Kpvsobm! Pg! Tupnbupmphz
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thessaloniki Hotels Directory 2020-21
THESSALONIKI HOTELS ASSOCIATION 1 9 1 4 - 2014 THESSALONIKI HOTELS DIRECTORY 2020-21 take a stroll. in peace. this is Thessaloniki. Walk! Don’t rush. Walk. Thessaloniki’s chilled-out attitude Thessaloniki shimmers is your passport to true relaxation: admire the with its own brand magnificence of the sea while drinking a coffee of easy-living spirit -all at one of the local cafés; catch impro jazz sounds you need to do is let or alternative beats at the hip downtown bars; sample yourself go and have fun. delicious Mediterranean dishes at one of the many An impressive mix picturesque tavernas... Just take your time and enjoy! of gastronomic cultures, a rich and varied nightlife, a great history to explore on every step of the way. Do not forget to try the wines! LIVELY NIGHTLIFE City-break lovers will be amazed by the great choice of nightlife on offer, mixing traditions, cultures, the past and the present. Traditional Greek ALL KINDS music halls, live music bars, buzzing new venues showcasing the best yeah! OF TUNES live acts every night of the week, whatever you’re after, you are sure to Cozy little coffee shops and bars find it here. Have a late-night seafood feast at Perea and Aretsou by in the city centre and the Ladadika the seaside, indulge in an oriental sweet at Ano Poli (the old citadel) or port district welcome their guests wander down to Valaoritou street -the city’s latest hotspot- where you can with all kinds of tunes –from jazz to hang out with people from all walks of life till the small hours. -

Office Markets in Europe Strong
S2 2020 MARKET INSIGHT REPORT THESSALONIKI MARKET REPORT 2020 has been characterised as the year of the Covid-19 pandemic. Global markets and economies have struggled throughout with Lockdowns and Restrictions that have blown away all macro economic goals and indicators. 2021 is already seen as the first step to recovery. GDP in Volume Terms/Seasonally adjusted figures MACRO FIGURES (q-o-q) and (y-o-y) European and Global figures imply that economic impact of Covid-19 has lead the economies to unprecedent economic crisis. Forecasts of 2021 are optimistic and most economists agree that we are headed to a recovery fuelled by the massive vaccination programs across the globe. Greek Economy S2 Overview Greece had to face the outcomes of a ten year economic crisis, which officially came to an end in 2019. Before yet witnessing Source: Elstat the increases in macro figures, Covid-19 EUROPEAN COMISSION FORECASTS has trashed all hope for positive macro ECONOMIC 2019 2020 2021 2022 numbers in 2020. Recession in 2020 due to INDICATORS the pandemic has hit Greece hard and the unavoidable lock down measures and GDP (%) 1,9 -10 5 3,5 restrictions have worn out the Greek Inflation (%) 0,8 -1,3 0,9 1,3 economy. In 2020 the fall in GDP was at Unemployement 10% with the published figures so far. The 17,3 18 17,5 16,7 slow down and shrinking of the economy is (%) Gvnt Balance evident in all relevant indicators The 1,5 -6,9 -6,3 -3,4 economy is expected to bounce back in Sheet (% GDP) 2021 and get into even more optimistic Gross Public Debt 180,5 207,2 200,7 194,8 numbers by 2022. -

Thessaloniki Perfecture
