Education: Beyond the Medical Program Ann Jervie Sefton
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Brunei International Medical Journal
Brunei International Medical Journal OFFICIAL PUBLICATION OF THE MINISTRY OF HEALTH AND UNIVERSITI BRUNEI DARUSSALAM Volume 17 27 April 2021 (15 Ramadhan 1442H ) EVOLUTION OF UNDERGRADUATE MEDICAL EDUCATION IN BRUNEI DARUSSALAM. Divya Thirumalai RAJAM1, Fazean Irdayati IDRIS1, Nurolaini KIFLI1, Khadizah H. ABDUL- MUMIN1,2, Glenn HARDAKER3. 1PAPRSB Institute of Health Sciences, Universiti Brunei Darussalam, Jalan Tungku Link, BE1410, Brunei Darussalam. 2School of Nursing and Midwifery, La Trobe University, Bundoora, VIC 3086, Australia. 3Centre for Lifelong Learning, Universiti Brunei Darussalam, Jalan Tungku Link, BE1410, Brunei Darussalam. BACKGROUND The establishment of a localised medical programme will increase the number of future doctors for the country. Additionally, this will improve the quality of education, through locally trained doctors, leading to better health care for the population. Our article reports the developmental transitions of medical education in Brunei Darussalam, which are derived from our experiences as curriculum developers and observers. This is supported by internal university documented resources such as: reports, historical perspectives from lo- cal journals and university documents. The aim of this article is to highlight the insights of medical educa- tion and its developments in Brunei Darussalam. Medical education in Brunei began with overseas training of students who typically completed their higher secondary school education in the United Kingdom. This followed by a twinning programme, and later an articulated programme with partner medical schools (PMS) across the United Kingdom, Republic of Ireland, Australia, Canada and Hong Kong. The aim being to develop a ‘full-fledged’ medical programme in the near future. There have been further milestones achieved in the preparation of medical education, which will be reported in this article. -

2013 NSW Museum & Gallery Sector Census and Survey
2013 NSW Museum & Gallery Sector Census and Survey 43-51 Cowper Wharf Road September 2013 Woolloomooloo NSW 2011 w: www.mgnsw.org.au t: 61 2 9358 1760 Introduction • This report is presented in two parts: The 2013 NSW Museum & Gallery Sector Census and the 2013 NSW Small to Medium Museum & Gallery Survey. • The data for both studies was collected in the period February to May 2013. • This report presents the first comprehensive survey of the small to medium museum & gallery sector undertaken by Museums & Galleries NSW since 2008 • It is also the first comprehensive census of the museum & gallery sector undertaken since 1999. Images used by permission. Cover images L to R Glasshouse, Port Macquarie; Eden Killer Whale Museum , Eden; Australian Fossil and Mineral Museum, Bathurst; Lighting Ridge Museum Lightning Ridge; Hawkesbury Gallery, Windsor; Newcastle Museum , Newcastle; Bathurst Regional Gallery, Bathurst; Campbelltown arts Centre, Campbelltown, Armidale Aboriginal Keeping place and Cultural Centre, Armidale; Australian Centre for Photography, Paddington; Australian Country Music Hall of Fame, Tamworth; Powerhouse Museum, Tamworth 2 Table of contents Background 5 Objectives 6 Methodology 7 Definitions 9 2013 Museums and Gallery Sector Census Background 13 Results 15 Catergorisation by Practice 17 2013 Small to Medium Museums & Gallery Sector Survey Executive Summary 21 Results 27 Conclusions 75 Appendices 81 3 Acknowledgements Museums & Galleries NSW (M&G NSW) would like to acknowledge and thank: • The organisations and individuals -

