Neutrophil Antibody Detection and Identification
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
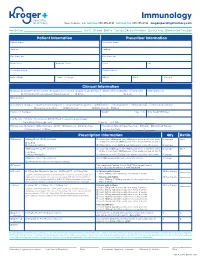
Immunology New Orleans, LA Toll Free 888.355.4191 Toll Free Fax 888.355.4192 Krogerspecialtypharmacy.Com
Immunology New Orleans, LA toll free 888.355.4191 toll free fax 888.355.4192 krogerspecialtypharmacy.com Need By Date: _________________________________________________ Ship To: Patient Office Fax Copy: Rx Card Front/Back Clinical Notes Medical Card Front/Back Patient Information Prescriber Information Patient Name Prescriber Name Address Address City State Zip City State Zip Main Phone Alternate Phone Phone Fax Social Security # Contact Person Date of Birth Male Female DEA # NPI # License # Clinical Information Diagnosis: J45.40 Moderate Asthma J45.50 Severe Asthma L20.9 Atopic Dermatitis L50.1 Chronic Idiopathic Urticaria (CIU) Eosinophil Levels J33 Chronic Rhinosinusitis with Nasal Polyposis Other: ________________________________ Dx Code: ___________ Drug Allergies Concomitant Therapies: Short-acting Beta Agonist Long-acting Beta Agonist Antihistamines Decongestants Immunotherapy Inhaled Corticosteroid Leukotriene Modifiers Oral Steroids Nasal Steroids Other: _____________________________________________________________ Please List Therapies Weight kg lbs Date Weight Obtained Lab Results: History of positive skin OR RAST test to a perennial aeroallergen Pretreatment Serum lgE Level: ______________________________________ IU per mL Test Date: _________ / ________ / ________ MD Specialty: Allergist Dermatologist ENT Pediatrician Primary Care Prescription Type: Naïve/New Start Restart Continued Therapy Pulmonologist Other: _________________________________________ Last Injection Date: _________ / ________ -

Infection Control for Neutropenic Cancer Patients : the Libraryuse of Prophylactic Antibiotics Lecture Author Jean A
Infection control for neutropenic cancer patients : the Libraryuse of prophylactic antibiotics Lecture author Jean A. Klastersky Onlineby Institut Jules Bordet,© Université Libre de Bruxelles (ULB) Brussels, Belgium ESCMID Complications and mortality associated with febrile neutropenia Library No Bacteremia Bacteremia Total ComplicationsLectureDeaths Total Complications Deaths author Solid tumors 784 60 (8 %) 25 135 30 (22 %) 17 Onlineby (3 %) (13 % ) © Hematological cancer 859 111 (13 %) 32 364 76 (21 %) 32 (4 %) (9 %) ESCMID J. Klastersky et al., 2007 2 Complications associated with febrile neutropenia Library Hypotension : systolic blood pressure less than 90 mmHg or need for pressor support to maintain blood pressure Respiratory failure : arterial oxygen pressure less than 60mmHg while breathing room air or needLecture for mechanical ventilation Disseminated intravascular coagulation Confusion or altered mental state author Congestive cardiac failure seen on chest X-ray and requiring treatment Onlineby Bleeding severe enough to require© transfusion Arrhythmia or ECG changes requiring treatment Renal failure requiring investigation and/or treatment with IV fluids, dialysis, or any other intervention ESCMID J. Klastersky et al., 2000 3 Cost of febrile neutropenia Library Initial hospitalization Initial hospitalization plus all downstreamLecture neutropenia care author 2.010 $ Onlineby 14.407 $ © ESCMID D. Weyckler et al., 2008 4 Use of oral antibiotics in protected units environment : clinical effectiveness and role in the emergence -

