Special Report Legislative Joint Auditing Committee
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Needs Improvement Priority Schools Arkansas Was Required to Identify A
Needs Improvement Priority Schools Arkansas was required to identify a number of lowest-performing schools equal to at least five percent of the state’s Title I schools. Arkansas had 803 Title I schools in 2011, requiring at least 40 Title I schools be identified among the schools identified as Needs Improvement Priority Schools. Arkansas identified 48 schools which included 41 Title I schools. The criteria for identification of Priority Schools set by USDE included identifying schools that were: • Among the lowest five percent of schools in the state based on proficiency and lack of progress of the “All Students” group, or • Title I participating or Title I eligible high schools with graduation rates less than 60% over a number of years, or • Tier I or Tier II SIG schools implementing a school intervention model. An added ranks method was used to identify Needs Improvement Priority Schools. The details of this method are provided on pages 87 – 88 of Arkansas’s approved ESEA Flexibility request. This method was used in previous years to identify the persistently lowest achieving schools under Section 1003(g) of the Elementary and Secondary Schools Act. This method considers the rank of school performance in math and literacy for a three-year period. The three-year average math and literacy performance for Priority Schools ranged from 7.9% of students scoring at or above the Proficient level to 47.7% of students scoring at or above the Proficient level. Interventions for Needs Improvement Priority Schools are detailed on pages 88 – 96 of Arkansas’s approved ESEA Flexibility request. -

2018-2019 Geographic Shortage Areas
2018-2019 Geographic Shortage Areas County School District School Bradley HERMITAGE SCHOOL DISTRICT HERMITAGE ELEMENTARY SCHOOL HERMITAGE HIGH SCHOOL HERMITAGE MIDDLE SCHOOL WARREN SCHOOL DISTRICT EASTSIDE PRIMARY SCHOOL EASTSIDE NEW VISION ELEM. CHARTER SCHOOL THOMAS C. BRUNSON ELEM. SCHOOL WARREN HIGH SCHOOL WARREN MIDDLE SCHOOL Chicot DERMOTT SCHOOL DISTRICT DERMOTT ELEMENTARY SCHOOL DERMOTT HIGH SCHOOL LAKESIDE SCHOOL DISTRICT EUDORA ELEMENTARY SCHOOL LAKESIDE HIGH SCHOOL LAKESIDE LOWER ELEM. SCHOOL LAKESIDE MIDDLE SCHOOL LAKESIDE UPPER ELEM. SCHOOL WONDER JR HIGH SCHOOL Columbia EMERSON-TAYLOR-BRADLEY SCHOOL DISTRICT EMERSON ELEMENTARY SCHOOL EMERSON HIGH SCHOOL TAYLOR ELEMENTARY SCHOOL TAYLOR HIGH SCHOOL MAGNOLIA SCHOOL DISTRICT CENTRAL ELEMENTARY SCHOOL EAST-WEST ELEMENTARY SCHOOL MAGNOLIA JUNIOR HIGH SCHOOL MAGNOLIA HIGH SCHOOL Desha DUMAS SCHOOL DISTRICT CENTRAL ELEMENTARY SCHOOL REED ELEMENTARY SCHOOL DUMAS JUNIOR HIGH SCHOOL DUMAS NEW TECH HIGH SCHOOL MCGEHEE SCHOOL DISTRICT MCGEHEE ELEMENTARY MCGEHEE JUNIOR HIGH SCHOOL MCGEHEE HIGH SCHOOL Fulton HIGHLAND SCHOOL DISTRICT CHEROKEE ELEMENTARY SCHOOL HIGHLAND MIDDLE SCHOOL HIGHLAND HIGH SCHOOL MAMMOTH SPRING SCHOOL DISTRICT MAMMOTH SPRING ELEMENTARY SCHOOL MAMMOTH SPRING HIGH SCHOOL SALEM SCHOOL DISTRICT SALEM ELEMENTARY SCHOOL SALEM HIGH SCHOOL VIOLA SCHOOL SISTRICT VIOLA ELEMENTARY SCHOOL VIOLA HIGH SCHOOL Izard IZARD COUNTY SCHOOL DISTRICT IZARD COUNTY ELEMENTARY IZARD COUNTY MIDDLE SCHOOL IZARD COUNTY HIGH SCHOOL Jackson JACKSON COUNTY SCHOOL DISTRICT TUCKERMAN ELEMENTARY SCHOOL SWIFTON MIDDLE SCHOOL TUCKERMAN HIGH SCHOOL NEWPORT SCHOOL DISTRICT NEWPORT HIGH SCHOOL NEWPORT ELEMENTARY SCHOOL NEWPORT JUNIOR HIGH SCHOOL CASTLEBERRY ELEM. SCHOOL GIBBS ALBRIGHT ELEM. SCHOOL Jefferson CORRECTIONS SCHOOL SYSTEM DELTA REGIONAL UNIT CENTRAL ARKANSAS CORRECTION CENTER CUMMINS UNIT DIAGNOSTIC UNIT EAST ARKANSAS REGIONAL UNIT GRIMES UNIT J. -