SKOPIA - BEOGRAD SOFIA BU a MONI TIMIOU PRODROMOU YU Iriniko TO SOFIASOFIA BU Amoudia Kataskinossis Ag. Markos V Karperi Divouni Skotoussa Antigonia Melenikitsio Kato Metohi Hionohori Idomeni 3,5 Metamorfossi Ag. Kiriaki 5 Ano Hristos Milohori Anagenissi 3 8 3,5 5 Kalindria Fiska Kato Hristos3,5 3 Iliofoto 1,5 3,5 Ag. Andonios Nea Tiroloi Inoussa Pontoiraklia 6 5 4 3,5 Ag. Pnevma 3 Himaros V 1 3 Hamilo Evzoni 3,5 8 Lefkonas 5 Plagia 5 Gerakari Spourgitis 7 3 1 Meg. Sterna 3 2,5 2,5 1 Ag. Ioanis 2 0,5 1 Dogani 3,5 Himadio 1 Kala Dendra 3 2 Neo Souli Em. Papas Soultogianeika 3 3,5 4 7 Melissourgio 2 3 Plagia 4,5 Herso 3 Triada 2 Zevgolatio Vamvakia 1,5 4 5 5 4 Pondokerassia 4 3,5 Fanos 2,5 2 Kiladio Kokinia Parohthio 2 SERES 7 6 1,5 Kastro 7 2 2,5 Metala Anastassia Koromilia 4 5,5 3 0,5 Eleftherohori Efkarpia 1 2 4 Mikro Dassos 5 Mihalitsi Kalolivado Metaxohori 1 Mitroussi 4 Provatas 2 Monovrissi 1 4 Dafnoudi Platonia Iliolousto 3 3 Kato Mitroussi 5,5 6,5 Hrisso 2,5 5 5 3,5 Monoklissia 4,5 3 16 6 Ano Kamila Neohori 3 7 10 6,5 Strimoniko 3,5 Anavrito 7 Krinos Pentapoli Ag. Hristoforos N. Pefkodassos 5,5 Terpilos 5 2 12 Valtoudi Plagiohori 2 ZIHNI Stavrohori Xirovrissi 2 3 1 17,5 2,5 3 Latomio 4,5 3,5 2 Dipotamos 4,5 Livadohori N. -

The Full Guide Halkidiki, Greece
Halkidiki, Greece Halkidiki, the Full Guide Halkidiki, Greece Halkidiki inside your dreams… They say that no other place in Greece can boast beaches like those of Halkidiki. Still, the region stands for far more than beaches. Halkidiki is the perfect combination of the reviving Mediterranean light, the unspoiled land, the lively communities and a glorious past to explore. Add the local gastronomy, the religious traditions, the openness and hospitality of the people, the wide range of activities and lifestyles; flavour with the soothing scent of the pine-trees and there you are! -the already desirable has turned to the simply irresistible. Halkidiki is literally sculpted by nature forces to balance earth and sea. Three peninsulas, fjiord-like bays with emerald beaches and coves, imposing mountains -the stage for thriving life and civilizations in every form -like the thousand- year old monastic state of Mt. Athos, a unique World Heritage Site! Myth has it that the great greek philosopher Aristotle, who was born here and spent his life away from his native land -if only to teach the young Alexander the Great- never ceased to praise the honey of Halkidiki! Was it a metaphor or he actually meant the renowned honey we can cherish today? There is no way to know but who cares! You too will love the land and the rich produce of its gardens and orchards. It is truly a place of dreams… and your dream has only just begun… HALKIDIKI FACTS GENERAL INFORMATION Location: Halkidiki peninsula is located near Pets: There are pet friendly hotels, the city of Thessaloniki and it is a part of camping facilities and studios. -

5.4 Waste Water Treatment
CONTENTS Message from President ............................................... 4 Message from CEO ....................................................... 5 Information on how the annual report was prepared .. 6 1. THE COMPANY IN 2019 1.1 At a glance ................................................................ 8 2. THE COMPANY 2.1 Background ............................................................. 12 2.2 Objects ...................................................................14 2.3 Vision – Objective – Implementation .....................15 2.4 Major investment projects under way .................... 17 2.5 Major events in 2019................................................18 2.6 Pricing policy ......................................................... 20 2.7 Research, Development & GIS ................................ 21 3. COMPANY STRUCTURE 3.1 Organisational Chart .............................................. 26 3.2 The Board of Directors .......................................... 