Commonwealth of Australia Gazette! Published by the Australian Government Publishing Service
commonwealth of Australia Gazette! Published by the Australian Government Publishing Service No. G 32 Canberra, Tuesday, 16 August 1977 GENERAL CONTENTS AVAILABILrrY. The Gazette may be obtained by mail from: Notice to private advertisers 2 Mail Ordei Sales, Australian Government Publishing Scrvice, Proclamations 2 P.O. Box 84, Canberra, A.C.T. 2600 Legislation 2 or over the counter from Australian Government Pub- Customs 3 lishing Service Bookshops at: Government departments 6 Adelaide: 12 Pirie Street (Telephone 212 3646) Defence force appointments, etc. 16 Brisbane: ShO"'lo]p 42, The Valley rCentre , Fortitud" " e Valley Commonwealth teaching service 20 (Telephone 52 5526) Canberra: 113 London Circuii t (Telephon 547 7211) Bankruptcy Act 20 Hobart: 162 Macquariarie StreeSu t (Telephone 23 7151) Private advertisements 28 Melbourne: 347 Swanston Street (Telephone 66 33010) Tenders invited 31 Perth: 200 St George's Terrace (Telephone 22 4737) Contracts arranged 35 Sydney: 309 Pitt Street (Telephone 211 4755) Special Gazettes Nos S 158, S 159, S 160, S 161 and The Gazette is also available for perusal at official S 162 are attached Post Offices. Commonwealth Acts and Statutory Rules, Australian Commonwealth of Australia Gazette is published section- Capital Territory Ordinances and Regulations, and other ally in accordance with the arrangements set out below: Australian Government publications may also be pur- Public Service issues contain notices concerning admin- chased at these addresses. istrative matters, including examinations, vacancies, transfers and promotions within the Australian Public NOTICES FOR PUBLICATION and related corres- Service. These issues are published weekly at 10.30 a.m. pondence should be addressed to: on Thursday, and are sold at 95c each plus postage or Gazette Office, Australian Government Publishing on subscription of $58,00 (50 issues), $32.00 (25 issues), Service, P.O. -

Faculty of Law Handbook 1995 Faculty of Law Handbook 1995 ©The University of Sydney 1994 ISSN 1034-2656
The University of Sydney Faculty of Law Handbook 1995 Faculty of Law Handbook 1995 ©The University of Sydney 1994 ISSN 1034-2656 The address of the Law School is: The University of Sydney Law School 173-5 Phillip Street Sydney, N.S.W. 2000 Telephone (02) 232 5944 Document Exchange No: DX 983 Facsimile: (02) 221 5635 The address of the University is: The University of Sydney N.S.W. 2006 Telephone 351 2222 Setin 10 on 11.5 Palatino by the Publications Unit, The University of Sydney and printed in Australia by Printing Headquarters, Sydney. Text printed on 80gsm recycled bond, using recycled milk cartons. Welcome from the Dean iv Location of the Law School vi How to use the handbook vii 1. Staff 1 2. History of the Faculty of Law 3 3. Law courses 4 4. Undergraduate degree requirements 7 Resolutions of the Senate and the Faculty 7 5. Courses of study 12 6. Guide for law students and other Faculty information 24 The Law School Building 24 Guide for law students 24 Other Faculty information 29 Law Library 29 Sydney Law School Foundation 30 Sydney Law Review 30 Australian Centre for Environmental Law 30 Institute of Criminology 31 Centre for Plain Legal Language 31 Centre for Asian and Pacific Law 31 Faculty societies and student representation 32 Semester and vacation dates 33 The Allen Allen and Hemsley Visiting Fellowship 33 Undergraduate scholarships and prizes 34 7. Employment 36 Main Campus map 39 The legal profession in each jurisdiction was almost entirely self-regulating (and there was no doubt it was a profession, and not a mere 'occupation' or 'service industry'). -

Curriculum Vitae
1 University of Calgary Cumming School of Medicine CURRICULUM VITAE I: BIOGRAPHICAL DATA Dr. Aliya Kassam Room G028 Office of Postgraduate Medical Education 3330 Hospital Drive NW Calgary, Alberta Canada T2N 4N1 Phone: E-mail: [email protected] 403 210 7526 [email protected] II: ACADEMIC RECORD • Masters of Science (Biomedical Ethics) The University of Calgary (in progress since September 2016) • Doctorate of Philosophy (Health Service and Population Research) Institute of Psychiatry, King’s College London, 2010 • Masters of Science (Epidemiology) The University of Calgary, Alberta, 2005 • Bachelors of Science (Psychology) with First Class Honors The University of Calgary, Alberta, 2002 III: PROFESSIONAL AND TEACHING POSITIONS • Assistant Professor, Department of Community Health Sciences, University of Calgary (2011- Present) • Research Lead, Office of Postgraduate Medical Education (2011-Present) • Workshop Facilitator, Office of Postgraduate Medical Education (2011-Present) IV: EDUCATIONAL ACTIVITIES Graduate Courses • MDCH 621: Research Methods and Statistics in Medical Education (Fall 2015) 39 Hrs, 5 students (Instructor) • MDCH 626: Meta-Analysis and Systematic Reviews in Medical Education 2 (Winter 2014) 39 Hrs, 3 students (Instructor) • MDSC 755.34: Meta-Analysis and Systematic Reviews in Medical Education (Winter 2012) 39 Hrs, 6 students (Co-Instructor) Office of Health and Medical Education Scholarship & Medical Education Specialization Committee – Journal Club • Select articles and facilitate a 1hr journal club one -

