Informed Refusal by James W
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Congressional Record—House H2331
March 26, 2003 CONGRESSIONAL RECORD — HOUSE H2331 postal carriers, the service responds to more There was no objection. Mr. DAVIS of Illinois. Mr. Speaker, I than 1,000 postal-related assaults and credit Mr. DUNCAN. Mr. Speaker, I yield yield myself such time as I might con- threats, 75,000 complaints of consumer mail myself such time as I may consume. sume. fraud, and it arrests 12,000 criminal suspects Mr. Speaker, it is a real honor and (Mr. DAVIS of Illinois asked and was for mail-related crimes each year. privilege for me to bring this par- given permission to revise and extend Today, my colleagues have a special oppor- ticular legislation to the floor at this his remarks.) tunity to honor the entire United States Postal time because Floyd Spence was a close, Mr. DAVIS of Illinois. Mr. Speaker, Service, by naming a postal facility after one personal friend of mine and one of the H.R. 917, which names a postal facility of their own heroes. With the passage of H.R. greatest Members this body has ever located at 1830 South Lake Drive in 825, The House of Representatives will re- seen. I had the privilege of traveling Lexington, South Carolina, after Floyd name the Moraine Valley, Illinois Post Office several different places with Congress- Spence, was introduced on February 25, the Michael J. Healy Post Office. man Spence and working with him on 2003, by the gentleman from South Finally, I would like to recognize Joan many different pieces of legislation. Carolina (Mr. WILSON). Healy, Michael’s mother, his brother David, H.R. -

Man of the House
Walkthrough - - (7.30AM) breakfast talk with mom, for earn some points. - (8.30AM) Talk with Sis (Ashley) twice, and open new option. - For now MC only need talk with Veronica in the Kitchen (9.00 - 10.00AM) and open new option. - In the beggin MC need go in his Room and in the computer and have Online Course, do it till have the message that MC –have mastered completely - (8.00-12.00AM) - MC need go in the pizzeria and Work (12.00 -15.00AM) – doing this, MC can open new options, and get some itens. - (15.00PM) Teaching Sis in Her Bedroom, twice. - (18.00PM) Dinner with everyone. - (19.00) Talk with Mom in the kitchen, for earn some points. - (19.00 – 19.30PM) See movies with Sis. - (21,00PM) MC giving for Mom the -rub foot-, after –Try to move- (MC need give her some Wine) -Buy in the Supermarket - - - (22.00PM) MC need give Goodnight for Sis (Ashley) - (6.00AM) Go to the rooftop, see and talk with Mom. - - The Rooftop - - Advice: Walking or travel with bus, taxi or even going with Veronica’s car, is a random event but MC can find some itens and some advertising that open Pizzeria, Casino and maybe others location (in the next version). - And for open Health Club, MC need talk with Mom in the rooftop (6.00AM) - In the morning new event (7.00AM) MC need sleep and wake up at 7.00Am (before sleep need heard the phone in the Mom's bedroom, 22.00PM Mom and Aunt talking) - - Ashley - (8.30AM) - Breakfast - (15.00PM) - Teaching (Twice, till options are open) - (19.00PM) - See movies (When Horror movie are open, new option in the night) (19.30PM when MC talk with Mom) - (21.00PM) - Bathroom (New scenes with Sis) – You can alternate with Mom’s scenes – one day Sis, another Mom. -

San Diego Health & Exercise Survey
THIS SURVEY SHOULD BE COMPLETELY FILLED OUT BY THE FOLLOWING PERSON, WHO MUST BE I' AT LEAST 18 YEARS OLD: D The lady of the house. If the lady of D The man of the house. If the man of the house is not available, then the the house is not available, then the man of the house should fill it out. lady of the house should 'fill it out. o Check here if you want a free 2 week pass to Family Fitness Center. Please read each question carefully and answer it to the best of your ability. Do not spend too much time on any question. Your answers will be kept in strictest confidence. SAN DIEGO HEALTH & EXERCISE SURVEY 1. How is your health? (PLEASE CHECK ONE) VERY GOOD_l GOOD 2 AVERAGE _3 POOR _4 VERY POOR_5 2. Do you need to limit your physical activity because of an illness, NO 1 injury or handicap? YES, BECAUSE OF TEMPORARY ILLNESS _ 2 (CHECK ONE) YES, BECAUSE OF LONG-TERM ILLNESS _ 3 YES, BECAUSE OF TEMPORARY INJURY _ 4 YES, BECAUSE OF LONG-TERM INJURY . OR HANDICAP. _ 5 3. Are you being treated by a doctor for any medical condition? NO _1 If yes, please explain _ YES _2 4. Have either of your parents ever had a heart attack or stroke before NO 1 they were 55 years old? YES _2 DON'T KNOW _3 5. How often do you eat the following foods? (MARK ONE NUMBER FOR EACH ITEM) Never or Several Few Times About Once Times Few Times Almost a Year a Month a Month a Week ~ 1. -

