HANDBOOK of Nursing DIAGNOSIS, 14Th EDITION
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chloracne: from Clinic to Research
DERMATOLOGICA SINICA 30 (2012) 2e6 Contents lists available at SciVerse ScienceDirect Dermatologica Sinica journal homepage: http://www.derm-sinica.com REVIEW ARTICLE Chloracne: From clinic to research Qiang Ju 1, Kuochia Yang 2, Christos C. Zouboulis 3, Johannes Ring 4, Wenchieh Chen 4,* 1 Department of Dermatology, Shanghai Skin Disease and STD Hospital, Shanghai, People’s Republic of China 2 Department of Dermatology, Changhua Christian Hospital, Changhua, Taiwan 3 Departments of Dermatology, Venereology, Allergology and Immunology, Dessau Medical Center, Dessau, Germany 4 Department of Dermatology and Allergy, Technische Universität München, Munich, Germany article info abstract Article history: Chloracne is the most sensitive and specific marker for a possible dioxin (2,3,7,8-tetrachlorodibenzo-p- Received: Oct 31, 2011 dioxin) intoxication. It is clinically characterized by multiple acneiform comedone-like cystic eruptions Revised: Nov 9, 2011 mainly involving face in the malar, temporal, mandibular, auricular/retroauricular regions, and the Accepted: Nov 9, 2011 genitalia, often occurring in age groups not typical for acne vulgaris. Histopathology is essential for adefinite diagnosis, which exhibits atrophy or absence of sebaceous glands as well as infundibular Keywords: dilatation or cystic formation of hair follicles, hyperplasia of epidermis, and hyperpigmentation of aryl hydrocarbon receptor stratum corneum. The appearance of chloracne and its clinical severity does not correlate with the blood chloracne “ ” 2,3,7,8-tetrachlorodibenzo-p-dioxin levels of dioxins. Pathogenesis of chloracne remains largely unclear. An aryl hydrocarbon receptor - polyhalogenated aromatic hydrocarbons mediated signaling pathway affecting the multipotent stem cells in the pilosebaceous units is probably sebaceous gland the major molecular mechanism inducing chloracne. -

Nursing Specialization in the UAE
Nursing Specialization in the UAE Specialization Committee Prepared by : Michelle Machon, RN, MSN Presented by: Aysha Al Mehri, RN Nursing Specialization Specialization refers to “the acquisition of a level of knowledge and skill in a particular area of nursing/ patient population which is greater than that acquired during the course of basic nursing education” (ICN, 2009) Levels of Specialty Description Education Qualification A nurse with experience in a certain area of No formal RN nursing who is recognized by the employer or education licensing authority as “specialized” in the field. Specialty specific certificate short courses e.g. one month RN wound care course Specialty nurses without general RN training (e.g. 3 year “direct RN pediatrics, psychiatry, etc.) entry” degree Post RN graduate specialty programs focusing on a 12-18 month post- Specialty RN patient population (e.g. peds, critical care, etc.) graduate diploma Specialized in a specific patient Masters level Specialty RN or population/disease process (e.g. Cardiology or program Advanced Neurosurgery Clinical Nurse Specialist) or in a Practice RN functional field of nursing (quality, education etc) “Advanced practice” nurse training resulting in Masters or PhD Advanced autonomous practitioners (Nurse level Practice RN Practitioner/Nurse Anesthetist). Possible Specialties worldwide 200 + including: Hyperbaric nursing Perioperative nursing Immunology and allergy nursing Private duty nursing Ambulatory care nursing Intravenous therapy nursing Psychiatric or mental health nursing -