28 3.3 The General Manager and Managers ................... 30 3.4 Corporate Governance Statement ........................ 32 3.5 Legislative Framework ........................................... 33 4. CORPORATE SOCIAL RESPONSIBILITY 4.1 Employee education - support ............................... 36 4.2 Customer service ................................................... 37 4.3 Ecological practices .............................................. 38 4.4 Relations with the local community ...................... 38 4.5 Human Resources ................................................. -

Whelton, H. L., Lewis, J., Halstead, P., Isaakidou, V., Triantaphyllou, S., Tzevelekidi, V., Kotsakis, K., & Evershed, R. P
Whelton, H. L., Lewis, J., Halstead, P., Isaakidou, V., Triantaphyllou, S., Tzevelekidi, V., Kotsakis, K., & Evershed, R. P. (2018). Strontium isotope evidence for human mobility in the Neolithic of northern Greece. Journal of Archaeological Science: Reports, 20, 768-774. https://doi.org/10.1016/j.jasrep.2018.06.020 Peer reviewed version License (if available): CC BY-NC-ND Link to published version (if available): 10.1016/j.jasrep.2018.06.020 Link to publication record in Explore Bristol Research PDF-document This is the author accepted manuscript (AAM). The final published version (version of record) is available online via Elsevier at https://doi.org/10.1016/j.jasrep.2018.06.020 . Please refer to any applicable terms of use of the publisher. University of Bristol - Explore Bristol Research General rights This document is made available in accordance with publisher policies. Please cite only the published version using the reference above. Full terms of use are available: http://www.bristol.ac.uk/red/research-policy/pure/user-guides/ebr-terms/ 1 Strontium isotope evidence for human mobility in the Neolithic of northern Greece 2 3 Whelton, H. L. a, Lewis, J.b, Halstead, P.c, Isaakidou, V.d, Triantaphyllou, S.e, Tzevelekidi, V.f, 4 Kotsakis, K.e, Evershed, R. P.a 5 6 aOrganic Geochemistry Unit, School of Chemistry, University of Bristol, Cantock’s Close, Bristol BS8 7 1TS, UK 8 bBristol Isotope Group, School of Earth Sciences, University of Bristol, Wills Memorial Building, 9 Queen’s Road, Bristol, BS8 1RJ, UK 10 cDepartment of Archaeology, University of Sheffield, Sheffield, UK 11 dSchool of Archaeology, University of Oxford, Oxford, UK 12 eSchool of History & Archaeology, Aristotle University of Thessaloniki, Thessaloniki 54124, Greece 13 fEphorate of Antiquities of West Attica, Pireus and Islands, Ministry of Culture and Sports, Athens, 14 Greece 15 16 Abstract 17 18 Strontium isotope ratios are widely used in archaeology to differentiate between local and non-local 19 populations. -
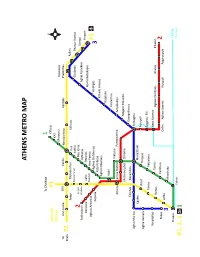
Athens Metro Map
ATHENS METRO MAP To Chalkida 1 Suburban P1 Kifissia Railway ΚΑΤ Maroussi Doukissis To Ano Liosia SΚΑ Iraklio Neratziotissa Pentelis Plakentias Kiato P2 Zefyri Metamorfosi Irini Kifissias Pallini Kato Acharne Iraklio Chalandri Peania- Kantza 2 Pyrgos Nea Ionia Koropi Anthoupoli Vasilissis Pefkakia Aghia Paraskevi Airport Peristeri Aghioi Perissos Nomismatokopio Anargyroi Aghios Antonios Ano Patisia Aghios Eleftherios Holargos Sepolia P3 Kato Patissia 3 Ethniki Amyna Aghios Nikolaos Katehaki Attiki Panormou Viktoria Athens Larissa Station Panepistimio Ampelokipi Metaxourghio Omonia Megaro Mousikis Eleonas Keramikos Evangelismos Aghia Marina Syntagma Egaleo Monastiraki Rouf Acropoli Aghia Varvara Thisseio Syggrou- FIX Tavros Petralona Korydallos Neos Kosmos Rentis Tavros Aghios Dimitrios