Congressional Record-·House
1900. CONGRESSIONAL RECORD-·HOUSE. 189 By Mr. HOFFECKER: A bill (H. R.12507) granting an increase By Mr. ROBINSON of Indiana: Petition of Advance Grange, of pension to Ezekiel Dawson-to the Committee on Invalid Pen No. 2100, Patrons of Husbandry, of Fremont, Ind., favoring pure sions. food legislation-to the Committee on Agriculture. By Mr. RANSDELL: A bill (H. R. 12508) for the relief of John By Mr. RYAN of New York: Petition of Rev. George B. New McDonnell-to the Committee on Military Affairs. comb and others, of Buffalo, N. Y., in favor of the anti-polygamy By Mr. KLEBERG: A bill (H. R. 12509) for the relief of Maria. amendment to the Constitution-to the Committee on the Judi Thornton, residuary legatee of Richard Miller, deceased-to the ciary. Committee on War Claims. By Mr. SHACKLEFORD: Petition of the estate of John W. Livesay, deceased, of Missouri, for reference of war claim to the Court of Claims-to the Committee on War Claims. PETITIONS, ETC. By Mr. SIBL.EY: Petitions of druggists of Warren County, Pa., Under clause 1 of Rule XXII, the following petitions and papers for the repeal of the special tax on proprietary medicines-to the were laid on the Clerk's desk and referred as follows: Committee on Ways and Means. By Mr. ACHESON: Petition of J. D. Moffat and other citizens Also, petition of citizens of Warren, Pa., in favor of the anti of Washington County, Pa., in favor of an amendment to the polygamy amendment to the Constitution-to the Committee on Constitution against polygamy-to the Committee on the Judi the Judiciary. -

Hartford Public Library DVD Title List
Hartford Public Library DVD Title List # 24 Season 1 (7 Discs) 2 Family Movies: Family Time: Adventures 24 Season 2 (7 Discs) of Gallant Bess & The Pied Piper of 24 Season 3 (7 Discs) Hamelin 24 Season 4 (7 Discs) 3:10 to Yuma 24 Season 5 (7 Discs) 30 Minutes or Less 24 Season 6 (7 Discs) 300 24 Season 7 (6 Discs) 3-Way 24 Season 8 (6 Discs) 4 Cult Horror Movies (2 Discs) 24: Redemption 2 Discs 4 Film Favorites: The Matrix Collection- 27 Dresses (4 Discs) 40 Year Old Virgin, The 4 Movies With Soul 50 Icons of Comedy 4 Peliculas! Accion Exploxiva VI (2 Discs) 150 Cartoon Classics (4 Discs) 400 Years of the Telescope 5 Action Movies A 5 Great Movies Rated G A.I. Artificial Intelligence (2 Discs) 5th Wave, The A.R.C.H.I.E. 6 Family Movies(2 Discs) Abduction 8 Family Movies (2 Discs) About Schmidt 8 Mile Abraham Lincoln Vampire Hunter 10 Bible Stories for the Whole Family Absolute Power 10 Minute Solution: Pilates Accountant, The 10 Movie Adventure Pack (2 Discs) Act of Valor 10,000 BC Action Films (2 Discs) 102 Minutes That Changed America Action Pack Volume 6 10th Kingdom, The (3 Discs) Adventure of Sherlock Holmes’ Smarter 11:14 Brother, The 12 Angry Men Adventures in Babysitting 12 Years a Slave Adventures in Zambezia 13 Hours Adventures of Elmo in Grouchland, The 13 Towns of Huron County, The: A 150 Year Adventures of Ichabod and Mr. Toad Heritage Adventures of Mickey Matson and the 16 Blocks Copperhead Treasure, The 17th Annual Lane Automotive Car Show Adventures of Milo and Otis, The 2005 Adventures of Pepper & Paula, The 20 Movie -