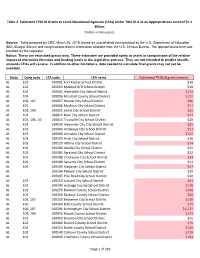
Page 1 of 283 State Cong Code LEA Code LEA Name Estimated FY2018
Table 2. Estimated FY2018 Grants to Local Educational Agencies (LEAs) Under Title IV-A at an Appropriations Level of $1.1 Billion Dollars in thousands Source: Table prepared by CRS, March 26, 2018, based on unpublished data provided by the U.S. Department of Education (ED), Budget Service and congressional district information available from the U.S. Census Bureau. The appropriations level was provided by the requester. Notice: These are estimated grants only. These estimates are provided solely to assist in comparisons of the relative impact of alternative formulas and funding levels in the legislative process. They are not intended to predict specific amounts LEAs will receive. In addition to other limitations, data needed to calculate final grants may not yet be available. State Cong code LEA code LEA name Estimated FY2018 grant amount AL 102 100001 Fort Rucker School District $10 AL 102 100003 Maxwell AFB School District $10 AL 104 100005 Albertville City School District $153 AL 104 100006 Marshall County School District $192 AL 106, 107 100007 Hoover City School District $86 AL 105 100008 Madison City School District $57 AL 103, 106 100011 Leeds City School District $32 AL 104 100012 Boaz City School District $41 AL 103, 106, 107 100013 Trussville City School District $20 AL 103 100030 Alexander City City School District $83 AL 102 100060 Andalusia City School District $51 AL 103 100090 Anniston City School District $122 AL 104 100100 Arab City School District $26 AL 105 100120 Athens City School District $54 AL 104 100180 Attalla -

Fiscal Year 2019 Title I Grants to Local Educational Agencies
Fiscal Year 2019 Title I Grants to Local Educational Agencies - ARKANSAS No data No data No data LEA ID District FY 2019 Title I Allocation 502250 Alma School District 855,489 502280 Alpena School District 200,288 502430 Arkadelphia School District 558,833 502550 Armorel School District 51,498 502580 Ashdown School District 398,186 502610 Atkins Public Schools 274,620 502670 Augusta School District 413,481 502700 Bald Knob School District 428,355 502730 Barton-Lexa School District 330,577 500019 Batesville School District 830,687 502790 Bauxite School District 122,154 502820 Bay School District 103,639 500032 Bearden School District 176,904 502880 Beebe School District 700,709 502960 Benton School District 614,742 503060 Bentonville Public Schools 1,257,260 503090 Bergman School District 191,993 503150 Berryville Public Schools 683,880 503240 Bismarck Public Schools 270,880 503300 Blevins School District 246,791 503320 Blytheville School District 1,693,324 503450 Booneville School District 437,623 503480 Bradford School District 146,328 503630 Brinkley School District 457,300 503640 Brookland School District 236,838 503690 Bryant Public Schools 963,907 503710 Buffalo Island Central School District 206,112 503750 Cabot Public Schools 1,440,757 503770 Caddo Hills School District 320,212 503840 Calico Rock School District 124,876 506060 Camden Fairview School District 1,257,554 503960 Carlisle School District 116,122 504050 Cave City School District 594,290 500070 Cedar Ridge School District 260,804 504080 Cedarville School District 375,871 -