Surgical News
Surgicalthe royaL austraLasian CoNewsLLege of surgeons May 2012 Vol: 12 No:10 Nov/Dec 2011 The College delivers Competency Training Standards, p28 The College of Surgeons of Australia and New Zealand Hearing the next generation Important initiative from the Foundation of Surgery p22 c ntents 12 Wattle & Fern – the New President’s Gown A lighter gown will make If you’re a doctor in presidential travelling easier 14 A Surgeon’s Treasure training interested in A treasured compass has a research placement, made it to the public domain would $25,000 or 16 International Development $50,000 help? Professor David Wood delivering the HPV Avant is delighted to announce the launch vaccine in PNG of the Avant Doctor in Training Research 18 Successful Scholar 42 Scholarships Program. Matthew Hong delivering REGULAR PAGES Each year we will award two full-time on efficiency 8 Surgical Snips 11 Poison’d Chalice scholarships to the value of $50,000 each and 22 Foundation for Surgery four part-time scholarships of $25,000 each. 13 Dr BB Gloved Important initiatives from 21 Ina Training Let us help turn your dream of that elusive generous donations 25 Law Commentary PD Workshops research placement into a reality. 28 Competency Training 36 27 The College delivers a world first on standards 25 Regional News 28 How New Zealand fares on As a recipient of grants in the past, I would encourage healthcare quality you to put as much detail as possible into the application, and safety it’s worth the time and effort to get it right. -

College of Human Medicine Records UA.15.13 This Finding Aid Was Produced Using Archivesspace on August 19, 2021
College of Human Medicine Records UA.15.13 This finding aid was produced using ArchivesSpace on August 19, 2021. Finding aid written in English. Describing Archives: A Content Standard Michigan State University Archives and Historical Collections Conrad Hall 943 Conrad Road, Room 101 East Lansing , MI 48824 [email protected] URL: http://archives.msu.edu/ College of Human Medicine Records UA.15.13 Table of Contents Summary Information .................................................................................................................. 3 Historical Note ............................................................................................................................. 3 Series Description ......................................................................................................................... 4 Series List ..................................................................................................................................... 6 Administrative Information .......................................................................................................... 8 Related Materials .......................................................................................................................... 8 Controlled Access Headings ......................................................................................................... 9 Collection Inventory ................................................................................................................... 10 Office of the Dean -
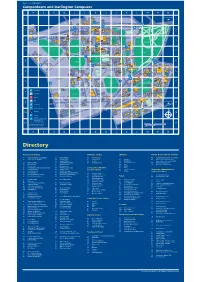
Camperdown and Darlington Campuses
Map Code: 0102_MAIN Camperdown and Darlington Campuses A BCDEFGHJKLMNO To Central Station Margaret 1 ARUNDEL STREETTelfer Laurel Tree 1 Building House ROSS STREETNo.1-3 KERRIDGE PLACE Ross Mackie ARUNDEL STREET WAY Street Selle Building BROAD House ROAD Footbridge UNIVERSITY PARRAMATTA AVENUE GATE LARKIN Theatre Edgeworth Botany LANE Baxter's 2 David Lawn Lodge 2 Medical Building Macleay Building Foundation J.R.A. McMillan STREET ROSS STREET Heydon-Laurence Holme Building Fisher Tennis Building Building GOSPER GATE AVENUE SPARKES Building Cottage Courts STREET R.D. Watt ROAD Great Hall Ross St. Building Building SCIENCE W Gate- LN AGRICULTURE EL Bank E O Information keepers S RUSSELL PLACE R McMaster Building P T Centre UNIVERSITY H Lodge Building J.D. E A R Wallace S Badham N I N Stewart AV Pharmacy E X S N Theatre Building E U ITI TUNN E Building V A Building S Round I E C R The H Evelyn D N 3 OO House ROAD 3 D L L O Quadrangle C A PLAC Williams Veterinary John Woolley S RE T King George VI GRAFF N EK N ERSITY Building Science E Building I LA ROA K TECHNOLOGY LANE N M Swimming Pool Conference I L E I Fisher G Brennan MacCallum F Griffith Taylor UNIV E Centre W Library R Building Building McMaster Annexe MacLaurin BARF University Oval MANNING ROAD Hall CITY R.M.C. Gunn No.2 Building Education St. John's Oval Old Building G ROAD Fisher Teachers' MANNIN Stack 4 College Manning 4 House Manning Education Squash Anderson Stuart Victoria Park H.K. -