Hartford Public Library DVD Title List
Hartford Public Library DVD Title List # 20 Wild Westerns: Marshals & Gunman 2 Days in the Valley (2 Discs) 2 Family Movies: Family Time: Adventures 24 Season 1 (7 Discs) of Gallant Bess & The Pied Piper of 24 Season 2 (7 Discs) Hamelin 24 Season 3 (7 Discs) 3:10 to Yuma 24 Season 4 (7 Discs) 30 Minutes or Less 24 Season 5 (7 Discs) 300 24 Season 6 (7 Discs) 3-Way 24 Season 7 (6 Discs) 4 Cult Horror Movies (2 Discs) 24 Season 8 (6 Discs) 4 Film Favorites: The Matrix Collection- 24: Redemption 2 Discs (4 Discs) 27 Dresses 4 Movies With Soul 40 Year Old Virgin, The 400 Years of the Telescope 50 Icons of Comedy 5 Action Movies 150 Cartoon Classics (4 Discs) 5 Great Movies Rated G 1917 5th Wave, The 1961 U.S. Figure Skating Championships 6 Family Movies (2 Discs) 8 Family Movies (2 Discs) A 8 Mile A.I. Artificial Intelligence (2 Discs) 10 Bible Stories for the Whole Family A.R.C.H.I.E. 10 Minute Solution: Pilates Abandon 10 Movie Adventure Pack (2 Discs) Abduction 10,000 BC About Schmidt 102 Minutes That Changed America Abraham Lincoln Vampire Hunter 10th Kingdom, The (3 Discs) Absolute Power 11:14 Accountant, The 12 Angry Men Act of Valor 12 Years a Slave Action Films (2 Discs) 13 Ghosts of Scooby-Doo, The: The Action Pack Volume 6 complete series (2 Discs) Addams Family, The 13 Hours Adventure of Sherlock Holmes’ Smarter 13 Towns of Huron County, The: A 150 Year Brother, The Heritage Adventures in Babysitting 16 Blocks Adventures in Zambezia 17th Annual Lane Automotive Car Show Adventures of Dally & Spanky 2005 Adventures of Elmo in Grouchland, The 20 Movie Star Films Adventures of Huck Finn, The Hartford Public Library DVD Title List Adventures of Ichabod and Mr. -

THE MOVIE CHANNEL Schedule
THE MOVIE CHANNEL Schedule November 1, 2012 7:10 AM: Shall We Dance? (PG) 9:10 AM: Jean Claude Van Damme: Behind Closed Doors: Dubai (TV14) 9:55 AM: My Father The Hero (PG) 11:25 AM: Cop And A Half (PG) 1:00 PM: Dragonslayer (2011) (TVMA) 2:15 PM: Blues Brothers 2000 (PG13) 4:20 PM: Bob Funk (R) 6:10 PM: The Tempest (PG13) 8:00 PM: Real Steel (PG13) 10:10 PM: Big Money Rustlas (R) 11:45 PM: Death Racers (R) November 2, 2012 1:20 AM: Hobo With a Shotgun (TVMA) 2:50 AM: I Went Down (R) 4:40 AM: The Thin Blue Line (TV14) 6:30 AM: Barnyard (PG) 8:00 AM: Straight Talk (PG) 9:30 AM: Checking Out (R) 11:05 AM: Daddy and Them (R) 12:50 PM: Beaches (PG13) 3:00 PM: The Heavy (R) 4:45 PM: Momentum (R) 6:25 PM: Runner, The (1999) (R) 8:00 PM: Source Code (PG13) 9:35 PM: Flesh Wounds (R) 11:00 PM: Elephant White (R) November 3, 2012 12:35 AM: Maximum Velocity (PG13) 2:10 AM: Bikini A Go Go (TVMA) 3:30 AM: Twelve (R) 5:05 AM: The Skulls III (PG13) 7:00 AM: Red (PG13) 9:00 AM: Saved! (PG13) 12:30 PM: Barry Munday (R) 2:05 PM: Aces N' Eights (TVPG) 3:35 PM: Cracks (R) 5:30 PM: Paycheck (PG13) 7:30 PM: Our Idiot Brother (R) 9:00 PM: Mother's Day (R) 11:00 PM: Road Kill (R) November 4, 2012 12:35 AM: Mother's Day (R) 1:30 AM: Road Kill (R) 3:00 AM: Messages Deleted (TVMA) 4:35 AM: King of the Avenue (R) 7:30 AM: The King's Speech (R) 9:30 AM: Suburban Girl (PG13) 11:10 AM: The Ref (R) 12:50 PM: Other Woman, The (2011) (R) 2:35 PM: My 5 Wives (R) 4:15 PM: The Story Of Us (R) 5:50 PM: Blues Brothers 2000 (PG13) 8:00 PM: Real Steel (PG13) 10:15 PM: The Tempest -