County District School Date of Clinic Location of Clinic (Address) If Not at the School
County District School Date of Clinic Location of clinic (address) if not at the school PULASKI ACADEMIC PLUS SCHOOL DISTRICT ACADEMICS PLUS TBA PULASKI ACADEMIC PLUS SCHOOL DISTRICT ACADEMICS PLUS TBA CRAWFORD ALMA SCHOOL DISTRICT ALMA HIGH SCHOOL 10/28/10 CRAWFORD ALMA SCHOOL DISTRICT ALMA INTERMEDIATE SCHOOL 11/1/10 CRAWFORD ALMA SCHOOL DISTRICT ALMA MIDDLE SCHOOL 11/4/10 CRAWFORD ALMA SCHOOL DISTRICT ALMA PRIMARY SCHOOL 10/25/10 BOONE ALPENA SCHOOL DISTRICT ALPENA ELEMENTARY SCHOOL 11/30/10 BOONE ALPENA SCHOOL DISTRICT ALPENA HIGH SCHOOL 11/30/10 GARLAND AR MATH & SCIENCE SCHOOL AR MATH & SCIENCE SCHOOL 10/13/10 PULASKI ARK. SCHOOL FOR THE BLIND ARK. SCHOOL FOR THE BLIND ELEM 10/20/10 PULASKI ARK. SCHOOL FOR THE BLIND ARK. SCHOOL FOR THE BLIND H.S. 10/20/10 PULASKI ARK. SCHOOL FOR THE DEAF ARK. SCHOOL FOR THE DEAF ELEM. 10/20/10 PULASKI ARK. SCHOOL FOR THE DEAF ARK. SCHOOL FOR THE DEAF H.S. 10/20/10 CLARK ARKADELPHIA SCHOOL DISTRICT ARKADELPHIA HIGH SCHOOL 11/17/10 CLARK ARKADELPHIA SCHOOL DISTRICT CENTRAL PRIMARY SCHOOL 11/12/10 CLARK ARKADELPHIA SCHOOL DISTRICT GOZA MIDDLE SCHOOL 11/12/10 CLARK ARKADELPHIA SCHOOL DISTRICT LOUISA PERRITT PRIMARY 11/10/10 County District School Date of Clinic Location of clinic (address) if not at the school CLARK ARKADELPHIA SCHOOL DISTRICT PEAKE ELEMENTARY SCHOOL 11/10/10 PULASKI ARKANSAS VIRTUAL SCHOOL ARKANSAS VIRTUAL ELEM SCHOOL TBA PULASKI ARKANSAS VIRTUAL SCHOOL ARKANSAS VIRTUAL MIDDLE SCHOOL TBA MISSISSIPPI ARMOREL SCHOOL DISTRICT ARMOREL ELEMENTARY SCHOOL 10/21/10 MISSISSIPPI ARMOREL SCHOOL DISTRICT ARMOREL HIGH SCHOOL 10/21/10 LITTLE RIVER ASHDOWN SCHOOL DISTRICT ASHDOWN HIGH SCHOOL 10/6/10 LITTLE RIVER ASHDOWN SCHOOL DISTRICT ASHDOWN JUNIOR HIGH SCHOOL 10/6/10 LITTLE RIVER ASHDOWN SCHOOL DISTRICT C. -

Post-School Outcomes 6-Year Sampling Plan for 2014-2019
Arkansas’ Indicator 14: Post-School Outcomes 6-Year Sampling Plan for 2014-2019 Table 1: ADM Strata ADM # Districts ADM Strata 20,000 and over 2 6 10,000 to 19,999 5 5 5,000 to 9,999 8 4 2,500 to 4,999 30 3 1,000 to 2,499 73 2 1 to 999 142 1 N = 260 Table 2: Randomization Summary Counts per Year and ADM Strata ADM Strata by Count of LEA Sampling Year 1 2 3 4 5 6 Grand Total 1 23 12 5 2 0 2 44 2 23 12 5 2 1 43 3 23 13 5 1 1 43 4 24 12 5 1 1 43 5 24 12 5 1 1 43 6 25 12 5 1 1 44 Grand Total 142 73 30 8 5 2 260 Post-school Outcomes Survey Districts by Sampling Year 1 (2013-14) and ADM Strata; 2012-13 Leavers LEA Number District Name Sampling Year ADM Strata 0403000 GENTRY SCHOOL DISTRICT 1 2 0440700 BENTON COUNTY SCHOOL OF ARTS 1 1 0601000 HERMITAGE SCHOOL DISTRICT 1 1 0803000 GREEN FOREST SCHOOL DISTRICT 1 2 1104000 PIGGOTT SCHOOL DISTRICT 1 1 1305000 CLEVELAND COUNTY SCHOOL DISTRICT 1 1 1603000 BROOKLAND SCHOOL DISTRICT 1 2 1608000 JONESBORO SCHOOL DISTRICT 1 4 1611000 NETTLETON SCHOOL DISTRICT 1 3 1613000 RIVERSIDE SCHOOL DISTRICT 1 1 2002000 FORDYCE SCHOOL DISTRICT 1 1 2307000 VILONIA SCHOOL DISTRICT 1 3 2501000 MAMMOTH SPRING SCHOOL DISTRICT 1 1 2602000 FOUNTAIN LAKE SCHOOL DISTRICT 1 2 2703000 POYEN SCHOOL DISTRICT 1 1 2808000 PARAGOULD SCHOOL DISTRICT 1 3 3003000 MAGNET COVE SCHOOL DIST. -

