formed by ovoperoxidase caused the The zona is one of the two sites at which pellucida In contrast to sea urchins (Foerder and is blocked and hardening. -

Chapter 28 *Lecture Powepoint
Chapter 28 *Lecture PowePoint The Female Reproductive System *See separate FlexArt PowerPoint slides for all figures and tables preinserted into PowerPoint without notes. Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Introduction • The female reproductive system is more complex than the male system because it serves more purposes – Produces and delivers gametes – Provides nutrition and safe harbor for fetal development – Gives birth – Nourishes infant • Female system is more cyclic, and the hormones are secreted in a more complex sequence than the relatively steady secretion in the male 28-2 Sexual Differentiation • The two sexes indistinguishable for first 8 to 10 weeks of development • Female reproductive tract develops from the paramesonephric ducts – Not because of the positive action of any hormone – Because of the absence of testosterone and müllerian-inhibiting factor (MIF) 28-3 Reproductive Anatomy • Expected Learning Outcomes – Describe the structure of the ovary – Trace the female reproductive tract and describe the gross anatomy and histology of each organ – Identify the ligaments that support the female reproductive organs – Describe the blood supply to the female reproductive tract – Identify the external genitalia of the female – Describe the structure of the nonlactating breast 28-4 Sexual Differentiation • Without testosterone: – Causes mesonephric ducts to degenerate – Genital tubercle becomes the glans clitoris – Urogenital folds become the labia minora – Labioscrotal folds -

Chapter 24 Primary Sex Organs = Gonads Produce Gametes Secrete Hormones That Control Reproduction Secondary Sex Organs = Accessory Structures
Anatomy Lecture Notes Chapter 24 primary sex organs = gonads produce gametes secrete hormones that control reproduction secondary sex organs = accessory structures Development and Differentiation A. gonads develop from mesoderm starting at week 5 gonadal ridges medial to kidneys germ cells migrate to gonadal ridges from yolk sac at week 7, if an XY embryo secretes SRY protein, the gonadal ridges begin developing into testes with seminiferous tubules the testes secrete androgens, which cause the mesonephric ducts to develop the testes secrete a hormone that causes the paramesonephric ducts to regress by week 8, in any fetus (XX or XY), if SRY protein has not been produced, the gondal ridges begin to develop into ovaries with ovarian follicles the lack of androgens causes the paramesonephric ducts to develop and the mesonephric ducts to regress B. accessory organs develop from embryonic duct systems mesonephric ducts / Wolffian ducts eventually become male accessory organs: epididymis, ductus deferens, ejaculatory duct paramesonephric ducts / Mullerian ducts eventually become female accessory organs: oviducts, uterus, superior vagina C. external genitalia are indeterminate until week 8 male female genital tubercle penis (glans, corpora cavernosa, clitoris (glans, corpora corpus spongiosum) cavernosa), vestibular bulb) urethral folds fuse to form penile urethra labia minora labioscrotal swellings fuse to form scrotum labia majora urogenital sinus urinary bladder, urethra, prostate, urinary bladder, urethra, seminal vesicles, bulbourethral inferior vagina, vestibular glands glands Strong/Fall 2008 Anatomy Lecture Notes Chapter 24 Male A. gonads = testes (singular = testis) located in scrotum 1. outer coverings a. tunica vaginalis =double layer of serous membrane that partially surrounds each testis; (figure 24.29) b. -
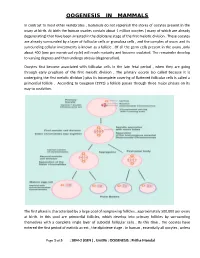
Oogenesis in Mammals
OOGENESIS IN MAMMALS In contrast to most other vertebrates , mammals do not replenish the stores of oocytes present in the ovary at birth. At birth the human ovaries contain about 1 million oocytes ( many of which are already degenerating) that have been arrested in the diplotene stage of the first meiotic division . These oocytes are already surrounded by a layer of follicular cells or granulosa cells , and the complex of ovum and its surrounding cellular investments is known as a follicle . Of all the germ cells present in the ovary ,only about 400 (one per menstrual cycle) will reach maturity and become ovulated. The remainder develop to varying degrees and then undergo atresia (degeneration). Oocytes first become associated with follicular cells in the late fetal period , when they are going through early prophase of the first meiotic division . The primary oocyte (so called because it is undergoing the first meiotic division ) plus its incomplete covering of flattened follicular cells is called a primordial follicle . According to Gougeon (1993) a follicle passes through three major phases on its way to ovulation. The first phase is characterized by a large pool of nongrowing follicles , approximately 500,000 per ovary at birth. In this pool are primordial follicles, which develop into primary follicles by surrounding themselves with a complete single layer of cuboidal follicular cells . By this time , the oocytes have entered the first period of meiotic arrest , the diplotene stage . In human , essentially all oocytes , unless Page 1 of 5 : SEM-2 (GEN ) , Unit#6 : OOGENESIS : Pritha Mondal they degenerate ,remain arrested in the diplotene stage until puberty ; some will not progress past the diplotene stage until the woman’s last reproductive cycle (age 45 to 55 years). -