A Study of Home Moviemaking As Visual Communication
Studies in Visual Communication Volume 2 Issue 2 Fall 1975 Article 5 1975 Cinéma Naïveté: A Study of Home Moviemaking as Visual Communication Richard Chalfen Recommended Citation Chalfen, R. (1975). Cinéma Naïveté: A Study of Home Moviemaking as Visual Communication. 2 (2), 87-103. Retrieved from https://repository.upenn.edu/svc/vol2/iss2/5 This paper is posted at ScholarlyCommons. https://repository.upenn.edu/svc/vol2/iss2/5 For more information, please contact [email protected]. Cinéma Naïveté: A Study of Home Moviemaking as Visual Communication This contents is available in Studies in Visual Communication: https://repository.upenn.edu/svc/vol2/iss2/5 CINEMA NA.iVETE: A STUDY OF HOME MOVIEMAKING AS VISUAL COMMUNICATION 1 RICHARD CHALFEN In comparison with other types of films, home movies are stereotypically !hought of as films of everyday life, of com monplace family activities, of life around the house, and the like. At face value, such films seem to be extremely rich in Those home movies on TV_:_~ore bombshells to come? ethnographic data, and as such, should be valued by social scientists as native views of initimate realities. 2 One objective Figure 7 of this paper is to examine this proposition as data about the problematic relationship between the symbolic reality of the home movie medium, the stated cultural and technical pre behavior organized within social and cultural contexts. Be scriptions about its use, and the reality of everyday life. A ~aviors surrounding filmmaking are understood as promoted, related objective is to better understand the notion of l1mited, or restricted primarily by social norms rather than as symbolic manipulation as it applies to one genre of film com limitations primarily imposed by psychological or technical munication-namely, home movies. -

CONGRESSIONAL RECORD—HOUSE April 9, 1997
April 9, 1997 CONGRESSIONAL RECORD Ð HOUSE H1347 have refused to produce a budget, re- not only will increase take-home on both sides of the aisle have said over fused to hold hearings on campaign fi- wages, it will help us in our effort to the 1-minute period this morning, they nance reform, refused to schedule ac- decrease the deficit and deal with our want to see us begin moving ahead tion on kids' health care, and refused national debt problem. with our work. We want to do that. We to schedule a vote on any of the Demo- Mr. Speaker, I urge my colleagues if want to take up these measures that cratic education initiatives: how to get they have not already joined in the co- could be considered under suspension of kids to school and have working fami- sponsorship of my measure, which in- the rules. lies be able to afford that. cludes my colleague, the gentlewoman Mr. Speaker, this rule itself is non- The Republican majority would like from Missouri, KAREN MCCARTHY, the controversial. It requires consultation to continue to do nothing. So be it. But gentleman from Virginia, Mr. MORAN, with the minority, so I hope very much get out of the way so others can talk the gentleman from Florida, and sev- that we can move as expeditiously as about an agenda that helps working eral other people who are involved in possible to pass this. families in this country. this in a bipartisan way, I urge Mem- Mr. Speaker, I reserve the balance of f bers to cosponsor it. -