Archived: 2003 Title I Grants to Local Educational Agencies
Fiscal Year 2003 Title I Grants to Local Educational Agencies - ARKANSAS Maximum Required Expenditures For Choice-Related Maximum Per-Child Transportation Expenditure For FY 2003 Title I And Supplemental Supplemental LEA ID District Allocation* Educational Services** Educational Services*** 502220 ACORN SCHOOL DISTRICT 111,372 22,274 1,484.95 502250 ALMA SCHOOL DISTRICT 476,788 95,358 1,018.78 502280 ALPENA SCHOOL DISTRICT 101,081 20,216 981.37 502310 ALREAD SCHOOL DISTRICT 31,439 6,288 1,209.19 502330 ALTHEIMER UNIFIED SCHOOL DISTRICT 347,874 69,575 1,391.50 502370 ALTUSDENNING SCHOOL DISTRICT 95,375 19,075 1,083.81 502430 ARKADELPHIA SCHOOLS 477,982 95,596 1,023.52 502460 ARKANSAS CITY SCHOOL DISTRICT 69,979 13,996 1,428.14 502550 ARMOREL SCHOOL DISTRICT 32,381 6,476 2,158.74 502580 ASHDOWN SCHOOL DISTRICT 339,810 67,962 1,020.45 502610 ATKINS PUBLIC SCHOOLS 264,995 52,999 996.22 502670 AUGUSTA SCHOOL DISTRICT 323,955 64,791 1,439.80 502700 BALD KNOB SCHOOL DISTRICT 374,234 74,847 1,281.62 502730 BARTONLEXA SCHOOL DISTRICT 146,897 29,379 1,335.43 500019 BATESVILLE SCHOOL DISTRICT 460,391 92,078 1,101.41 502790 BAUXITE SCHOOL DISTRICT 82,210 16,442 813.97 502820 BAY SCHOOL DISTRICT 120,284 24,057 1,366.86 500032 BEARDEN SCHOOL DISTRICT 178,759 35,752 1,004.27 502880 BEEBE SCHOOL DISTRICT 311,394 62,279 958.14 502960 BENTON SCHOOL DISTRICT 605,920 121,184 1,439.24 503060 BENTONVILLE PUBLIC SCHOOLS 722,409 144,482 972.29 503090 BERGMAN SCHOOL DISTRICT 150,444 30,089 1,002.96 503150 BERRYVILLE PUBLIC SCHOOLS 398,785 79,757 1,001.97 503210 -

AGENDA STATE BOARD of EDUCATION June 10, 2016 Arkansas Department of Education ADE Auditorium 9:00 AM
AGENDA STATE BOARD OF EDUCATION June 10, 2016 Arkansas Department of Education ADE Auditorium 9:00 AM Back Print Reports Report-1 Chair's Report Presenter: Chair Report-2 Commissioner's Report Presenter: Commissioner Johnny Key Report-3 2015 ATOY Report The 2015 Arkansas Teacher of the Year will present a component of her professional development project. Presenter: 2015 Arkansas Teacher of the Year Ms. Ouida Newton Report-4 2014-2015 Grade Inflation Report Presenter: Elbert Harvey Report-5 ForwARd Arkansas Report Presenter: Susan Harriman, Executive Director of ForwARd Report-6 Learning Services Report This information is provided to keep the State Board of Education apprised of the Department's work activities associated with college and career readiness. Presenter: Stacy Smith Report-7 Computer Science Report This information is provided to keep the State Board of Education apprised of the Department's work activities associated with Computer Science. Presenter: Anthony Owen Arkansas Social Studies Standards “A people without the knowledge of their past history, origin and culture is like a tree without roots.” – Marcus Garvey. The importance of the Social Studies Curriculum Frameworks to Arkansas K-12 education cannot be overlooked. Parents and educators readily agree on the importance of developing reading, writing and math skills. They even agree in our technological society on the importance of teaching science, but what about social studies? It is through the study of social studies that students become aware of the world around them and how that world directly impacts their lives. By learning about economics, civics and government, geography and history, students are able to develop core beliefs and values, an understanding of how the past has shaped the present and will shape the future, and the interconnectedness of the content areas. -