Nurses: Are You Ready for Your New Role in Health Information Technology?
Nurses: Are You Ready for Your New Role in Health Information Technology? A 4-Part Educational Series Sponsored by TNA and TONE For 300,000 Texas Nurses Acknowledgement: Contribution by Susan McBride, PhD, RN and Mary Beth Mitchell, MSN, RN, BC-NI and the TNA/TONE HIT Task Force members © Texas Nurses Association, 2012 Webinar 4 Unintended Consequences of Using Electronic Health Records Mary Beth Mitchell, MSN, RN, BC Texas Health Resources Mari Tietze, PhD, RN, BC, FHIMSS Texas Woman’s University Introduction TNA/TONE Health IT Task Force • Charge: Determine implications of health care informatics for nursing practice and education in Texas • Include nationally-based Technology Informatics Guiding Education Reform (TIGER) initiative Vision: To enable nurses and interprofessional colleagues to use informatics and emerging technologies to make healthcare safer, more effective, efficient, patient-centered, timely and equitable by interweaving evidence and technology seamlessly into practice, education and research fostering a learning healthcare system. TNA = Texas Nurses Association http://www.thetigerinitiative.org/ TONE = Texas Organization of Nurse Executives 3 Introduction HIT Taskforce Membership Composed of TNA and TONE Members from practice and academia Task Force Members Texas Nurses Assoc. – David Burnett – Clair Jordan – Nancy Crider * – Joyce Cunningham – Mary Anne Hanley – Laura Lerma – Susan McBride – Molly McNamara – Mary Beth Mitchell – Elizabeth Sjoberg – Mari Tietze * * = Co-chairs 4 Why Does HIT Matter Introduction Environmental Forces: Deep in the Heart of • Health Care Reform/ARRA • Advanced Practice Nurse Roles Texas ? • EHR Incentives • IOM/RWJF Report Advancing Health Care • Informatics Nurse Standards by ANA Benchmark Reports on Progress CNE for Practicing Nurses Educational Content Dissemination Awareness Campaign HIT Orgs. -

Ds Support Feeding Problems
DS SUPPORT FEEDING PROBLEMS Acknowledgment: Down’s Heart Group (1998-2013) _________________________________________________________________________________________ Feeding Problems Babies with Down syndrome have a tendency to early feeding problems possibly as a result of poor muscle tone, and babies with a heart problem also tend to have problems as they tire easily when feeding. So, babies who have a heart defect and Down syndrome have two things making it harder for them and poor feeding and slow weight gain are common causes of anxiety for parents. If you are currently struggling with feeding your baby, perhaps the following will give you some ideas and encouragement or at the very least help relieve some stress. And whether breast or bottle fed, your baby is likely to settle and feed better with a relaxed mum rather than one who is constantly worrying about weight gain, so do try to enjoy your baby and not focus all your concentration on their weight. Weight Make sure their weight is being plotted on a growth chart specifically for children with Down syndrome. With a heart defect they are likely to be on a low centile (growth line) on the chart, but this will give a far more accurate picture than plotting them on a standard growth chart. Don’t expect too much, all babies lose weight after birth and those with heart problems and also those with Down syndrome tend to put on weight more slowly, so your baby is no different. The main thing is that their weight is monitored and that they continue to put on weight rather than losing it, even if the increase is very slow. -

Consumer Information
Consumer Information WARNING ENTRAPMENT/ WARNING STRANGULATION HAZARD • This package contains small parts. • Keep away from children during assembly. • Infants have died in TODDLER BEDS from • Adult assembly required. entrapment and strangulation. Failure to • Screws left after assembly should be kept out follow these warnings and the assembly of reach of children. instructions could result in serious injury or death. Assembly • NEVER place bed near windows where cords IMPORTANT! Before assembly or each use, from blinds or drapes may strangle a child. inspect this product for damaged hardware, • DO NOT place items with a string, cord, or loose joints, missing parts or sharp edges. ribbon around a child’s neck, such as hood DO NOT use if any parts are missing or strings or pacifier cords. damaged. • DO NOT suspend strings over a toddler bed Contact manufacturer for replacement parts for any reason. and instructions if needed. • Guardrails are used as a mattress Never substitute parts. containment means. Guardrails provided BE SURE bed rails are secure. Bed rails must must be used to avoid the formation of a gap be attached to headboard on the inside of the between the mattress and the bed that could post. cause entrapment. • Toddler bed must have more than 12 inches IMPORTANT: (31cm) of space between the toddler bed and •DO NOT use this bed without a mattress. solid objects such as a wall or dresser. Child could slide into small space and suffocate. • DO NOT use a water mattress with this Care And Maintenance toddler bed. To clean bed frame and bed rails, use only household soap or detergent and warm water. -