Neutropenia Fact Sheet
Neutropenia in Barth Syndrome i ii (Chronic, Cyclic or Intermittent) What problems can Neutropenia cause? Neutrophils are the main white blood cell for fighting or preventing bacterial or fungal infections. They may be referred to as polymorphonuclear cells (polys or PMNs), white cells with segmented nuclei (segs), or neutrophils in the complete blood cell count (CBC) report. Immature neutrophils are referred to as bands. When someone is neutropenic (an abnormally low level of neutrophils in the blood), the risk of infection increases. The absolute neutrophil count (ANC) is a measure of the total number of neutrophils present in the blood. When the ANC is less than 1,000, the risk of infection increases. Most infections occur in the ears, skin or throat and to a lesser extent, the chest. These infections can be very serious and may require antibiotics to clear infections. When someone with Barth syndrome is neutropenic his defenses are weakened, he is likely to become seriously ill more quickly than someone with a normal neutrophil count. Tips: • No rectal temperatures as any break in the skin can lead to an infection. • If the individual has a temperature > 100.4° F (38° C) or has infectious symptoms, the primary physician or hematologist should be notified. The individual may need to be seen. • If the individual has a temperature of 100.4° F (38° C) – 100.5° F (38.05° C)> 8 hours or a temperature > 101.5° F (38.61° C), an immediate examination by the physician is warranted. Some or all of the following studies may be ordered: CBC with differential and ANC Urinalysis Blood, urine, and other appropriate cultures C-Reactive Protein Echocardiogram if warranted • The physician may suggest antibiotics (and G-CSF if the ANC is low) for common infections such as otitis media, stomatitis. -

We Work at the Intersection of Immunology and Developmental Biology
Development and Homeostasis of Mucosal Tissues U934/UMR3215 – Genetics and Developmental Biology Pedro Hernández Chef d'équipe [email protected] We work at the intersection of immunology and developmental biology. Our primary goal is to understand how immune responses impact the development, integrity and function of mucosal tissue layers, such as the intestinal epithelium, during homeostasis and upon different types of stress, including infections. To study these questions we exploit the advantages of the zebrafish model such as ex utero and rapid development, transparency, large progeny, and simple genetic manipulation. We combine live imaging, flow cytometry, single-cell transcriptomics, and models inducing mucosal stress, including pathogenic challenges. Our research can be subdivided into three main topics: 1) Protection of intestinal epithelial integrity since early development: Epithelial cells are at the core of intestinal organ function. They are in charge of absorbing nutrients and water, and at the same time constitute a barrier for potential pathogens and harmful molecules. Epithelial cells perform all these functions before full development of the immune system, which promotes epithelial barrier function upon injury. We study how robust epithelial integrity is achieved prior and after maturation of the intestinal immune system, with a focus on the function of mucosal cytokines. 2) Epithelial-leukocyte crosstalk throughout development: Intestines become vastly populated by leukocytes after exposure to external cues from diet and colonization by the microbiota. We have recently reported the existence and diversity of zebrafish innate lymphoid cells (ILCs), a key component of the mucosal immune system recently discovered in mice and humans. ILCs mediate immune responses by secreting cytokines such as IL-22 which safeguards gut epithelial integrity. -

Immunology Stories: How Storytelling Can Help Us to Make Sense of Complex Topics
Immunology Stories: How Storytelling Can Help Us to Make Sense of Complex Topics Jennifer Giuliani, MSc Camosun College, Lansdowne Campus, 3100 Foul Bay Rd, Victoria BC V8P 5J2 [email protected] Abstract The immune response is a wonderfully complex aspect of our physiology that can sometimes confound students and instructors alike. How do we wade through the layers of detail to help our students develop an understanding of immunology? In this article, I will share some of the stories about immunology research that helped me strengthen my own understanding and improve my approach to helping students learn and understand this topic. In addition, we will explore some of the research on the power of storytelling, and how learning through stories might be a defining characteristic of what it means to be human. https://doi.org/10.21692/haps.2020.105 Key words: storytelling, immunology Introduction I have been trying to understand the immune response for a My personal journey to develop a better understanding of long time. Like many Anatomy and Physiology instructors, I the immune system was a compelling reminder to me of the did not have an immunology background beyond what was power of storytelling. Suddenly I saw examples of storytelling covered in my undergraduate physiology courses. When the everywhere that I saw authentic learning. In this article, I will time came for me to teach students about the immune system, share some of what I have learned about learning through I relied heavily on the information presented in our textbooks. stories, some of the fun and fascinating immunology stories I was able to present students with the key pieces of from Davis’ books, and my current approach to helping information and help them to remember a few facts, and the students understand the immune response. -