(STEP) 2014-2015 Geographic Shortage Area
State Teacher Education Program (STEP) 2014-2015 Geographic Shortage Area County School District School Bradley HERMITAGE SCHOOL DISTRICT HERMITAGE ELEMENTARY SCHOOL HERMITAGE HIGH SCHOOL HERMITAGE MIDDLE SCHOOL WARREN SCHOOL DISTRICT EASTSIDE PRIMARY SCHOOL THOMAS C. BRUNSON ELEM. SCHOOL WARREN HIGH SCHOOL WARREN MIDDLE SCHOOL Chicot DERMOTT SCHOOL DISTRICT DERMOTT ELEMENTARY SCHOOL DERMOTT HIGH SCHOOL LAKESIDE SCHOOL DISTRICT EUDORA ELEMENTARY SCHOOL LAKESIDE HIGH SCHOOL LAKESIDE LOWER ELEM. SCHOOL LAKESIDE MIDDLE SCHOOL LAKESIDE UPPER ELEM. SCHOOL Clay CORNING SCHOOL DISTRICT CENTRAL ELEMENTARY SCHOOL CORNING HIGH SCHOOL PARK ELEMENTARY SCHOOL PIGGOTT SCHOOL DISTRICT PIGGOTT ELEMENTARY SCHOOL PIGGOTT HIGH SCHOOL RECTOR SCHOOL DISTRICT RECTOR ELEMENTARY SCHOOL RECTOR HIGH SCHOOL County School District School WONDER JR HIGH SCHOOL Dallas FORDYCE SCHOOL DISTRICT FORDYCE ELEMENTARY SCHOOLS FORDYCE MIDDLE SCHOOL FORDYCE HIGH SCHOOL Desha DUMAS SCHOOL DISTRICT CENTRAL ELEMENTARY SCHOOL DUMAS HIGH SCHOOL DUMAS JUNIOR HIGH SCHOOL REED ELEMENTARY SCHOOL MCGEHEE SCHOOL DISTRICT MCGEHEE ELEMENTARY SCHOOL MCGEHEE HIGH SCHOOL Izard CALICO ROCK SCHOOL DISTRICT CALICO ROCK ELEMENTARY SCHOOL CALICO ROCK HIGH SCHOOL IZARD COUNTY CONSOLIDATED SCHOOL IZARD COUNTY ELEMENTARY DISTRICT IZARD COUNTY MIDDLE SCHOOL IZARD COUNTY HIGH SCHOOL MELBOURNE SCHOOL DISTRICT MOUNT PLEASANT ELEMENTARY SCHOOL MELBOURNE ELEMENTARY SCHOOL State Teacher Education Program (STEP) 2014-2015 Geographic Shortage Area MELBOURNE HIGH SCHOOL Jefferson CORRECTIONS SCHOOL SYSTEM DELTA -

ATRS 10502 Annual Report
Comprehensive Annual Financial Report A Component Unit of the State of Arkansas Prepared by the staff of Arkansas Teacher Retirement System Linda Parsons Chair–Board of Trustees Copies of this report are available from: Arkansas Teacher Retirement System 1400 West Third Street Little Rock, Arkansas 72201 501.682.1517 or 1.800.666.2877 website: atrs.state.ar.us ARKANSAS TEACHER RETIREMENT SYSTEM ANNUAL REPORT FOR FISCAL YEAR ENDED JUNE 30, 2002 2002 Comprehensive Annual Financial Report A Component Unit of the State of Arkansas 3 ARKANSAS TEACHER RETIREMENT SYSTEM ANNUAL REPORT FOR FISCAL YEAR ENDED JUNE 30, 2002 INTRODUCTORY SECTION Letter of Transmittal ..................................................................................................................................................................... 4 Board of Trustees .......................................................................................................................................................................... 7 Professional Consultants .............................................................................................................................................................. 8 Organizational Chart and Administrative Staff .................................................................................................................... 10 FINANCIAL SECTION Basic Financial Statements: Statement of Plan Net Assets ................................................................................................................................................. -