Pediatric Dysphagia: Who’S Ready, Who’S at Risk, and How to Approach
Pediatric Dysphagia: Who’s Ready, Who’s at Risk, and How to Approach Maria McElmeel, MA, CCC-SLP Laura Sayers, MA, CCC-SLP Megan Schmuckel, MA, CCC-SLP Erica Wisnosky, MA, CCC-SLP University of Michigan Mott Children’s Hospital Disclosure Statement We have no relevant financial or nonfinancial relationships to disclose. 2 Objectives Participants will be able to: • Identify at least one strategy to utilize with children exhibiting food refusal behaviors. • Identify safe and appropriate technique for feeding infant with cleft lip and palate. • Identify the four goals for a successful feeding in the NICU population. • Identify various feeding difficulties associated with cardiac and airway anomalies. 3 NICU Feeding Who’s Ready? • Increased early opportunities for oral feeding can lead to full oral feedings sooner (McCain & Gartside, 2002). • Gestational age = 32-34 weeks – Preterm infants unable to coordinate suck- swallow-breathe prior to 32 weeks (Mizuno & Ueda, 2003). – Often not fully organized until 34 weeks. • Behaviors or cues can be better indicators than age. • Growing body of research correlates cue-based feeding and decreased time to full oral feedings in healthy preterm infants. 5 What are the cues? • Physiological cues • Behavioral cues – Tolerates full enteral – Roots in response to feeds touch around the – Has a stable mouth respiratory system – Places hands to – Tolerates gentle mouth handling – Lip smacking – Able to transition to – Tongue protrusion an alert state – Searches for nipple – Has the ability to lick, when placed to nuzzle or suck non- breast nutritively 6 Cue-Based Feeding • A cue-based feeding model is an alternative to traditional medical models for feeding. -

Empowering Frontline Staff to Deliver Evidence-Based Care
Empowering frontline staff to deliver evidence-based care: The contribution of nurses in advanced practice roles Executive summary Kate Gerrish, Louise Guillaume, Marilyn Kirshbaum, Ann McDonnell, Mike Nolan, Susan Read, Angela Tod This Executive Summary presents the main findings from a major research study examining the contribution of advanced practice nurses1 (APNs) to promoting evidence-based practice among frontline staff. The study was commissioned by the Department of Health as part of its Policy Research Programme. Background The need for frontline staff to be empowered to deliver a quality service is a major aspect of contemporary healthcare policy.Within the nursing professions this has been supported by the introduction of new advanced practice roles such as consultant nurse and modern matron, to augment the existing clinical nurse specialist, nurse practitioner and practice development nurse roles. Policy guidance on advanced practice roles identifies the need for nurses in such positions to base not only their own practice on research evidence, but also through clinical leadership to act as change agents in promoting evidence-based care amongst frontline staff. Despite widespread recognition of the need for nursing practice to be based on sound evidence, frontline staff experience considerable challenges to implementing evidence-based care at an individual and organisational level. In particular, frontline nurses have difficulty interpreting research findings and although willing to use research they often lack the skills to do so. A lack of organisational support in the form of unsupportive colleagues and restricted local access to information is also problematic (Bryar et al 2003). Research examining evidence-based practice identifies the contribution that ‘opinion leaders’ such as advanced practice nurses make in influencing the practice of frontline staff (Fitzgerald et al 2003). -