Journal of Microbiology, Immunology and Infection
JOURNAL OF MICROBIOLOGY, IMMUNOLOGY AND INFECTION AUTHOR INFORMATION PACK TABLE OF CONTENTS XXX . • Description p.1 • Impact Factor p.1 • Abstracting and Indexing p.2 • Editorial Board p.2 • Guide for Authors p.4 ISSN: 1684-1182 DESCRIPTION . Journal of Microbiology, Immunology and Infection, launched in 1968, is the official bi-monthly publication of the Taiwan Society of Microbiology, the Chinese Society of Immunology, the Infectious Diseases Society of Taiwan and the Taiwan Society of Parasitology. The journal is an open access journal, committed to disseminating information on the latest trends and advances in microbiology, immunology, infectious diseases and parasitology. Articles on clinical or laboratory investigations of relevance to microbiology, immunology, infectious diseases, parasitology and other related fields that are of interest to the medical profession are eligible for consideration. Article types considered include perspectives, review articles, original articles, brief reports and correspondence. The Editorial Board of the Journal comprises a dedicated team of local and international experts in the field of microbiology, immunology, infectious diseases and parasitology. All members of the Editorial Board actively guide and set the direction of the journal. With the aim of promoting effective and accurate scientific information, an expert panel of referees constitutes the backbone of the peer- review process in evaluating the quality and content of manuscripts submitted for publication. JMII is open access and indexed in SCIE, PubMed, MEDLINE, EMBASE, Scopus, AIDS & Cancer Reseach, CABI, BIOSIS Previews, Biological Abstracts, EBSCOhost, CancerLit, Reactions Weekly (online), Chemical Abstracts, HealthSTAR, Global Health, ProQuest. Benefits to authors We also provide many author benefits, such as free PDFs, a liberal copyright policy, special discounts on Elsevier publications and much more. -

Vancomycin-Resistant Enterococci Colonization in Patients with Hematological Malignancies: Screening and Its Cost-Effectiveness
Vancomycin-resistant enterococci colonization in patients with hematological malignancies: screening and its cost-effectiveness Gedik Habip1, Şimşek Funda1, Kantürk Arzu1, Yıldırmak Taner1, Arıca Deniz2, Aydın Demet2, Yokuş Osman2, Demirel Naciye2 1. Department of Infectious Diseases and Clinical Microbiology, Ministry of Health Okmeydanı Training and Research Hospital, Istanbul 2. Department of Hematology, Ministry of Health Okmeydanı Training and Research Hospital, Istanbul Abstract: Background and objective: We evaluated the rates of vancomycin-resistant enterococci (VRE) colonization and VRE- related bacteremia in patients with hematological malignancies in terms of routine screening culture and its cost-effective- ness. Materials and Methods: All patients of the hematology department who were older than 14 years of age and who devel- oped at least one febrile neutropenia episode during chemotherapy for hematological cancers between November 2010 and November 2012 were evaluated retrospectively. Results: We retrospectively analyzed 282 febrile episodes in 126 neutropenic patients during a two-year study period. The study included 65 cases in the first study-year and 78 cases in the second study-year. The numbers of colonization days and colonized patient were748 days of colonization in 29 patients (44%) in the first study-year and 547 colonization days in 21 patients (26%) in the second study-year, respectively. Routine screening culture for VRE cost $4516,4 (427 cultures) in the first study-year, $5082,7 (504 cultures) in the second study-year depending on the number of patients and their length of stay. Conclusion: In line with our study results, routine screening of hematological patients for VRE colonization is not cost- effective. Routine surveillance culture for VRE should be considered with respect to the conditions of health care setting. -

