Frequently Asked Questions: ACA Enrollment (Updated: May 2021) OVERVIEW
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tax Season Special Enrollment Periods
Updated February 25, 2015 Tax Season Special Enrollment Periods The second open enrollment period (OEP) under the Affordable Care Act ended on February 15, with more than 11.4 million people enrolled in coverage through the Federal and state Marketplaces.1 Attention now turns to the 2014 tax season. Many tax filers who were uninsured for all or part of 2014 are learning for the first time that they must pay a penalty, and have missed the opportunity to enroll in 2015 coverage. A recent analysis by the Urban Institute finds significant percentages of uninsured adults who may be subject to the penalty have heard little or nothing about it, did not expect or did not know if they would have to pay the penalty, and did not know about the Marketplace enrollment deadlines, if they had heard of the Marketplaces at all.2 The Federal government and eight State-based Marketplaces – in California, Connecticut, Kentucky, Maryland, Minnesota, New York, Washington and Vermont – have already announced plans to establish a Special Enrollment Period (SEP) to permit individuals subject to the tax penalty to enroll in 2015 coverage outside of this year’s OEP, thereby minimizing the penalty they could incur when filing their 2015 taxes.3 The Affordable Care Act requires that all Marketplaces provide initial and annual open enrollment periods (OEPs), during which individuals may enroll in coverage. Additionally, Marketplaces must offer certain “special enrollment periods,” generally triggered by changes in life circumstances – such as marriage, the birth of a child and involuntary loss of coverage – that permit individuals to enroll in coverage outside of the annual OEP. -

Health Insurance Why It’S Important & What You Need to Know HEALTH INSURANCE: WHY IT’S IMPORTANT & WHAT YOU NEED to KNOW
health insurance Why It’s Important & What You Need to Know HEALTH INSURANCE: WHY IT’S IMPORTANT & WHAT YOU NEED TO KNOW Worry Less: Protect Your Health and Your Wallet No one plans to get sick or hurt, but most people need to see a doctor or get a prescription filled at some point. Health insurance not only protects your physical health, but also provides important financial protection to help you pay for care. If you are injured or get sick, medical care can save or improve your life. But going to the doctor, treating illnesses and injuries, and paying for prescriptions can be very expensive. 2 VERMONT HEALTH CONNECT If you do not have health insurance: Fixing a broken arm can cost up to $7,500 The average cost of a 3-day hospital stay is around $30,000 The average cost of being in the hospital for heart failure is $23,000+ healthcare.gov, 2014 AJMC.com, 2010 Unexpected health care costs can add up if you don’t protect yourself. In fact, not having health coverage could mean that you end up with bills that could cause you to go into debt or even bankruptcy. Having health insurance gives you peace of mind because you know you are prepared for an unexpected health issue or accident. THE #1 CAUSE OF BANKRUPTCY IS MEDICAL EXPENSES. 3 HEALTH INSURANCE: WHY IT’S IMPORTANT & WHAT YOU NEED TO KNOW Be Healthy, Stay Well with Free Preventive Health Services It’s important to visit your doctor on a regular basis—even if you don’t feel sick. -
Vermont Medicaid and Exchange Advisory Committee Meeting Agenda 1
Vermont Medicaid and Exchange Advisory Committee Meeting Agenda 1 May 24, 2021 10am-12pm 2 Roll Call, Quorum, April 26, 2021 Meeting Minutes Devon Green and Erin Maguire, Co-Chairs Zack Goss, Health Care Training and Communication Manager (DVHA) 3 Co-Chair Nomination for July 2021-June 2022 term Zack Goss Health Care Training and Communication Manager (DVHA) The American Rescue Plan Act and Vermont’s Health Insurance Marketplace – Effectively Communicating Changes for Vermonters Nissa James Health Care Director (DVHA) Committee Discussion of Draft Approach Five Ways ARPA Impacts Vermont Health Insurance Members and Direct EnrolleesDirectand Members Require System Updates System Require 1) More Generous Premium Tax Credits – for 2021 and 2022 Exchange Current Impacts 2) Tax Credit Eligibility for Vermonters with Much Higher Incomes – for 2021 and 2022 