W2990 Sleigh Toddler
Toddler bed (2990) - Assembly and Operation Manual Congratulations on purchasing a MDB Family product. This bed will provide many years of service if you adhere to the following guidelines for assembly, maintenance and operation. This bed is for residential use only. Any institutional use is strictly prohibited. Please be sure to follow the instructions for proper assembly. Use a Phillips head screwdriver for the assembling of the bed. Do not use power screwdrivers. All of our toddler beds are made from natural woods. Please understand that natural woods have color variations which are the result of nature and are not defects in workmanship. DO NOT SUBSTITUTE PARTS. ALL MODELS HAVE THE SAME QUANTITY OF PARTS AND HARDWARE. YOUR MODEL MAY LOOK DIFFERENT FROM THE ONE ILLUSTRATED DUE TO STYLISTIC VARIATIONS. Please read the Caution and Warning Statements insert before using your bed. revised 29DEC2011 page 1 PARTS C. Slats (10) D. Center slat A. Headboard B. Footboard E. Left side rail F. Right side rail HARDWARE G. 2” Allen head bolt (4) H. Barrel nut (14) K. Allen wrench J. 3 1/2” Allen head bolt (10) L. Lock washer (10) READ ALL INSTRUCTIONS BEFORE ASSEMBLING BED. WARNING: KEEP THE MANUAL FOR FUTURE USE. page 2 STEP 1. Fit the dowels of the slats (C) into the pre-drilled holes of the E left side rail (E). Attach the center slat (D) to the left side rail (E) using two 2” Allen head bolts (G) and two barrel nuts (H). C E G C G D H STEP 2. Attach the right side rail (F) in the same manner as step 1. -
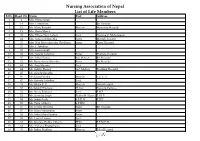
Nursing Association of Nepal List of Life Members S.No
Nursing Association of Nepal List of Life Members S.No. Regd. No. Name Post Address 1 2 Mrs. Prema Singh 2 14 Mrs. I. Mathema Bir Hospital 3 15 Ms. Manu Bangdel Matron Maternity Hospital 4 19 Mrs. Geeta Murch 5 20 Mrs. Dhana Nani Lohani Lect. Nursing C. Maharajgunj 6 24 Mrs. Saraswati Shrestha Sister Mental Hospital 7 25 Mrs. Nati Maya Shrestha (Pradhan) Sister Kanti Hospital 8 26 Mrs. I. Tuladhar 9 32 Mrs. Laxmi Singh 10 33 Mrs. Sarada Tuladhar Sister Pokhara Hospital 11 37 Mrs. Mita Thakur Ad. Matron Bir Hospital 12 42 Ms. Rameshwori Shrestha Sister Bir Hospital 13 43 Ms. Anju Sharma Lect. 14 44 Ms. Sabitry Basnet Ast. Matron Teaching Hospital 15 45 Ms. Sarada Shrestha 16 46 Ms. Geeta Pandey Matron T.U.T. H 17 47 Ms. Kamala Tuladhar Lect. 18 49 Ms. Bijaya K. C. Matron Teku Hospital 19 50 Ms.Sabitry Bhattarai D. Inst Nursing Campus 20 52 Ms. Neeta Pokharel Lect. F.H.P. 21 53 Ms. Sarmista Singh Publin H. Nurse F. H. P. 22 54 Ms. Sabitri Joshi S.P.H.N F.H.P. 23 55 Ms. Tuka Chhetry S.P.HN 24 56 Ms. Urmila Shrestha Sister Bir Hospital 25 57 Ms. Maya Manandhar Sister 26 58 Ms. Indra Maya Pandey Sister 27 62 Ms. Laxmi Thakur Lect. 28 63 Ms. Krishna Prabha Chhetri PHN F.P.M.C.H. 29 64 Ms. Archana Bhattacharya Lect. 30 65 Ms. Indira Pradhan Matron Teku Hospital S.No. Regd. No. Name Post Address 31 67 Ms. -