Alimos Elliniko Nikea Kallithea 2 Lefka Dafni Aghios Ioannis Ilioupoli Argyroupoli 3 Moschato Piraeus Tram Faliro to Voula P1, 2, 3 1 THESSALONIKI BUS LINES N.S. MAKEDONIAAIRPORT STATHMOS LAOGRAFIKO MOUSEIO ARRIVALS AGORA BALTA KAMARA FALIRO KRIKELA ZOGRAFOU KOLOMVOU ΑG. FOTINI ASTYNOMIA KTEL BUSES MAKEDONIAAIRPORT THESSALONIKIS PERIF. ENOTITA DEPARTURES PAN. MAKEDONIAS MEGARO25is MOUSIKIS MARTIOU PLATEIA ARISTOTELOUS DIMARCHIAKO MEGARO LINE 01Χ COSMOS KTEL BUSES MICHANOURGION.S. OSE STATHMOS AGHION PANTON KOLOMVOU ALKAZAR KAMARA AHEPA IPPOKRATIO 25is MARTIOU AGHIAS ANASTASIASMEDITERRANEAN LINE 45 ANTIGONIDON ΚΤΕL CHALKIDIKIS PLATEIA ARISTOTELOUS OTHER BASIC BUS LINES NUMBER TERMINALS AREAS COVERED NUMBER TERMINALS AREAS COVERED EFKARPIA T.S.- SKLAVENITIS- 01 PAPAGEORGIOU HOSP.- EFEDROUPOLI- POLICHNI- PAVLOU MELA - EVOSMOS- EL. KORDELIO- DENDROPOTAMOS- MENEMENI 19 EL. KORDELIO- N.S. STATHMOS ELEFTHERIO KORDELIO- EVOSMOS- DENDROPOTAMOS- MENEMENI- Ν.N. RAILWAY STATION KTEL 02 Α.S. ΙΚΕΑ- KTEL MAKEDONIA NEA KRINI- FINIKAS- DEPO/ KARAMPOURNAKI- VOULGARI- EGNATIA- VARDARIS 21 EVOSMOS- ARISTOTELOUS ΕVOSMOS- AMPELOKIPI- VARDARIS- DIKASTIRION SQ. NEA KRINI- ARERTSOU- KALAMARIA- KARAMPOURNAKI- V. -

Curriculum Vitae of Nikos Moschovos
CURRICULUM VITAE, NIKOS MOSCHOVOS JOURNALIST, EDITOR, AUTHOR, RADIO PRODUCER/PRESENTER, LECTURER, MEMBER OF ESIEMTH Name: Nikos Moschovos Address in Canada: 1613-24 Wellesley St W Toronto, ON, M4Y 2X6 (416)-361-9605 (home) (416)-844-9663 (emergency) Address in Greece: 21, Pafsania Postal code: 54352 City: Thessaloniki Country: Greece Telephone number: 6944-18.17.72 and 2310-286.962 Email: [email protected], [email protected] Website: www.edu.typologos.com and www.typologos.com RECENT WORK EXPERIENCE HIGHLIGHTS: From January 2013 to December 2013: Ex- Owner of the former - firm NMOS- Nikolaos Moschovos, Journalism- Internet lectures of Journalism, promotion, communications, advertisement, news presentation and developing ideas. From 2008 to March 2012: Journalist, Director North Greece office, newspaper “Espresso”, Imerisios Typos S.A. and NEP Publishing S.A., Science, Police, life-style reporting. From October 2008 to September 2009: Journalist, newspaper “Sfina”, KYKA Publishing S.A., column “Edo Thessaloniki” (“Here Thessaloniki”). Open topic reportage. 1/4/1998 up to September 2008: Journalist, Primary North Greece correspondent and Director from 2004, newspaper “Apogevmatini”, “Apogevmatini S.A.”. Columns “Edo Thessaloniki” ( “Here Thessaloniki”) and “Perifereia Ellados” (“District of Greece”). Writing about culture, arts, medical and free- theme issues. 2006: Lecturer, state college IEK, Epanomi, Thessaloniki, at the Department of Journalism and Imaging. Courses: International and television reporting. Nikolaos Moschovos C.V., Page 1 1995 - 1997: Presenter, editor, and producer. Radio show “Vimata stous dromous tis tehnis” (“Steps on the road of art”) at a local radio station “Radio-Foni tis Toumpas” (“Voice of Toumba”) in Thessaloniki. DETAILED TEACHING – WORK EXPERIENCE: 2011- present: Founder, Experimental-volunteer (non-profit) news portal www.typologos.com on knowledge, science and art. -

List of Bank Branches by Branch Name 31/12/2014