5-7 December, Sydney, Australia
IRUG 13 5-7 December, Sydney, Australia 25 Years Supporting Cultural Heritage Science This conference is proudly funded by the NSW Government in association with ThermoFisher Scientific; Renishaw PLC; Sydney Analytical Vibrational Spectroscopy Core Research Facility, The University of Sydney; Agilent Technologies Australia Pty Ltd; Bruker Pty Ltd, Perkin Elmer Life and Analytical Sciences; and the John Morris Group. Conference Committee • Paula Dredge, Conference Convenor, Art Gallery of NSW • Suzanne Lomax, National Gallery of Art, Washington, USA • Boris Pretzel, (IRUG Chair for Europe & Africa), Victoria and Albert Museum, London • Beth Price, (IRUG Chair for North & South America), Philadelphia Museum of Art Scientific Review Committee • Marcello Picollo, (IRUG chair for Asia, Australia & Oceania) Institute of Applied Physics “Nello Carrara” Sesto Fiorentino, Italy • Danilo Bersani, University of Parma, Parma, Italy • Elizabeth Carter, Sydney Analytical, The University of Sydney, Australia • Silvia Centeno, The Metropolitan Museum of Art, New York, USA • Wim Fremout, Royal Institute for Cultural Heritage, Brussels, Belgium • Suzanne de Grout, Cultural Heritage Agency of the Netherlands, Amsterdam, The Netherlands • Kate Helwig, Canadian Conservation Institute, Ottawa, Canada • Suzanne Lomax, National Gallery of Art, Washington, USA • Richard Newman, Museum of Fine Arts, Boston, USA • Gillian Osmond, Queensland Art Gallery|Gallery of Modern Art, Brisbane, Australia • Catherine Patterson, Getty Conservation Institute, Los Angeles, USA -

Northwestern University Health Service ADMISSION HEALTH RECORD
Northwestern University Health Service ADMISSION HEALTH RECORD and Required Immunizations for NON-HEALTHCARE STUDENTS REQUIRED FOR ALL FULL-TIME AND HALF-TIME STUDENTS (DISTANCE LEARNERS COMPLETE THIS PAGE ONLY) Important Notes – Please read prior to completing this form. 1. Student should complete PARTS I, III, IV, and V of this form. If under 18, complete PART VI with parent. 2. Proof of immunization may be provided by the following: • Have your healthcare professional complete “PART II: REQUIRED IMMUNIZATIONS” (page 2). This page must be signed and dated by the healthcare professional to be valid. • Submit copies of your immunization record from your physician, former high school or university or other official record such as immigration paperwork. If laboratory titers are completed, copies of the lab result must be submitted. Submission of “PART II: REQUIRED IMMUNIZATIONS” is not required if you are submitting copies of records. 3. DEADLINES: This form and proof of immunizations should be submitted to the Evanston campus Health Service by: FALL entrants – July 1 Undergraduate and Graduate students (including Law, WINTER entrants – December 1 Kellogg and Continuing Studies) SPRING entrants – March 15 SUMMER entrants – May 1 All Half-time students and students accepted after the 30 days after date of acceptance term deadline above 4. Mail to: Northwestern University Health Service, Health Information Management Services, 633 Emerson St., Evanston, IL 60208 5. STUDENTS WHO FAIL TO SUBMIT THE COMPLETED ADMISSION HEALTH RECORD, INCLUDING PROOF OF IMMUNIZATIONS OR FAIL TO RECTIFY DEFICIENCIES WITHIN 30 DAYS AFTER THE START OF CLASSES WILL BE: • ASSESSED A NON-REFUNDABLE $100 LATE FEE AND • IN ACCORDANCE WITH ILLINOIS STATE LAW, BARRED FROM CLASS REGISTRATION FOR SUBSEQUENT TERMS UNTIL COMPLIANT. -

