Development of the ICD-10 Procedure Coding System (ICD-10-PCS)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Alternative Treatment Method for Cervical Ectopic Pregnancy Servikal Ektopik Gebelik İçin Alternatif Tedavi Yöntemi
J Kartal TR 2016;27(2):147-149 CASE REPORT doi: 10.5505/jkartaltr.2015.065982 OLGU SUNUMU Alternative Treatment Method for Cervical Ectopic Pregnancy Servikal Ektopik Gebelik İçin Alternatif Tedavi Yöntemi Ali Emre TAHAOĞLU, Mehmet İrfan KÜLAHÇIOĞLU, Ahmet ESER, Cihan TOĞRU Diyarbakır Obstetrics and Child Health Hospital, Diyarbakır, Turkey Summary Özet Cervical ectopic pregnancy is a very rare form of ectopic Servikal ektopik gebelik, tüm ektopik gebelikler arasında çok pregnancy. Cervical ectopic pregnancy can be a cause of se- nadir rastalanan bir ektopik gebelik formudur. Servikal ektopik vere bleeding and it is associated with high morbidity and gebelik ciddi bir hemoraji nedeni olabilir. Ayrıca yüksek morbi- mortality. In recent years, many conservative methods of dite ve mortalite ile ilişkilidir. Son yıllarda fertiliteyi korumak treatment seeking to preserve fertility have been reported. amacı ile farklı birçok konservatif yaklaşım rapor edilmiştir. Presently described is case of pregnant woman at gesta- Kliniğimize yedi hafta dört gün ile uyumlu fetal kardiyak ak- tional age of 7 weeks and 4 days who was admitted to clinic tivitesi olmayan gebe vajinal kanama şikayeti ile başvurdu. with vaginal bleeding. Fetal cardiac activity was negative. Hasta yüksek servikal sütür ve Mcdonald serklaj uygulanarak Patient was successfully treated with high ligation suture başarı ile tedavi edildi. Servikal gebelik tedavisi hala tartışma and McDonald cerclage. There is no consensus yet on best konusudur. Fakat tedavi konusunda henüz kesin bir fikir birliği treatment of cervical ectopic pregnancy, but conservative bulunmamaktadır. Konservatif yaklaşım hastayı histerektomi methods can avoid major surgical procedure such as hyster- gibi büyük bir cerrahiden ve bunun getirdiği kötü sonuçlardan ectomy and its consequences. -

Surgical Best Practices: 14-Point Plan William P
Surgical Best Practices: 14-Point Plan William P. Adams, Jr., MD & Anand K. Deva, MBBS (Hons), MS SURGICAL BEST PRACTICES: 14-POINT PLAN William P. Adams, Jr., MD and Anand K. Deva, MBBS (Hons), MS Introduction The 14-Point Plan aims to reduce the number of bacteria present at the time of breast implant placement, thereby reducing the risk of associated infection.1 Each of these steps outlined below is backed by evidence and cumulatively have been shown to reduce the risk of capsular contracture in patients following breast implant surgery. During breast implant placement, if bacteria attach to the surface of an implant and create a biofilm over time, the biofilm becomes almost impossible to remove. If the bacterial biofilm load reaches a certain threshold it can lead to chronic inflammation and known sequelae, including infection, capsular contracture, double capsule, and breast implant-associated ALCL (BIA-ALCL).1, 2 We have performed extensive bench and clinical studies on this topic and are committed to educating plastic surgeons on proven steps that have been shown to reduce the bacterial biofilm load.1 These simple steps have been shown to decrease the risk of developing capsular contracture ten-fold.3-5 Additionally, a wealth of evidence has demonstrated a link between chronic inflammation from bacterial biofilm in the pathogenesis of BIA-ALCL, especially in textured devices where the increased surface area can result in an increased amount of bacterial biofilm.2 A meticulous procedure will help minimize the known and likely sequelae of bacterial attachment including infection and chronic biofilm, which is implicated in the pathogenesis of both capsular contracture and BIA-ALCL. -