Eosinophils but Not of Neutrophils Stimulates Effector Functions of Human Interaction with Secretory Component
Interaction with Secretory Component Stimulates Effector Functions of Human Eosinophils But Not of Neutrophils This information is current as Youichi Motegi and Hirohito Kita of September 23, 2021. J Immunol 1998; 161:4340-4346; ; http://www.jimmunol.org/content/161/8/4340 Downloaded from References This article cites 49 articles, 20 of which you can access for free at: http://www.jimmunol.org/content/161/8/4340.full#ref-list-1 Why The JI? Submit online. http://www.jimmunol.org/ • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average by guest on September 23, 2021 Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 1998 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Interaction with Secretory Component Stimulates Effector Functions of Human Eosinophils But Not of Neutrophils1 Youichi Motegi and Hirohito Kita2 Eosinophils and their products are important in the pathophysiology of allergic inflammation in mucosal tissues. Secretory component bound to IgA mediates transepithelial transport of IgA and confers increased stability on the resultant secretory IgA; however, the effect of secretory component on the biologic activity of IgA is unknown. -

Cells, Tissues and Organs of the Immune System
Immune Cells and Organs Bonnie Hylander, Ph.D. Aug 29, 2014 Dept of Immunology [email protected] Immune system Purpose/function? • First line of defense= epithelial integrity= skin, mucosal surfaces • Defense against pathogens – Inside cells= kill the infected cell (Viruses) – Systemic= kill- Bacteria, Fungi, Parasites • Two phases of response – Handle the acute infection, keep it from spreading – Prevent future infections We didn’t know…. • What triggers innate immunity- • What mediates communication between innate and adaptive immunity- Bruce A. Beutler Jules A. Hoffmann Ralph M. Steinman Jules A. Hoffmann Bruce A. Beutler Ralph M. Steinman 1996 (fruit flies) 1998 (mice) 1973 Discovered receptor proteins that can Discovered dendritic recognize bacteria and other microorganisms cells “the conductors of as they enter the body, and activate the first the immune system”. line of defense in the immune system, known DC’s activate T-cells as innate immunity. The Immune System “Although the lymphoid system consists of various separate tissues and organs, it functions as a single entity. This is mainly because its principal cellular constituents, lymphocytes, are intrinsically mobile and continuously recirculate in large number between the blood and the lymph by way of the secondary lymphoid tissues… where antigens and antigen-presenting cells are selectively localized.” -Masayuki, Nat Rev Immuno. May 2004 Not all who wander are lost….. Tolkien Lord of the Rings …..some are searching Overview of the Immune System Immune System • Cells – Innate response- several cell types – Adaptive (specific) response- lymphocytes • Organs – Primary where lymphocytes develop/mature – Secondary where mature lymphocytes and antigen presenting cells interact to initiate a specific immune response • Circulatory system- blood • Lymphatic system- lymph Cells= Leukocytes= white blood cells Plasma- with anticoagulant Granulocytes Serum- after coagulation 1. -

Effect of Recombinant Granulocyte Colony-Stimulating Factor on Blood
Original ..............Article Effect of Recombinant Granulocyte Colony-Stimulating Factor on Blood Neutrophil Concentrations among Patients with ‘‘Idiopathic Neonatal Neutropenia’’: A Randomized, Placebo-controlled Trial Sandra E. Juul, MD, PhD INTRODUCTION Robert D. Christensen, MD A severe but self-limited idiopathic variety of neutropenia, termed ‘‘idiopathic neonatal neutropenia’’, has been described among preterm infants.1,2 Neonates with this condition have several features in common, including the fact that no specific variety of OBJECTIVES: neutropenia is diagnosed, it often appears late in the clinical We previously described a severe, prolonged, idiopathic, but self-resolving, course, can be quite prolonged, and generally occurs in otherwise variety of neutropenia among preterm neonates. In the present study, we well infants.1,2 It is not clear whether this condition is a single sought to assess the marrow neutrophil reserves of these patients by entity or represents multiple disorders with the common feature of serially measuring blood neutrophils following the administration of severe but self-limited neutropenia. As neutropenia in preterm recombinant granulocyte colony-stimulating factor (rG-CSF) or placebo. infants can be a sign of incipient severe illness, particularly sepsis, STUDY DESIGN: this variety of neutropenia in the neonatal intensive care unit (NICU) often causes concern, and sometimes prompts evaluations Prospective, randomized trial of rG-CSF vs placebo for infants with for infection and repeated or prolonged -

