Chapter 5 Cost Effectiveness of Dialysis and Resource Utilization
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(COVID-19) SITUATION in MALAYSIA 6 October 2020
PRESS STATEMENT MINISTRY OF HEALTH MALAYSIA UPDATES ON THE CORONAVIRUS DISEASE 2019 (COVID-19) SITUATION IN MALAYSIA 6 October 2020 Current Status of Confirmed COVID-19 Cases Who Have Recovered The Ministry of Health (MOH) would like to inform that 87 cases have fully recovered and discharged today. Cumulatively, 10,427 confirmed COVID-19 cases have been discharged (77.2% of total cumulative cases). Current Situation of COVID-19 in Malaysia 6 October 2020, 12 pm, MOH would like to inform that 394 cases were detected in the Tembok Cluster, a prison in Kedah (i.e. 57.0% of the total cases reported today), 294 cases from other localities and three (3) imported cases. In total, 691 additional confirmed COVID-19 cases were reported to the National Crisis Preparedness and Response Centre (CPRC) MOH today. Cumulatively there are now 13,504 confirmed COVID-19 cases in Malaysia. Therefore, there are currently 2,936 active and infective COVID-19 cases. They have all been isolated and given treatment. Of the 691 cases reported today, three (3) are imported cases who were infected overseas, involving one (1) Malaysian and two (2) non- Malaysian who were travellers from: • India – 1 case reported in Kuala Lumpur, a Malaysian. • Egypt – 1 case reported in Sarawak, a non-Malaysian. • Philippines – 1 case reported in Selangor, a non-Malaysian. Of the 688 local transmission cases, 661 cases are Malaysians and 27 cases non-Malaysians. Of the 688 cases, 394 cases are those detected in the Tembok Cluster, a prison in Kedah (57.0% of total cases reported today). -

1. MOA AAA 2016 Abstract
Abstract Combined Meeting of the th Malaysian Orthopaedic 46Association Annual General Meeting / Annual Scientific Meeting th ASEAN Arthroplasty 10 Association Meeting 2016 Fundamentals In Orthopaedics – Back To Basics Pre-Conference Day Conference Days 25th May 2016 26th to 28th May 2016 Persada Johor International Convention Centre, Johor Bahru, Malaysia. www.moa-home.com Abstract CD (Please click on the links below to view the respective categories of abstracts.) Oral Presentations Abstracts Poster Presentations Abstracts (Click Here...) Combined Meeting of the 46th Malaysian Orthopaedic Association Annual General Meeting / Annual Scientific Meeting & 10th ASEAN Arthroplasty Association Meeting 2016 26th May 2016 (Thursday) - Lecture Hall MOA 1, Level 3 TIME TOPIC SPEAKER 0700 -1730 REGISTRATION COUNTER OPENS SUBIR SENGUPTA MEMORIAL LECTURE Chairperson Prof Dr Saw Aik 0830 - 0900 Prevention And Early Detection Of DDH - The Japanese SM 01 Prof Dr Makoto Kamegaya Experience OPENING CEREMONY 0900 - 1030 Orthopaedics At The Frontlines In A Changing Globalised World. SK 01 Roles And Responsibilities. Dato' Dr Ahmad Faizal Mohd Perdaus A View From A Humanitarian And Colleauge. 1030 - 1100 TEA BREAK & EXHIBIT VISIT SPORTS Dr Shamsul Iskandar Hussein Chairperson Dr Raymond Yeak Dieu Kiat Revision Anterior Cruciate Ligament Reconstruction: Analysis 1100 - 1112 SX 01 Of Causes Of Failures, Preoperative Clinical Evaluation And Dr Deepak V. Patel Planning, Surgical Technique, And Clinical Outcomes SLAP (Superior Labrum Anterior Posterior) -