LIST OF BANK BRANCHES BY BRANCH NAME 31/12/2014 PIRAEUS BANK S.A. BRANCH NAMEHEBIC AREA ADDRESS TELEPHONE NUMBER / FAX 1866 SQUARE, CHANIA0172758 CHANIA 70, Chatzimichali Giannari str., 731 35 CHANIA tel.: 2821029100, fax: 2821050710 25TH AVGOUSTOU, HERAKLIO0172751 HERAKLEIO 39, 25th Avgoustou str., 712 02 HERAKLEIO tel.: 2810247610, fax: 2810228324 3RD SEPTEMVRIOU, OMONIA 0172039 ATHENS 28, 3rd Septemvriou & Kapodistriou str., 104 32 ATHENS BRANCH tel.: 2105205100, fax: 2105235138 62 MARTIRON HERAKLIOU0172761 HERAKLEIO 97, 62 Martiron Ave. & 1, Dionysiou Fragiadaki str., 713 04 HERAKLEIO tel.: 2810264330, fax: 2810255997 ABELONAS0171393 AMPELONAS 1, Goltsiou & 5, Thermopylon str., 404 00 AMPELONAS tel.: 2492306000, fax: 2492031402 ACHARNON0172058 ATHENS 421, Acharnon str., 111 43 ATHENS tel.: 2102588070, fax: 2102520490 ACHARNON STR.0171592 ATHENS 205, Acharnon & Niovis str.s., 104 46 ATHENS tel.: 2166008310, fax: 2168003817 AEGINA BRANCH0172124 AEGINA Dimokratias Coastal Ave. & Leonardou Lada str., 180 10 AEGINA tel.: 2297029890, fax: 2297028882 AG. ACHILLIOU0171563 LARISSA 146, El. Venizelou str., 412 22 LARISSA tel.: 2416000160, fax: 2416007111 AG. ANTONIOU, PERISTERI0172048 PERISTERI 33, Ethnarchou Makariou str., 121 31 PERISTERI tel.: 2105783020, fax: 2105773224 AG. DIMITRIOS0171555 AGIOS DIMITRIOS 266, Vouliagmenis Ave., 173 43 AGIOS DIMITRIOS tel.: 2160005020, fax: 2109765714 AG. DIMITRIOU0172085 AGIOS DIMITRIOS 173, Ag. Dimitriou Ave., 173 43 AGIOS DIMITRIOS tel.: 2109758170, fax: 2109764036 AG. DIMITRIOU, THESSALONIKI0172203 THESSALONIKI 77, Ag. Dimitriou str., 546 33 THESSALONIKI tel.: 2310254860, fax: 2310223843 AG. IOANNI RENTI SQ. BRANCH0172136 AG. I. RENTIS 4, Konstantinou Palaiologou str., Ag. I. Renti sq., 182 33 AG. I. RENTIS tel.: 2104838120, fax: 2104832389 AG. IOANNOU, AG. PARASKEVI0172010 AGIA PARASKEVI 40, Ag. Ioannou str., 153 42 AGIA PARASKEVI tel.: 2106085800, fax: 2106011128 AG. -

Evolution of Water Supply Infrastructures of Thessaloniki City, Hellas, Through Centuries
European Water 58: 465-472, 2017. © 2017 E.W. Publications Evolution of water supply infrastructures of Thessaloniki city, Hellas, through centuries S. Yannopoulos1, A. Kaiafa-Saropoulou2*, E. Gala-Georgila3 and E. Eleftheriadou4 1 School of Rural and Surveying Engineering, Faculty of Engineering, Aristotle University of Thessaloniki, GR 54124 Thessaloniki, Greece 2 School of Architecture, Aristotle University, 54124 Thessaloniki, Greece, Cherianon 7, Kalamaria, GR 55133, Thessaloniki, Greece 3 Delfon 195, GR 54655 Thessaloniki, Greece 4 Department of Environment and Hydroeconomy of Thessaloniki, District of Central Macedonia, 26th Oktovriou 64, GR 54627 Thessaloniki, Greece * e-mail: [email protected] Abstract: Thessaloniki city, in the east core of Thermaic gulf, has been continuously inhabited for about 2330 years. The choice of its founding at this specific location is very much attributed to the high availability of water in the wider region. However, the development of Thessaloniki in a big city and the simultaneous increasing population, created an increased need for water, which could not be covered by the water of the wells. Until the 19th century, water needs were met with cisterns, water channels, fountains and water towers in combination with the wells. Moreover, the city was also equipped with large scale and of high expertise water supply projects, which were exploiting the region’s water resources in four different places and were transferring water inside the walls. These water transfer works were associated with water distribution systems, with pipes located beneath roads or following the contour lines. Also, people who lived in the Hellenistic, Roman, Byzantine, Ottoman and newer Hellenic periods gave their own perspective in the problems related to water supply in the city. -

UC Berkeley UC Berkeley Electronic Theses and Dissertations