Granulocyte Transfusions in Haematopoietic Cell Transplants and Leukaemia: the Phoenix Or Beating a Dead Horse?
www.nature.com/bmt EDITORIAL Granulocyte transfusions in haematopoietic cell transplants and leukaemia: the phoenix or beating a dead horse? © The Author(s), under exclusive licence to Springer Nature Limited 2021 Bone Marrow Transplantation (2021) 56:2046–2049; https://doi.org/10.1038/s41409-021-01399-3 You should make a point of trying every experience once, excepting incest and folk-dancing. (and perhaps granulocyte transfusions?) Sir Arnold Bax Why is it some things which are so intuitive and seem easily proved continue engendering controversy and debate (Fig. 1). The example at hand is granulocyte transfusions. It has been known for >50 years infection risk increases precipitously in people when their blood granulocyte concentration is <0.5 × 10E + 9/L [1, 2] (Fig. 2). Whether, given the development of more effective systemic and oral non-absorbable antibiotics and anti-fungal drugs, often given prophylactically 0.5 × 10E + 9/L remains the threshold for increased infection risk or whether the threshold is closer 0–0.2 × 10E + 9/L is unknown. It is also possible there is no blood granulocyte nadir requiring granulocyte transfusions or where a benefit of granulocyte transfusions can be convincingly proved. Regardless, the seemingly simple remedy to decreased Fig. 1 Centre for the Study of Rationality. Hebrew Univ. Jerusalem. blood granulocytes is to transfuse granulocytes from normals or, formally, from persons with chronic myeloid leukaemia (CML). Amino™ (now renamed CelltrifugeTM)orbyfiltration leukapheresis Why should granulocyte transfusions be different than RBC and in persons with granulocytopenia and gram-negative sepsis. platelet transfusions which are convincingly safe and effective. -

Current Challenges in Providing Good Leukapheresis Products for Manufacturing of CAR-T Cells for Patients with Relapsed/Refractory NHL Or ALL
cells Article Current Challenges in Providing Good Leukapheresis Products for Manufacturing of CAR-T Cells for Patients with Relapsed/Refractory NHL or ALL Felix Korell 1,*, Sascha Laier 2, Sandra Sauer 1, Kaya Veelken 1, Hannah Hennemann 1, Maria-Luisa Schubert 1, Tim Sauer 1, Petra Pavel 2, Carsten Mueller-Tidow 1, Peter Dreger 1, Michael Schmitt 1 and Anita Schmitt 1 1 Department of Internal Medicine V, University Hospital Heidelberg, 69120 Heidelberg, Germany; [email protected] (S.S.); [email protected] (K.V.); [email protected] (H.H.); [email protected] (M.-L.S.); [email protected] (T.S.); [email protected] (C.M.-T.); [email protected] (P.D.); [email protected] (M.S.); [email protected] (A.S.) 2 Institute of Clinical Transfusion Medicine and Cell Therapy (IKTZ), 89081 Heidelberg, Germany; [email protected] (S.L.); [email protected] (P.P.) * Correspondence: [email protected] Received: 9 April 2020; Accepted: 13 May 2020; Published: 15 May 2020 Abstract: Background: T lymphocyte collection through leukapheresis is an essential step for chimeric antigen receptor T (CAR-T) cell therapy. Timing of apheresis is challenging in heavily pretreated patients who suffer from rapid progressive disease and receive T cell impairing medication. Methods: A total of 75 unstimulated leukaphereses were analyzed including 45 aphereses in patients and 30 in healthy donors. Thereof, 41 adult patients with Non-Hodgkin’s lymphoma (85%) or acute lymphoblastic leukemia (15%) underwent leukapheresis for CAR-T cell production.