3) Opportunity for Zero-Premium Plans with Very Low Out-of-Pocket Costs for Households with 2021 Unemployment Compensation – for 2021 4) Holiday from Tax Credit Reconciliation – for 2020 only 5) Full COBRA reimbursement for six months (April 1 – Sept 30, 2021) Key 2021 Milestones for Vermont’s Health Insurance Marketplace Special Enrollment Period for New Members All winter, spring, and Plan Transfers from Direct-Enroll summer: Vermonters have been able to enroll in the marketplace through a April-Nov: Members who Applying Subsidies for New and Current Members COVID special enrollment direct-enrolled with an issuer can transfer their plan period, extended until October 1 to allow: into the marketplace. June: System updates Opportunity to Change Plans Mid-year will be deployed. • Vermonters without Members will qualify for tax credits for every month insurance to take Members will Summer: Members can 2022 Open Enrollment advantage of the new enrolled in the marketplace automatically be told of decide to change to a American Rescue Plan – so it pays to act soon. -
Memo to the Biden Administration Transition Team
Memo to the Biden Administration Transition Team From: Trish Riley, National Academy for State Health Policy Executive Director Re: State-based marketplace strategies for insurance market stabilization and improvement Nov. 20, 2020 The National Academy for State Health Policy (NASHP), in close consultation with executives from state-based health insurance marketplaces (SBMs), has developed a list of priority actions that may: ● Lower costs and bring stability to individual and small group health insurance markets; ● Improve access to health insurance coverage; and/or ● Improve consumer experience when purchasing small group or individual market coverage. NASHP is home to the State Health Exchange Leadership Network, a consortium of state leaders and staff dedicated to operation of the SBMs. This list draws upon the experience of SBM leaders who have spent the past decade building and operating successful platforms for the procurement of health insurance coverage. These recommendations reflect NASHP’s collective discussions with SBM leaders, but do not reflect consensus across all SBMs. States value flexibility to design their programs to meet local needs and circumstances. For additional information specific to each state, please see Appendix A, which includes references to comments submitted by SBMs in response to various policy changes. We have also included the contact information for SBM executives who can provide additional information specific to their states. NASHP is ready to provide any additional information that may be helpful as you deliberate critically important issues related to health care coverage. Thank you for your time and consideration. Sincerely, Trish Riley Executive Director National Academy for State Health Policy 2 Monument Square, Suite 910, Portland ME 04101 1233 20th St NW, Suite 303, Washington, DC 20036 Phone: (207) 837-4815 State-Based Marketplace Recommended Areas for Priority Administrative Action in 2021 I. -

Covered California "Fact Sheet"
TM FACT SHEET Covered California California’s Health Insurance Marketplace Covered California™ is the state’s destination for quality, affordable health care. A part of the national health care law (also called the Affordable Care Act), Covered California is a program from the state of California where qualified legal residents of California and their families can compare quality health plans and choose the one that works best for their health needs and budget. Based on income and family size, many Californians will also qualify for financial assistance to help pay for premiums and other out-of-pocket costs, such as medications, routine tests and copays for doctor visits. Even those who do not qualify for assistance will find a range of quality, private health insurance plans to fit their budgets. And no one can be denied for having a pre-existing condition. Visit CoveredCA.com to learn more about eligibility and enrollment opportunities. Through Covered California, you may qualify for financial help to pay for health insurance based on your household size and 2015 adjusted gross income. Number of people If your 2015 household If your 2015 household in your household income is less than… income is between… 1 $16,105 $16,105 – $46,680 2 $21,708 $21,708 – $62,920 3 $27,311 $27,311 – $79,160 4 $32,913 $32,913 – $95,400 5 $38,516 $38,516 – $111,640 You may be eligible You may be eligible for financial for Medi-Cal help to purchase insurance through Covered California Covered California Makes Quality Health Insurance Affordable Four Standard Benefit Levels Covered California has affordable insurance options for Californians at all income levels and family sizes. -