UC Berkeley UC Berkeley Electronic Theses and Dissertations Title Synoikism, Urbanization, and Empire in the Early Hellenistic Period Permalink https://escholarship.org/uc/item/5np6p9qx Author Boehm, Ryan Anthony Publication Date 2011 Peer reviewed|Thesis/dissertation eScholarship.org Powered by the California Digital Library University of California Synoikism, Urbanization, and Empire in the Early Hellenistic Period by Ryan Anthony Boehm A dissertation submitted in partial satisfaction of the requirements for the degree of Doctor of Philosophy in Ancient History and Mediterranean Archaeology in the Graduate Division of the University of California, Berkeley Committee in charge: Professor Emily Mackil, Chair Professor Erich Gruen Professor Mark Griffith Spring 2011 Copyright © Ryan Anthony Boehm, 2011 ABSTRACT SYNOIKISM, URBANIZATION, AND EMPIRE IN THE EARLY HELLENISTIC PERIOD by Ryan Anthony Boehm Doctor of Philosophy in Ancient History and Mediterranean Archaeology University of California, Berkeley Professor Emily Mackil, Chair This dissertation, entitled “Synoikism, Urbanization, and Empire in the Early Hellenistic Period,” seeks to present a new approach to understanding the dynamic interaction between imperial powers and cities following the Macedonian conquest of Greece and Asia Minor. Rather than constructing a political narrative of the period, I focus on the role of reshaping urban centers and regional landscapes in the creation of empire in Greece and western Asia Minor. This period was marked by the rapid creation of new cities, major settlement and demographic shifts, and the reorganization, consolidation, or destruction of existing settlements and the urbanization of previously under- exploited regions. I analyze the complexities of this phenomenon across four frameworks: shifting settlement patterns, the regional and royal economy, civic religion, and the articulation of a new order in architectural and urban space. -

Study on Adequate Urban Housing for Refugees
STUDY ON ADEQUATE URBAN HOUSING FOR REFUGEES Thessaloniki, Greece Avertissement In this proposition we use « refugee » as the generic term to describe the people fleeing to Greece, whether or not they had completed the legal process of claiming asylum. The vast majority of people arriving in Greece are fleeing countries in war and therefore are « internationally recognized as "refugees" with access to assistance from States, UNHCR, and other organizations ». However, a smaller proportion is from elsewhere and for many of these individuals, the term 'migrant' would be more appropriate. Authors : Simon Deprez & Eléonore Labattut www.etc-projects.eu [email protected] NRC > Study on Adequate Urban Housing for Refugees in Thessaloniki !2 Abbreviations ARSIS Association for the Social Support of Youth CRS Catholic Relief Services EU European Union GAS Greek Asylum Service GDP Gross Domestic Product MoMP Ministry of Migration Policy MdM Médecins du Monde NFI Non Food Items NRC Norwegian Refugee Council OEK Autonomous Workers' Housing Organization OSM Open Street Map POC Person of Concern PRAXIS Programs Of Development, Social Support And Medical Cooperation RHU Refugee Housing Unit UNHCR United Nations High Commissioner for Refugees WAHA Woman And Health Alliance International NRC > Study on Adequate Urban Housing for Refugees in Thessaloniki !3 Table of Content Table of Content 4 Executive Summary 6 Methodology 8 PART I CONTEXT ANALYSIS 11 1. Refugee situation in North Greece 12 1.1. Context 12 1.2. Situation in the camps 12 2. Existing housing strategies in Thessaloniki and the surrounding area 13 2.1. UNHCR and partners 13 2.2. Other Housing Projects 17 2.3.