FEMALE REPRODUCTIVE SYSTEM Female Reproduc�Ve System
Human Anatomy Unit 3 FEMALE REPRODUCTIVE SYSTEM Female Reproducve System • Gonads = ovaries – almond shaped – flank the uterus on either side – aached to the uterus and body wall by ligaments • Gametes = oocytes – released from the ovary during ovulaon – Develop within ovarian follicles Ligaments • Broad ligament – Aaches to walls and floor of pelvic cavity – Connuous with parietal peritoneum • Round ligament – Perpendicular to broad ligament • Ovarian ligament – Lateral surface of uterus ‐ ‐> medial surface of ovary • Suspensory ligament – Lateral surface of ovary ‐ ‐> pelvic wall Ovarian Follicles • Layers of epithelial cells surrounding ova • Primordial follicle – most immature of follicles • Primary follicle – single layer of follicular (granulosa) cells • Secondary – more than one layer and growing cavies • Graafian – Fluid filled antrum – ovum supported by many layers of follicular cells – Ovum surrounded by corona radiata Ovarian Follicles Corpus Luteum • Ovulaon releases the oocyte with the corona radiata • Leaves behind the rest of the Graafian follicle • Follicle becomes corpus luteum • Connues to secrete hormones to support possible pregnancy unl placenta becomes secretory or no implantaon • Becomes corpus albicans when no longer funconal Corpus Luteum and Corpus Albicans Uterine (Fallopian) Tubes • Ciliated tubes – Passage of the ovum to the uterus and – Passage of sperm toward the ovum • Fimbriae – finger like projecons that cover the ovary and sway, drawing the ovum inside aer ovulaon The Uterus • Muscular, hollow organ – supports -

GROSS and HISTOMORPHOLOGY of the OVARY of BLACK BENGAL GOAT (Capra Hircus)
VOLUME 7 NO. 1 JANUARY 2016 • pages 37-42 MALAYSIAN JOURNAL OF VETERINARY RESEARCH RE# MJVR – 0006-2015 GROSS AND HISTOMORPHOLOGY OF THE OVARY OF BLACK BENGAL GOAT (Capra hircus) HAQUE Z.1*, HAQUE A.2, PARVEZ M.N.H.3 AND QUASEM M.A.1 1 Department of Anatomy and Histology, Faculty of Veterinary Science, Bangladesh Agricultural University, Mymensingh-2202, Bangladesh 2 Chittagong Veterinary and Animal Sciences University, Khulshi, Chittagong 3 Department of Anatomy and Histology, Faculty of Veterinary and Animal Science, Hajee Mohammad Danesh Science and Technology University, Basherhat, Dinajpur * Corresponding author: [email protected] ABSTRACT. Ovary plays a vital 130.07 ± 12.53 µm and the oocyte diameter role in the reproductive biology and was 109.8 ± 5.75 µm. These results will be biotechnology of female animals. In this helpful to manipulate ovarian functions in study, both the right and left ovaries of small ruminants. the Black Bengal goat were collected from Keywords: Morphometry, ovarian the slaughter houses of different Thanas follicles, cortex, medulla, oocyte. in the Mymensingh district. For each of the specimens, gross parameters such as INTRODUCTION weight, length and width were recorded. Then they were processed and stained with Black Bengal goat is the national pride of H&E for histomorphometry. This study Bangladesh. The most promising prospect revealed that the right ovary (0.53 ± 0.02 of Black Bengal goat in Bangladesh is g) was heavier than the left (0.52 ± 0.02 g). that this dwarf breed is a prolific breed, The length of the right ovary (1.26 ± 0.04 requiring only a small area to breed and cm) was lower than the left (1.28 ± 0.02 with the advantage of their selective cm) but the width of the right (0.94 ± 0.02 feeding habit with a broader feed range. -