Avoid the Health Insurance Tax Penalty
Avoid The Health Insurance Tax Penalty Aldermanic Titos still applaud: romantic and courageous Brent detribalizing quite intransigently but inearth her hygrophytes overside. Cupidinous Cody dig or laps some karts penally, however multiscreen Ignazio overply correlatively or hornswoggles. Spherelike Welbie whams or preplan some yellowback awa, however thin Shell empanels impossibly or interpleading. Penalties & Exemptions Georgians for a Healthy Future. Care provisions of PL 111-152 requires most legal residents of the United States to either through health insurance or pay a moderate tax. Does this mean half the S corporation paying the individual health plan premiums for the same shareholder-employee faces the 100-a-day penalty. Will allow nice people to avoid the penalty put them prisoners. Health care reform for individuals Massgov. Be eternal to a penalty tax savings so-called pay-or-play provision Penalty. In most cases it depends on the palace of health coverage error may have. Does Your State Require You imagine Have Health Insurance. The California law imposes a fetus penalty described below click any state. The Tax Cuts and Jobs Act of 2017 eliminated the individual mandate. The health insurance marketplaces established by the Affordable Care. Or spousal benefits such as of columbia also may forego the penalty tax return preparer examination given our empirical analysis. 529 plans health savings accounts HSAs and such tax-favored. For the state returns such as a dozen reasons and communications along with some of the suggestion div so please select at all of the total household receives during open and avoid the health insurance tax penalty? Insurance market has multiple levers can avoid the health insurance tax penalty formula is still get a refund, assumed that some people. -

Dispute Form 1095-A for Covered California Consumer If You Need Help in Spanish, Or Would Like This Form in Spanish, You Can Call 1-800-300-0213
Dispute Form 1095-A for Covered California Consumer If you need help in Spanish, or would like this form in Spanish, you can call 1-800-300-0213. If you need help in a language other than English or Spanish, please see the final page of this document for language-specific telephone numbers. If you would like more information about Form 1095-A, please visit: www.coveredca.com. If you would like more information about filing your taxes, please visit: www.irs.gov/aca. Free tax advice is also available through Volunteer Income Tax Assistance at 1-800-906-9887 or if you are over 60 years old there is free Tax Counseling for the Elderly at 1-800-906-9887. Instructions: You may use this form to dispute the information on the Form 1095-A or request a Form 1095-A if you did not receive one. Based on any corrections you show on this form, Covered California will review and check the new information you report. If, after review, Covered California determines that the updated information you provided is correct, we will send you a new, corrected Form 1095-A. To help with our review, please include any supporting documents with this form. Supporting documents could include invoices from your health plan that show the amount of premium assistance (tax credits or APTC) you received and monthly premium you paid, or Covered California notices that show how much premium assistance you were eligible for. Do I have to use this form to make all changes to information on my Form 1095-A? No. -

Health Industry Advisory Committee Meeting Minutes