The University Archives – Record 2015
THE UNIVERSITY ARCHIVES 2015 Cover image: Students at Orientation Week with a Dalek, 1983. [G77/1/2360] Forest Stewardship Council (FSC®) is a globally recognised certification overseeing all fibre sourcing standards. This provides guarantees for the consumer that products are made of woodchips from well-managed forests, other controlled sources and reclaimed material with strict environmental, economical social standards. Record The University Archives 2015 edition University of Sydney Telephone Directory, n.d. [P123/1085] Contact us [email protected] 2684 2 9351 +61 Contents Archivist’s notes............................... 2 The pigeonhole waltz: Deflating innovation in wartime Australia ............................ 3 Aboriginal Photographs Research Project: The Generous Mobs .......................12 Conservatorium of Music centenary .......................................16 The Seymour Centre – 40 years in pictures ........................18 Sydney University Regiment ........... 20 Beyond 1914 update ........................21 Book review ................................... 24 Archives news ................................ 26 Selected Accession list.................... 31 General information ....................... 33 Archivist‘s notes With the centenary of WWI in 1914 and of ANZAC this year, not seen before. Our consultation with the communities war has again been a theme in the Archives activities will also enable wider research access to the images during 2015. Elizabeth Gillroy has written an account of where appropriate. a year’s achievements in the Beyond 1914 project. The impact of WWI on the University is explored through an 2015 marks another important centenary, that of the exhibition showing the way University men and women Sydney Conservatorium of Music. To mark this, the experienced, understood and responded to the war, Archives has made a digital copy of the exam results curated by Nyree Morrison, Archivist and Sara Hilder, from the Diploma of the State Conservatorium of Music, Rare Books Librarian. -

Vagrancy and the Victorians : the Social Construction of the Vagrant In
VAGRANCY AND THE VICTORIANS: THE SOCIAL CONSTRUCTION OF THE VAGRANT IN MELBOURNE, 1880-1907 SUSANNE ELIZABETH DAVIES RID THESiS, HISTORY DEPARTMENT, UNIVERSITY OF MELBOURNE, 1990 (This thesis does not exceed 100,000 words,) In Memory of my Father CONTENTS Page List of Figures 4 List of Illustrations 6 List of Abbreviations 9 Acknowledgements 10 Abstract 12 Introduction 15 Chapter One: A World of Difference 42 Chapter Two: The Evolution of the Vagrancy Laws 115 Chapter Three: Policing the Victorian Vagrancy Law 145 Chapter Four: Trial and Error 216 Chapter Five: Punishing and Reforming 274 Chapter Six: A System in Crisis $43 Chapter Seven: New Solutions for an Old Problem 397 Conclusion 450 Appendix One: Statistical Method 455 Appendix Two: Statistics relating to the Arrest and Imprisonment of Vagrants in Victoria, 1888-1907. 461 Appendix Three: Statistics relating to Vagrancy Cases heard by the Melbourne Court of Petty Sessions, 1 May 1888 - 30 April 1901. 468 Bibliography 478 4 FIGURES Page Figure 3.1: Vagrancy Arrests in Victoria, 1880-1907 161 Figure 3.2: Most Common Types of Arrests in Victoria, 1880-1905 162 Figure 3.3: Vagrancy Arrests as a Percentage of Total Arrests in Victoria, 1880-1907 163 Figure 3.4: '1 in 10' Sample - Vagrancy Cases heard by the MCPS, 1888-1901 167 Figure 3.5: '1 In 10' Sample - NVLMS/ILMS Cases as a Percentage of Total Vagrancy Cases, MCPS, 1888-1901 170 Figure 3.6: '1 in 10' Sample - Sex of Defendants in Vagrancy Cases, MCPS, 1888-1901 173 Figure 3.7: '1 in 10' Sample - Sex of Defendants in NVLMS/ILMS