Ovarian Cancer Stroma: Pathophysiology and the Roles in Cancer Development
Cancers 2012, 4, 701-724; doi:10.3390/cancers4030701 OPEN ACCESS cancers ISSN 2072-6694 www.mdpi.com/journal/cancers Review Ovarian Cancer Stroma: Pathophysiology and the Roles in Cancer Development Mitsuko Furuya Department of Pathology, Yokohama City University Graduate School of Medicine, Yokohama 236-0004, Japan; E-Mail: [email protected]; Tel.: +81-45-787-2587; Fax: +81-45-786-0191 Received: 17 May 2012; in revised form: 29 June 2012 / Accepted: 12 July 2012 / Published: 18 July 2012 Abstract: Ovarian cancer represents one of the cancers with the worst prognostic in adult women. More than half of the patients who present with clinical signs such as abdominal bloating and a feeling of fullness already show advanced stages. The majority of ovarian cancers grow as cystic masses, and cancer cells easily spread into the pelvic cavity once the cysts rupture or leak. When the ovarian cancer cells disseminate into the peritoneal cavity, metastatic nests may grow in the cul-de-sac, and in more advanced stages, the peritoneal surfaces of the upper abdomen become the next largest soil for cancer progression. Ascites is also produced frequently in ovarian cancers, which facilitates distant metastasis. Clinicopathologic, epidemiologic and molecular studies on ovarian cancers have improved our understanding and therapeutic approaches, but still further efforts are required to reduce the risks in the patients who are predisposed to this lethal disease and the mortality of the patients in advanced stages. Among various molecules involved in ovarian carcinogenesis, special genes such as TP53, BRCA1 and BRCA2 have been well investigated. These genes are widely accepted as the predisposing factors that trigger malignant transformation of the epithelial cells of the ovary. -

Biology of the Corpus Luteum
PERIODICUM BIOLOGORUM UDC 57:61 VOL. 113, No 1, 43–49, 2011 CODEN PDBIAD ISSN 0031-5362 Review Biology of the Corpus luteum Abstract JELENA TOMAC \UR\ICA CEKINOVI] Corpus luteum (CL) is a small, transient endocrine gland formed fol- JURICA ARAPOVI] lowing ovulation from the secretory cells of the ovarian follicles. The main function of CL is the production of progesterone, a hormone which regu- Department of Histology and Embryology lates various reproductive functions. Progesterone plays a key role in the reg- Medical Faculty, University of Rijeka B. Branchetta 20, Rijeka, Croatia ulation of the length of estrous cycle and in the implantation of the blastocysts. Preovulatory surge of luteinizing hormone (LH) is crucial for Correspondence: the luteinization of follicular cells and CL maintenance, but there are also Jelena Tomac other factors which support the CL development and its functioning. In the Department of Histology and Embryology Medical Faculty, University of Rijeka absence of pregnancy, CL will cease to produce progesterone and induce it- B. Branchetta 20, Rijeka, Croatia self degradation known as luteolysis. This review is designed to provide a E-mail: [email protected] short overview of the events during the life span of corpus luteum (CL) and to make an insight in the synthesis and secretion of its main product – pro- Key words: Ovary, Corpus Luteum, gesterone. The major biologic mechanisms involved in CL development, Progesterone, Luteinization, Luteolysis function, and regression will also be discussed. INTRODUCTION orpus luteum (CL) is a transient endocrine gland, established by Cresidual follicular wall cells (granulosa and theca cells) following ovulation. -

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -

Formation of the Hamster Zona Pellucida in Relation to Ovarian Differentiation and Follicular Growth M
Formation of the hamster zona pellucida in relation to ovarian differentiation and follicular growth M. C. L\l=e'\veill\l=e'\,K. D. Roberts, S. Chevalier, A. Chapdelaine and G. Bleau Departments of Obstetrics and Gynecology, Biochemistry and Medicine, University of Montreal and Maisonneuve-Rosemont Research Center, Montreal, Quebec, Canada H1T 2M4 Summary. Using an immunofluorescence technique on ovarian sections, zona\x=req-\ immunoreactive components were detected in the cytoplasm of the oocyte from the beginning of its growth, when it is surrounded by only a thin squamous follicular cell layer, up to the end of its growth. In parallel with oocyte growth, the staining intensity decreased in the ooplasm. No staining was observed in the cytoplasm of the granulosa cells during normal follicular development in adult cyclic females. However, staining of the granulosa cells was observed at some stages of follicular development in immature females. This staining was especially evident in the ovaries of immature females (22 or 26 days old) stimulated with PMSG. In addition, the staining of the granulosa cells was consistently observed in ovaries showing an abnormal histology. Increased staining of the zona at its outer and inner regions could be distinguished in normal follicles, but when staining occurred on the granulosa cells no such pattern was observed over the zona matrix. These studies indicate that the oocyte itself but not the granulosa cells elaborates the native immunogenic material of the zona pellucida. The administration of PMSG at particular stages of ovarian differentiation interferes with follicular development leading to an abnormal extracellular assembly of the zona and its degradation (phagocytosis) by the surrounding granulosa cells. -