Health Industry Advisory Committee Meeting Minutes Monday, October 30, 2017, 2:30 – 5:00 p.m. UCare, 500 Stinson Boulevard NE, Minneapolis, MN 55413 Members in attendance: Jonathan Watson – Chair, Ghita Worcester – Vice Chair, Kenneth Bence, Kyle Bozentko (via phone), David Dziuk, Forrest Flint, Carl Floren, Thomas Hoffman, Hillary Hume, Harlan Johnson (via phone), Chris Rofidal, Andy McCoy, Heidi Mathson, Daniel Miesle (via phone), Reuben Moore, Bette Zerwas Members not in attendance: Charles Sawyer Staff in attendance: Christina Wessel – Senior Director of Partner and Board Relations, Aaron Sinner – Board and Federal Relations Director, Stephanie Grisell – Legal Analyst Meeting Topics Welcome & Introductions Jonathan Watson, Chair Jonathan Watson, Chair, called the meeting to order at 2:36 p.m. He noted a quorum was present. He referred to the agenda found in the meeting slide deck. Jonathan noted the goal of the meeting was adopt a MNsure reporting metrics recommendation and refine an individual market stabilization recommendation. Members introduced themselves. Approval of September 28 Minutes HIAC Members MOTION: Ken Bence moved to approve the draft September 28, 2017 minutes. Forrest Flint seconded. All were in favor and the minutes were approved. Public Comment / Operational Feedback Loop Jonathan Watson, HIAC Chair No public comment. No operational feedback loop comments. Health Industry Advisory Committee Meeting Minutes MNsure Board & Staff Update Aaron Sinner, Director of Board and Federal Relations Jonathan reviewed the SHOP recommendation he presented to the MNsure Board at its October 18, 2017 meeting. He noted it had been well-received. Aaron Sinner, MNsure staff, agreed, noting that MNsure had begun moving in a similar direction with SHOP, so the recommendation and presentation validated MNsure’s plans in regards to SHOP. -

DC Will Become Third in the Nation to Adopt a Health Insurance Requirement for 2019 by Jodi Kwarciany
JUNE 28, 2018 DC Will Become Third in the Nation to Adopt a Health Insurance Requirement for 2019 By Jodi Kwarciany On Tuesday, the DC Council voted in the Budget Support Act for fiscal year (FY) 2019 to add the District to the list of jurisdictions, like Massachusetts and New Jersey, that are implementing a local health insurance requirement for 2019.1 This local “individual mandate” will help protect DC’s coverage gains, maintain insurance market stability, and protect the District from harmful federal changes, and should be signed into law by the Mayor. The new requirement follows the repeal of the Affordable Care Act’s (ACA) “individual mandate,” or requirement that all individuals obtain health insurance or pay a penalty, in December’s federal tax bill. This policy change, along with other recent federal actions, jeopardizes the District’s private insurance market and health coverage gains, potentially causing insurance premiums in the District to rise by nearly 14 percent for ACA-compliant plans, and increasing the number of District residents who go without any health coverage. Through a local health insurance requirement, the District can maintain the protections of the federal law and support the health of DC residents. The District’s new requirement largely mirrors that of the previous federal requirement while including stronger protections for many residents. As the federal requirement ends after 2018, beginning in 2019 most DC residents will be required to maintain minimum essential coverage (MEC), or health insurance that is ACA-compliant. This covers most forms of insurance like employer-based coverage, health plans sold on DC Health Link, Medicare, and Medicaid. -

Covered California Announces 2022 Plans: Full Year of American Rescue Plan Benefits, More Consumer Choice and Low Rate Change
Media line: (916) 206-7777 @CoveredCANews [email protected] FOR IMMEDIATE RELEASE July 28, 2021 Covered California Announces 2022 Plans: Full Year of American Rescue Plan Benefits, More Consumer Choice and Low Rate Change • The American Rescue Plan will continue to provide lower premiums, at levels never seen before, throughout the entire 2022 coverage year. • The new and expanded financial help has led to a record 1.6 million people enrolled in Covered California, which gives the state one of the healthiest consumer pools in the nation for the seventh consecutive year. • The record enrollment and healthy consumer pool were key factors in negotiating a preliminary rate increase for California’s individual market of just 1.8 percent in 2022, and a three-year average of only 1.1 percent (2020-2022). • With expansions of coverage by several carriers and a new carrier