United States Court of Appeals for the EIGHTH CIRCUIT ______
United States Court of Appeals FOR THE EIGHTH CIRCUIT __________ No. 03-3088 __________ Little Rock School District, * * Plaintiff, * * Servicemaster Management Services; * Blytheville School District; Bryant * School District; Fort Smith School * District; West Memphis School District; * Altus-Denning School District; * Ashdown School District; Barton-Lexa * Appeals from the United States School District; Batesville School * District Court for the District; Biggers-Reyno School District; * Eastern District of Arkansas. Black Rock School District; Bright Star * School District; Brinkley School * District; Centerpoint School District; * Clarendon School District; Cotton Plant * School District; Cutter Morning Star * School District; Dewitt School District; * Dollarway School District; Foreman * School District; Fountain Lake School * District; Gillett School District; Glen * Rose School District; Guy-Perkins * School District; Hoxie School District; * Jonesboro School District; Kirby School* District; Lavaca School District; * Lewisville School District; Magazine * School District; Malvern School * District; Mammoth Spring School * District; Manila School District; * Maynard School District; Oden School * District; Ozark School District; * Appellate Case: 03-3404 Page: 1 Date Filed: 08/05/2004 Entry ID: 1796194 Plainview-Rover School District; * Pocahontas School District; Prairie * Grove School District; South Conway * School District; Spring Hill School * District; Stamps School District; * Stephens School District; Turrell School* District; -

*JSE607* a Bill
Stricken language would be deleted from and underlined language would be added to present law. 1 State of Arkansas Call Item 13 2 85th General Assembly A Bill 3 First Extraordinary Session, 2006 SENATE BILL 5 4 5 By: Senators Argue, Broadway 6 By: Representatives Elliott, Cook, Mahony 7 8 9 For An Act To Be Entitled 10 AN ACT TO BE KNOWN AS THE EDUCATIONAL ADEQUACY 11 ACT OF 2006; TO ENSURE A GENERAL, SUITABLE AND 12 EFFICIENT SYSTEM OF PUBLIC EDUCATION FOR STUDENTS 13 BY ADRESSING ISSUES RAISED BY THE ARKANSAS 14 SUPREME COURT; TO AMEND THE MINIMUM TEACHER 15 COMPENSATION SCHEDULE; TO INCREASE THE FOUNDATION 16 FUNDING PROVIDED UNDER THE PUBLIC SCHOOL FUNDING 17 ACT OF 2003; TO CLARIFY THAT THE NINE PERCENT 18 (9%) OF FOUNDATION FUNDING DEDICATED TO PAYMENT 19 OF UTILITIES AND COSTS OF MAINTENANCE, REPAIR, 20 AND RENOVATION ACTIVITIES APPLIES TO ALL PUBLIC 21 SCHOOL FACILITIES; TO LIMIT THE EMPLOYER 22 CONTRIBUTION RATE FOR TEACHER RETIREMENT; AND FOR 23 OTHER PURPOSES. 24 25 Subtitle 26 THE EDUCATIONAL ADEQUACY ACT OF 2006. 27 28 29 BE IT ENACTED BY THE GENERAL ASSEMBLY OF THE STATE OF ARKANSAS: 30 31 SECTION 1. Arkansas Code Title 6, Chapter 10, Subchapter 1 is amended 32 to add an additional section to read as follows: 33 6-10-120. Adequate and equitable public education system. 34 (a) The General Assembly finds: 35 (1) It is the duty of the state of Arkansas to provide a 36 general, suitable, and efficient system of free public schools to the *JSE607* 03-31-2006 16:12 JSE607 SB5 1 children of the state, under Ark.