Scarless Breast Augmentation by Dr
Scarless Breast Augmentation By Dr. Babak Farzaneh Trans-Umbilical Breast Augmenta- naval, allowing for a virtually undetect- volume adjustment for better symmetry. tion (TUBA), more commonly known able scar - even in patients with darker The path for placement shortly as the “Belly Button Procedure”, is the skin tone. This alleviates the need for heals without visible tracts, providing a most innovative and novel approach any incision on the breast. The incision quick return to normal activity. There is in the long history of breast implant is so minimal that some have nicknamed also no need for sharp cutting or burn- surgery. It has been a long time since a the procedure “Band-Aid Breast Aug- ing of the breast tissue, which mini- new approach has allowed a multitude mentation”. (Naval piercing, if present, mizes bleeding and the need for drains; of desirable additions without signifi- is left undisturbed, and the naval ring is post- procedure numbness; and, more cant drawbacks. Endoscopic surgery has sterilized and replaced at the conclusion tangibly, reduces bruising and swelling, revolutionized medicine and surgery, of the surgery.) allowing for shorter and easier recovery. allowing operations to be performed The highly unique instruments In skilled hands, this approach through smaller incisions. Following this specially manufactured for the TUBA allows for natural and predictable results trend, breast augmentation is comple- technique allow me to implement my through a very small, hidden incision. mented immensely by the introduction artistic vision to produce a natural breast As with most unique and highly special- of the TUBA technique. shape with acceptable symmetry, and ized surgical techniques, most surgeons Using a very small incision create the desirable cleavage. -

Core Neurosurgery
BAYLOR SCOTT & WHITE TEXAS SPINE & JOINT HOSPITAL NEUROLOGICAL SURGERY CLINICAL PRIVILEGES NAME: ________________________________ Initial appointment Reappointment All new applicants must meet the following requirements as approved by the governing body. To be eligible to apply for core privileges in neurological surgery, the initial applicant must meet the following criteria: Successful completion of ACGME or American Osteopathic Association accredited residency in neurological surgery. Required previous experience: Applicants for initial appointment must be able to demonstrate the performance of at least 50 neurological surgical procedures, reflective of the scope of privileges requested, during the last 12 months or demonstrate successful completion of residency or fellowship within the past 12 months. Reappointment requirements: To be eligible to renew core privileges in Neurological Surgery, the applicant must meet the following maintenance of privilege criteria: Current demonstrated competence and an adequate volume of neurological surgery procedures with acceptable results, reflective of the scope of privileges requested, for the past 24 months based on results of ongoing professional practice evaluation and outcomes. Evidence of current ability to perform privileges requested is required of all applicants for renewal of privileges NEUROLOGICAL SURGERY CORE PRIVILEGES Requested: Admit, evaluate, diagnose, consult and provide nonoperative and pre-, intran, and postoperative care to patients of all ages presenting with injuries -

Small Bowel Obstruction After Laparoscopic Roux-En-Y Gastric Bypass Presenting As Acute Pancreatitis: a Case Report
Netherlands Journal of Critical Care Submitted January 2018; Accepted April 2018 CASE REPORT Small bowel obstruction after laparoscopic Roux-en-Y gastric bypass presenting as acute pancreatitis: a case report N. Henning1, R.K. Linskens2, E.E.M. Schepers-van der Sterren3, B. Speelberg1 Department of 1Intensive Care, 2Gastroenterology and Hepatology, and 3Surgery, Sint Anna Hospital, Geldrop, the Netherlands. Correspondence N. Henning - [email protected] Keywords - Roux-en-Y, gastric bypass, pancreatitis, pancreatic enzymes, small bowel obstruction, biliopancreatic limb obstruction. Abstract Small bowel obstruction is a common and potentially life-threatening bowel obstruction within this complication after laparoscopic Roux-en-Y gastric bypass surgery. population, because misdiagnosis We describe a 30-year-old woman who previously underwent can have disastrous outcomes.[1,3-5,7] gastric bypass surgery. She was admitted to the emergency In this report we describe the department with epigastric pain and elevated serum lipase levels. difficulty of diagnosing small Conservative treatment was started for acute pancreatitis, but she bowel obstruction in post- showed rapid clinical deterioration due to uncontrollable pain and LRYGB patients and why frequent excessive vomiting. An abdominal computed tomography elevated pancreatic enzymes scan revealed small bowel obstruction and surgeons performed can indicate an obstruction in an exploratory laparotomy with adhesiolysis. Our patient quickly these patients. The purpose of improved after surgery and could be discharged home. This case this manuscript is to emphasise report emphasises that in post-bypass patients with elevated Figure 1. Roux-en-Y gastric bypass that in post-bypass patients with pancreatic enzymes, small bowel obstruction should be considered ©Ethicon, Inc. -

Acr–Nasci–Sir–Spr Practice Parameter for the Performance and Interpretation of Body Computed Tomography Angiography (Cta)
The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Revised 2021 (Resolution 47)* ACR–NASCI–SIR–SPR PRACTICE PARAMETER FOR THE PERFORMANCE AND INTERPRETATION OF BODY COMPUTED TOMOGRAPHY ANGIOGRAPHY (CTA) PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -

Neurosurgery
KALEIDA HEALTH Name ____________________________________ Date _____________ DELINEATION OF PRIVILEGES - NEUROSURGERY All members of the Department of Neurosurgery at Kaleida Health must have the following credentials: 1. Successful completion of an ACGME accredited Residency, Royal College of Physicians and Surgeons of Canada, or an ACGME equivalent Neurosurgery Residency Program. 2. Members of the clinical service of Neurosurgery must, within five (5) years of appointment to staff, achieve board certification in Neurosurgery. *Maintenance of board certification is mandatory for all providers who have achieved this status* Level 1 (core) privileges are those able to be performed after successful completion of an accredited Neurosurgery Residency program. The removal or restriction of these privileges would require further investigation as to the individual’s overall ability to practice, but there is no need to delineate these privileges individually. PLEASE NOTE: Please check the box for each privilege requested. Do not use an arrow or line to make selections. We will return applications that ignore this directive. LEVEL I (CORE) PRIVILEGES Basic Procedures including: Admission and Follow-Up Repair cranial or dural defect or lesion History and Physical for diagnosis and treatment plan* Seizure Chest tube placement Sterotactic framed localization of lesion Debride wound Sterotactic frameless localization Endotracheal intubation Transsphenoidal surgery of pituitary lesion Excision of foreign body Trauma Insertion of percutaneous arterial -

Information for Patients Having a Sigmoid Colectomy
Patient information – Pre-operative Assessment Clinic Information for patients having a sigmoid colectomy This leaflet will explain what will happen when you come to the hospital for your operation. It is important that you understand what to expect and feel able to take an active role in your treatment. Your surgeon will have already discussed your treatment with you and will give advice about what to do when you get home. What is a sigmoid colectomy? This operation involves removing the sigmoid colon, which lies on the left side of your abdominal cavity (tummy). We would then normally join the remaining left colon to the top of the rectum (the ‘storage’ organ of the bowel). The lines on the attached diagram show the piece of bowel being removed. This operation is done with you asleep (general anaesthetic). The operation not only removes the bowel containing the tumour but also removes the draining lymph glands from this part of the bowel. This is sent to the pathologists who will then analyse each bit of the bowel and the lymph glands in detail under the microscope. This operation can often be completed in a ‘keyhole’ manner, which means less trauma to the abdominal muscles, as the biggest wound is the one to remove the bowel from the abdomen. Sometimes, this is not possible, in which case the same operation is done through a bigger incision in the abdominal wall – this is called an ‘open’ operation. It does take longer to recover with an open operation but, if it is necessary, it is the safest thing to do. -

Members | Diagnostic Imaging Tests
Types of Diagnostic Imaging Tests There are several types of diagnostic imaging tests. Each type is used based on what the provider is looking for. Radiography: A quick, painless test that takes a picture of the inside of your body. These tests are also known as X-rays and mammograms. This test uses low doses of radiation. Fluoroscopy: Uses many X-ray images that are shown on a screen. It is like an X-ray “movie.” To make images clear, providers use a contrast agent (dye) that is put into your body. These tests can result in high doses of radiation. This often happens during procedures that take a long time (such as placing stents or other devices inside your body). Tests include: Barium X-rays and enemas Cardiac catheterization Upper GI endoscopy Angiogram Magnetic Resonance Imaging (MRI) and Magnetic Resonance Angiography (MRA): Use magnets and radio waves to create pictures of your body. An MRA is a type of MRI that looks at blood vessels. Neither an MRI nor an MRA uses radiation, so there is no exposure. Ultrasound: Uses sound waves to make pictures of the inside of your body. This test does not use radiation, so there is no exposure. Computed Tomography (CT) Scan: Uses a detector that moves around your body and records many X- ray images. A computer then builds pictures or “slices” of organs and tissues. A CT scan uses more radiation than other imaging tests. A CT scan is often used to answer, “What does it look like?” Nuclear Medicine Imaging: Uses a radioactive tracer to produce pictures of your body. -