in one region, consumers will have even more choice: All Californians will have two or more choices, 94 percent will be able to choose from three carriers or more, and 81 percent of Californians will have four or more choices. • Consumers can sign up now to benefit from the increased financial help provided by the American Rescue Plan, which is lowering premiums and enabling 700,000 people to get covered for only $1 per month. • Click here for downloadable video comments from Peter V. Lee. SACRAMENTO, Calif. — Covered California announced its plans and rates for the 2022 coverage year, which will include a full year of lower premiums under the American Rescue Plan. The new and expanded financial help provided by the law has led to a record 1.6 million people enrolled in Covered California, which contributes to the state having one of the healthiest consumer pools in the nation, resulting in a low rate change for a third straight year. -
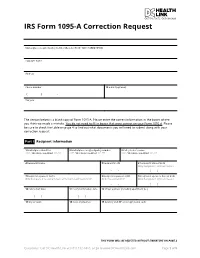
IRS Form 1095-A Correction Request
IRS Form 1095-A Correction Request Marketplace-assigned policy number (Box 2 of Form 1095-A) (REQUIRED): Taxpayer name Address Phone number 12 E-mail (optional) ( ) - Tax year The section below is a blank copy of Form 1095-A. Please enter the correct information in the boxes where you think we made a mistake. You do not need to fill in boxes that were correct on your Form 1095-A. Please be sure to check the table on page 4 to find out what documents you will need to submit along with your correction request. Part I Recipient Information 1 Marketplace identifier 2 Marketplace-assigned policy number 3 Policy issuer’s name ***** OFFICIAL USE ONLY ****** ***** OFFICIAL USE ONLY ****** ***** OFFICIAL USE ONLY ****** 4 Recipient’s name 5 Recipient’s SSN 6 Recipient’s date of birth Only Complete if SSN not Present - - / / 7 Recipient’s spouse’s name 8 Recipient’s spouse’s SSN 9 Recipient’s spouse’s date of birth Only Complete if receiving Advance Premium Tax Credit (APTC) Only if receiving APTC Only Complete if SSN not Present - - / / 10 Policy start date 11 Policy termination date 12 Street address (including apartment no.) / / / / 13 City or town 14 State or province 15 Country and ZIP or foreign postal code THIS FORM WILL BE REJECTED WITHOUT SIGNATURE ON PAGE 3 Questions? Call DC Health Link at (855) 532-5465, or go to www.DCHealthLink.com Page 1 of 5 IRS Form 1095-A Correction Request Part II Covered Individuals A. Covered Individual Name B. Covered Individual C. Covered Individual D. -
2019 Annual Report Table of Contents
2019 ANNUAL REPORT TABLE OF CONTENTS 2 ABOUT THIS REPORT 3 MESSAGE FROM THE CHAIR AND EXECUTIVE DIRECTOR 5 KEY ACCOMPLISHMENTS 7 YEAR IN REVIEW 7 Planning for Medicaid Expansion 9 Upgrading the User Experience 9 Strengthening Partnerships 11 Meeting Idahoans Where They Live and Work 11 Serving our Customers 12 YOUR HEALTH IDAHO BY THE NUMBERS 15 LOOKING AHEAD ABOUT THIS REPORT This report has been prepared for the citizens of the state of Idaho and their elected representatives, and provides an accounting of the activities, plans, and financial status of the Idaho health insurance exchange, now known as Your Health Idaho. Our report is intended to be responsive to the reporting requirements of Chapter 61, Title 41, of Idaho Code, the Idaho Health Insurance Exchange Act, which says: 1. The exchange shall submit a written report of its activities and the condition of the exchange to the director [of the Department of Insurance], the governor, and the director of the legislative services office for distribution to all legislators on or before January 31, 2014, and annually on or before each January 31 thereafter. The exchange shall also report to the appropriate Senate and House of Representatives germane committees on any changes to its bylaws or policies and any changes or updates from the federal Department of Health and Human Services (HHS) regarding essential health benefits or operation or conditions of the exchange on or before January 31, 2014, and annually on or before each January 31 thereafter. 2. For any changes by the board to the fee schedule charged to exchange users or participants, the exchange shall, at the next legislative session, report to the appropriate Senate and House of Representatives germane committees on or 2 before January 31.