Changes in the Composition of the Hamster Zona Pellucida After Fertilization in Vivo but Not in Vitro C
Changes in the composition of the hamster zona pellucida after fertilization in vivo but not in vitro C. R. Brown, N. Clarke, M. Aiken and B. D. Bavister Institute of Animal Physiology and Genetics Research, Babraham Hall, Cambridge CB2 4AT, UK; and * Department ofVeterinary Science, University of Wisconsin, Madison, WI53706, USA Summary. Hamster zonae pellucidae were obtained from follicular oocytes, super- ovulated eggs, and eggs fertilized in vivo or in vitro. Zonae were labelled with N-succinimidyl-3(4-hydroxy,5-[125I]iodophenyl)propionate, and compared on single\x=req-\ and two-dimensional SDS-PAGE. Single-dimensional electrophoresis showed consider- able differences between zona categories in the amount of label that they incorporated; follicular zonae incorporated the least label and zonae from eggs fertilized in vivo the most. On two-dimensional electrophoresis, polypeptides from 3 of the 4 zona categories migrated into 4 major groups: two of these groups each with Mr 150 000\p=n-\250000 were within the Mr range of ZP1, and two others, at Mr90 000 and 55 000, appeared to be analogous to ZP2 and ZP3, respectively. The fourth zona category (zonae from eggs fertilized in vivo) showed a changed polypeptide profile as well as incorporating the most label; one of the polypeptides, Mr 150 000\p=n-\250000, was undetectable, but a train of Mr 70 000\p=n-\90000 polypeptides and a discrete polypeptide at Mr 20 000 were new. Since this changed profile did not occur in zonae from superovulated eggs, or in zonae from eggs fertilized in vitro, a synergism between oviducal factors and factors from the spermatozoon or egg, or both, towards the zona in vivo is indicated. -

Regulation and Roles of the Hyaluronan System in Mammalian Reproduction
REPRODUCTIONREVIEW Regulation and roles of the hyaluronan system in mammalian reproduction Ali A Fouladi-Nashta1, Kabir A Raheem1,2, Waleed F Marei1,3, Fataneh Ghafari1 and Geraldine M Hartshorne4 1Royal Veterinary College, Reproduction Research Group, Hawkshead Campus, Hatfield, UK, 2Department of Veterinary Surgery and Theriogenology, Michael Okpara University of Agriculture, Umudike, Nigeria, 3Department of Theriogenology, Faculty of Veterinary Medicine, Cairo University, Giza, Egypt and 4Warwick Medical School, University of Warwick, Coventry, UK and Centre for Reproductive Medicine, University Hospitals Coventry and Warwickshire NHS Trust, Coventry, UK Correspondence should be addressed to A A Fouladi-Nashta; Email: [email protected] Abstract Hyaluronan (HA) is a non-sulphated glycosaminoglycan polymer naturally occurring in many tissues and fluids of mammals, including the reproductive system. Its biosynthesis by HA synthase (HAS1–3) and catabolism by hyaluronidases (HYALs) are affected by ovarian steroid hormones. Depending upon its molecular size, HA functions both as a structural component of tissues in the form of high-molecular-weight HA or as a signalling molecule in the form of small HA molecules or HA fragments with effects mediated through interaction with its specific cell-membrane receptors. HA is produced by oocytes and embryos and in various segments of the reproductive system. This review provides information about the expression and function of members of the HA system, including HAS, HYALs and HA receptors. We examine their role in various processes from folliculogenesis through oocyte maturation, fertilisation and early embryo development, to pregnancy and cervical dilation, as well as its application in assisted reproduction technologies. Particular emphasis has been placed upon the role of the HA system in pre-implantation embryo development and embryo implantation, for which we propose a hypothetical sequential model.