Equilibrium Radionuclide Angiography/ Multigated Acquisition
EQUILIBRIUM RADIONUCLIDE ANGIOGRAPHY/ MULTIGATED ACQUISITION Equilibrium Radionuclide Angiography/ Multigated Acquisition S van Eeckhoudt, Bravis ziekenhuis, Roosendaal VJR Schelfhout, Rijnstate, Arnhem 1. Introduction Equilibrium radionuclide angiography (ERNA), also known as radionuclide ventriculography (ERNV), gated synchronized angiography (GSA), blood pool scintigraphy or multi gated acquisition (MUGA), is a well-validated technique to accurately determine cardiac function. In oncology its high reproducibility and low inter observer variability allow for surveillance of cardiac function in patients receiving potentially cardiotoxic anti-cancer treatment. In cardiology it is mostly used for diagnosis and prognosis of patients with heart failure and other heart diseases. 2. Methodology This guideline is based on available scientifi c literature on the subject, the previous guideline (Aanbevelingen Nucleaire Geneeskunde 2007), international guidelines from EANM and/or SNMMI if available and applicable to the Dutch situation. 3. Indications Several Class I (conditions for which there is evidence and/or general agreement that a given procedure or treatment is useful and effective) indications exist: • Evaluation of left ventricular function in cardiac disease: - Coronary artery disease - Valvular heart disease - Congenital heart disease - Congestive heart failure • Evaluation of left ventricular function in non-cardiac disease: - Monitoring potential cardiotoxic side effects of (chemo)therapy - Pre-operative risk stratifi cation in high risk surgery • Evaluation of right ventricular function: - Congenital heart disease - Mitral valve insuffi ciency - Heart-lung transplantation 4. Contraindications None 5. Medical information necessary for planning • Clear description of the indication (left and/or right ventricle) • Previous history of cardiac disease • Previous or current use of cardiotoxic medication PART I - 211 Deel I_C.indd 211 27-12-16 14:15 EQUILIBRIUM RADIONUCLIDE ANGIOGRAPHY/ MULTIGATED ACQUISITION 6. -
A Patient's Guide to Colostomy Care
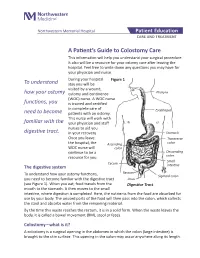
Northwestern Memorial Hospital Patient Education CARE AND TREATMENT A Patient’s Guide to Colostomy Care This information will help you understand your surgical procedure. It also will be a resource for your ostomy care after leaving the hospital. Feel free to write down any questions you may have for your physician and nurse. During your hospital Figure 1 To understand stay you will be visited by a wound, how your ostomy ostomy and continence Pharynx (WOC) nurse. A WOC nurse functions, you is trained and certified in complete care of Esophagus need to become patients with an ostomy. This nurse will work with familiar with the your physician and staff nurses to aid you digestive tract. in your recovery. Stomach Once you leave Transverse the hospital, the Ascending colon WOC nurse will colon continue to be a Descending resource for you. colon Small Cecum The digestive system intestine Rectum To understand how your ostomy functions, Sigmoid colon you need to become familiar with the digestive tract Anus (see Figure 1). When you eat, food travels from the Digestive Tract mouth to the stomach. It then moves to the small intestine, where digestion is completed. Here, the nutrients from the food are absorbed for use by your body. The unused parts of the food will then pass into the colon, which collects the stool and absorbs water from the remaining material. By the time this waste reaches the rectum, it is in a solid form. When the waste leaves the body, it is called a bowel movement (BM), stool or feces. -
Exploratory Laparotomy.Docx
EXPLORATORY LAPAROTOMY CONSENT FORM Your physician has determined that you may have a disease or abnormality inside your abdomen which may be life threatening, preventing pregnancy or causing medical problems if not treated. An exploratory laparotomy is an operation in which the doctor makes a surgical “cut” in the belly. Sometimes this operation is done to make sure that no disease or abnormality exists. If the physician finds that a disease is found or if the physician doesn’t feel that corrective surgery should be done immediately, then he will close up the surgical cut. If major corrective surgery is done the risk will be greater than if no corrective surgery is done. It is possible that you will be worse after the operation. Your physician can make no guarantee as to the result that might be obtained from this operation. Complications from exploratory surgery of the abdomen without any corrective surgery are infrequent, but they do occur. As with any surgical procedure, complications from bleeding and infection can occur. These complications can result in prolonged illness, the need for blood transfusions, poor healing wounds, scarring and the need for further operations. Other uncommon complications of this operation include: Damage to the intestines, blocked bowels, hernia or “rupture” developing at the site of the surgical cut, heart attacks or stroke, blood clots in the lungs and pneumonia. Some complications of exploratory surgery of the abdomen may require further surgery, some can cause permanent deformity and rarely, some can even be fatal. Furthermore, there may be alternative therapeutic or diagnostic methods available to you in addition to exploratory surgery.