Preferred Home Health Manual
PREFERRED HOME HEALTH PROVIDER M A NUA L PRV20455-2102 Table of Contents Home Health Benefits ................................................................................................................................. 3 Introduction ....................................................................................................................................... 3 Filing a Home Health Claim ................................................................................................. 3 Conditions of Coverage for All Contracts ............................................................................. 3 Reimbursement ................................................................................................................... 3 Contract Exclusions ............................................................................................................ 3 Physical Therapy, Occupational Therapy and Speech Therapy ........................................... 4 Home Infusion Services ...................................................................................................... 4 Filing Home Health Drug Charges Electronically .................................................................. 4 Drugs Administered Outside the Patient’s Home................................................................. 5 Compound Drugs ............................................................................................................... 5 Factor Drugs ...................................................................................................................... -

Lawrlwytho'r Atodiad Gwreiddiol
Operational services structure April 2021 14/04/2021 Operational Leadership Structures Director of Operations Director of Nursing & Quality Medical Director Lee McMenamy Joanne Hiley Dr Tessa Myatt Medical Operations Operations Clinical Director of Operations Deputy Director of Nursing & Deputy Medical Director Hazel Hendriksen Governance Dr Jose Mathew Assistant Clinical Director Assistant Director of Assistant Clinical DWiraerctringor ton & Halton Operations Corporate Corporate Lorna Pink Assistant Assistant Director Julie Chadwick Vacant Clinical Director of Nursing, AHP & Associate Clinical Director Governance & Professional Warrington & Halton Compliance Standards Assistant Director of Operations Assistant Clinical Director Dr Aravind Komuravelli Halton & Warrington Knowsley Lee Bloomfield Claire Hammill Clare Dooley Berni Fay-Dunkley Assistant Director of Operations Knowsley Associate Medical Director Nicky Over Assistant Clinical Director Allied Health Knowsley Assistant Director of Sefton Professional Dr Ashish Kumar AssiOstapenrta Dtiironesc tKnor oofw Oslpeeyr ations Sara Harrison Lead Nicola Over Sefton James Hester Anne Tattersall Assistant Clinical Director Associate Clinical Director Assistant Director of St Helens & Knowsley Inpatients St Helens Operations Sefton Debbie Tubey Dr Raj Madgula AssistanAt nDniree Tcatttore ofrs aOllp erations Head of St Helens & Knowsley Inpatients Safeguarding Tim McPhee Assistant Clinical Director Sarah Shaw Assistant Director of Associate Medical Director Operations St Helens Mental Health -

Compensation for Occupational Skin Diseases
ORIGINAL ARTICLE http://dx.doi.org/10.3346/jkms.2014.29.S.S52 • J Korean Med Sci 2014; 29: S52-58 Compensation for Occupational Skin Diseases Han-Soo Song1 and Hyun-chul Ryou2 The Korean list of occupational skin diseases was amended in July 2013. The past list was constructed according to the causative agent and the target organ, and the items of that 1 Department of Occupational and Environmental list had not been reviewed for a long period. The revised list was reconstructed to include Medicine, College of Medicine, Chosun University, Gwangju; 2Teo Center of Occupational and diseases classified by the International Classification of Diseases (10th version). Therefore, Environmental Medicine, Changwon, Korea the items of compensable occupational skin diseases in the amended list in Korea comprise contact dermatitis; chemical burns; Stevens-Johnson syndrome; tar-related skin diseases; Received: 19 December 2013 infectious skin diseases; skin injury-induced cellulitis; and skin conditions resulting from Accepted: 2 May 2014 physical factors such as heat, cold, sun exposure, and ionized radiation. This list will be Address for Correspondence: more practical and convenient for physicians and workers because it follows a disease- Han-Soo Song, MD based approach. The revised list is in accordance with the International Labor Organization Department of Occupational and Environmental Medicine, Chosun University Hospital, 365 Pilmun-daero, Dong-gu, list and is refined according to Korean worker’s compensation and the actual occurrence of Gwangju 501-717, Korea occupational skin diseases. However, this revised list does not perfectly reflect the actual Tel: +82.62-220-3689, Fax: +82.62-443-5035 E-mail: [email protected] status of skin diseases because of the few cases of occupational skin diseases, incomplete statistics of skin diseases, and insufficient scientific evidence.