Home of the Month
HOME OF THE MONTH A dedicated 15-seat theater serves Capacious media servers, simple software and intuitive touchpanels as the ultimate A/V wonderland for the homeowners and their create an amazing entertainment network for a family of four. three children. A wireless AMX by Lisa Montgomery, photography by Jeff Allen touchpanel displays movies avail- able on their Kaleidescape media server, cues up the Runco 1080p What’s the best way to unwind after a long, hard week? For the owners of this projector and Parasound surround- 12,000-square-foot Nantucket, MA, vacation home, nothing soothes away stress sound system, and dims the Lutron better than kicking back with a few relaxing tunes. A favorite choice on a Friday RadioRA controlled light fixtures. night after a tough commute might be songs from jazz vocalist Diana Krall. On a lazy Sunday afternoon, the preferred medley might be something completely different, like a compilation of R&B classics from Earth, Wind & Fire. 84 EH ■ January 2008 An Entertainment FREE-FOR-ALL ARCTIC TALE TM, ® AND © 2007 PARAMOUNT PICTURES. ALL RIGHTS RESERVED. ElectronicHouse.com 85 HOME OF THE MONTH His-and-hers office spaces offer plenty of flexibility for the family. The lady of the house can sum- mon a piece of music to her workspace from an AMX touch- panel, while her husband uses his own touchpanel to call up a favorites page that lists his top cable and satellite TV stations. A simple touch puts the chosen station onto the 60-inch NEC plasma TV. A trio of Bohlender- Graebener Radia speakers were mounted horizontally to comple- ment the lines of the cabinet. -
John F. Kennedy: Public Perception and Campaign Strategy in 1946 By
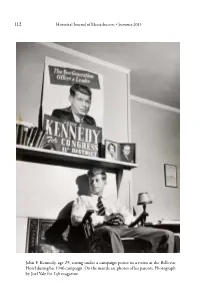
112 Historical Journal of Massachusetts • Summer 2013 John F. Kennedy, age 29, sitting under a campaign poster in a room at the Bellevue Hotel during his 1946 campaign. On the mantle are photos of his parents. Photograph by Joel Yale for Life magazine. 113 John F. Kennedy: Public Perception and Campaign Strategy in 1946 SETH M. RIDINGER Editor’s Introduction: Boston politics in the 1940s were replete with backroom dealmaking, cigar smoke, and corruption; it was a world of insiders. In 1946, John F. Kennedy took on this hostile realm in a bid for the United States Congress. Kennedy’s victory set his trajectory firmly on the path toward the White House. However, it was not Kennedy’s unlimited coffers that propelled him into office; instead, it was his ability to shape public perception and outwork the other candidates, his innovations in campaign strategy, and his appeal as a naval war hero that swept him to electoral victory. The author argues that although money is an important factor in politics, it was not the determining factor in Kennedy’s 1946 success. The author’s research draws on the extensive oral history collections of the John F. Kennedy Library and Museum. The Oral History Program’s goal is to “collect, preserve, and make available interviews conducted with individuals who were in some way associated with John F. Kennedy and his legacy.” The collection comprises more than 1,700 interviews; interviewees include prominent public figures as well as private individuals who played distinct roles in Kennedy’s life, career, Historical Journal of Massachusetts, Vol. -

January 6 9:00 Am Service
Shabbat Shalom! 27501 Fairmount Boulevard Pepper Pike, Ohio 44124 Tel: 216-831-6555 Fax: 216-831-4599 www.bnaijeshurun.org Condolence/Event Cancellation Tel: 216-831-6556 Welcome to the David J. & Ruth A. Moskowitz Sanctuary on behalf of Rabbi Stephen Weiss, Rabbi Hal Rudin-Luria, Cantor Aaron Shifman, Education Engagement Rabbi Josh Foster, Rabbi Emeritus Stanley J. Schachter, President Shelley Scher and Executive Director Jay Ross. Our Mission is “To ensure the flourishing of Jewish life through educational, social and Conservative religious experiences in a warm and dynamic community.” Parashat Shemot ,«un§a« January 5/6, 2018 - 19 Tevet 5778 Hertz Etz Hayim Verse Rishon 213 326 Ex. 3:1 - 3:6 Sheni 214 328 3:7 - 3:10 Shlishi 215 329 3:11 - 3:15 Revi’i 216 331 3:16 - 3:22 Chamishi 218 332 4:1 - 4:5 Shishi 218 333 4:6 - 4:9 Shevi’i 219 334 4:10 - 4:17 Maftir 219 334 4:14 - 4:17 Haftarah 225 343 Isaiah 27:6 - 28:13; 29:22 - 29:23 Thank you to our Torah readers: Terry Amon, Naomi Shapiro, Monica Sass, Rachel Cohen, Rylan Polster, Mara Cohen and Jody Katzner. Thank you to Jody Katzner for chanting the Haftorah. DAILY MINYAN MONDAY - THURSDAY 7:00 am & 7:30 am & 6:00 pm FRIDAY 7:00 am & 7:30 am & 6:00 pm (unless otherwise noted) SATURDAY 9:00 am & 6:00 pm SUNDAY & HOLIDAYS 8:00 am & 6:00 pm FRIDAY Mazal tov to everyone who is celebrating a birthday this month! Thank you to our greeter, Dale Nash.