Nursing Division Ministry of Health Malaysia
NURSING DIVISION MINISTRY OF HEALTH MALAYSIA First Edition Mei 2017 SAFE OPERATING PROSEDURE FOR ADMINISTRATION OF INTRAVENOUS ( BOLUS ) EDICATION SAFE OPERATING PROSEDURE FOR ADMINISTRATION OF INTRAVENOUS ( BOLUS ) EDICATION ACKNOWLEDGEMENT Nursing Division Ministry of Health Malaysia gratefully acknowledges the expert contributions made by the following members, without whom the development of this consensus document would not be possible. ADVISOR Puan Hajah Rosena binti Abdul Ghani Director of Nursing Division, MOH EDITIORS Dr. Nor’Aishah Binti Abu Bakar Head of Patient Safety Unit Senior Public Health Physician & Senior Principle Assistant Director Medical Care Quality Section Medical Development Division, Ministry of Health Malaysia Puan Monica Chee Soon Nyuk Senior Assistant Director of Nursing, Nursing Division, MOH Puan Ng Siew Luan Nursing Matron, Nursing Division, MOH TECHNICAL WORKING GROUP Puan Darmawan binti Ramli Nursing Tutor, Unit Curriculum, Nursing Division, MOH Puan Suzana binti Jaafar Assistant Director, Nursing Division. MOH Puan Norlaila binti Mohd Husin Assistant Director, Nursing Division. MOH Puan Zanita binti Ahmad Clinical Nursing Matron, Family Health Development Division, MOH Puan Razmiyah binti Awang Nursing Matron, Nursing Division, MOH Puan See Booi Cheng Nursing Matron, Family Health Development Division, MOH Puan Noor Wati binti Esa Nursing Matron, Kuala Lumpur General Hospital Puan Mariati binti Alias Nursing Matron, Putrajaya Hospital Puan Noorsiah binti Harun Nursing Matron, Kajang Hospital Puan Zalimah -
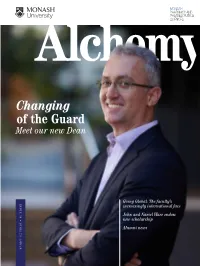
Changing of the Guard
MONASH PHARMACY AND PHARMACEUTICAL SCIENCES Changing of the Guard Meet our new Dean Going Global: The faculty’s ISSUE 34 • SUMMERISSUE 34 2019/20 increasingly international face John and Nariel Ware endow new scholarship Alumni news Fast Facts 2017 CLARIVATE ANALYTICS HIGHLY CITED RESEARCHERS (2004–2014) No.1 worldwide in Pharmacology and Toxicology QS WORLD UNIVERSITY RANKINGS BY SUBJECT, PHARMACY AND PHARMACOLOGY No.1 in Australia and Asia-Pacific 2018 No.1 worldwide for academic reputation 2018 No.2 worldwide 2018 Top 10 worldwide (average 2011–2018) Excellence in Research for Australia 2015 Top rating of 5 in all sectors (well above world standard) PharmAlliance with University of North Carolina at Chapel Hill, US and University College London, UK National Alliance for Pharmacy Education with University of Queensland, University of Sydney University of South Australia MONASH PHARMACY AND PHARMACEUTICAL SCIENCES Fast Facts Contents 02 News in brief Alchemy is produced 2017 CLARIVATE ANALYTICS by the Development Office, HIGHLY CITED RESEARCHERS (2004–2014) 04 Dean Charman steps down Faculty of Pharmacy and Pharmaceutical Sciences, No.1 worldwide in Pharmacology and Toxicology 06 Research with impact Monash University. Managing Editor: John Palmer 10 Special feature: Going global Writers: Rahul Ratwatte, Cyndi Ferguson, QS WORLD UNIVERSITY RANKINGS BY SUBJECT, Divya Krishnan 11 Monash University Malaysia’s School of Pharmacy Design: BPO Intelligence PHARMACY AND PHARMACOLOGY celebrates 10 years Photography: Paul Philipson and Greg Ford -

Risk Factors Associated with Necrotising Enterocolitis in Very Low Birth Weight Infants in Malaysian Neonatal Intensive Care Units
O riginal A rticle Singapore Med J 2012; 53(12) : 826 Risk factors associated with necrotising enterocolitis in very low birth weight infants in Malaysian neonatal intensive care units Nem-Yun Boo1, MRCP, FRCPCH, Irene Guat Sim Cheah2, MRCP, FRCPCH; Malaysian National Neonatal Registry Introduction This study aimed to identify the risk factors associated with necrotising enterocolitis (NEC) in very low birth weight (VLBW; weight < 1,501 g) infants in Malaysian neonatal intensive care units (NICUs). Methods This was a retrospective study based on data collected in a standardised format for all VLBW infants born in 2007 (n = 3,601) and admitted to 31 NICUs in Malaysian public hospitals. A diagnosis of NEC was made based on clinical, radiological and/or histopathological evidence of stage II or III, according to Bell’s criteria. Logistic regression analysis was performed to determine the significant risk factors associated with NEC. ResuLts 222 (6.2%) infants developed NEC (stage II, n = 197; stage III, n = 25). 69 (31.3%) infants died (stage II, n = 58; stage III, n = 11). The significant risk factors associated with NEC were: maternal age (adjusted odds ratio [OR] 1.024, 95% confidence interval [CI] 1.003–1.046; p = 0.027), intrapartum antibiotics (OR 0.639, 95% CI 0.421–0.971; p = 0.036), birth weight (OR 0.999, 95% CI 0.998–0.999; p < 0.001), surfactant therapy (OR 1.590, 95% CI 1.170– 2.161; p = 0.003), congenital pneumonia (OR 2.00, 95% CI 1.405–2.848; p < 0.001) and indomethacin therapy for the closure of patent ductus arteriosus (PDA) (OR 1.821, 95% CI 1.349–2.431; p = 0.001). -

Crc Sabah Newsletter
Issue 3 : September– December 2013 CRC SABAH NEWSLETTER Inside This Issue WELCOME TO ISSUE 3 OF CRC NEWSLETTER Welcome to Issue 3 of CRC Sabah Newletter Warmest Greeting from CRC Sabah! Welcome 2014, and Happy Investigator Initiated Research (IIR) New Year! As we begin this New Year, we hope that 2014 will and industry Sponsored Research bring bigger and better things for the Clinical Research Centre (ISR) updates (CRC). Activities and Photo Gallery In This issue, we want to announce the upcoming workshop organized by CRC Sabah for the year 2014. Contact Us 1. Good Clinical Practice (GCP) Workshop collaboration Upcoming Events with Clinical Research Malaysia (CRM) 19th – 21st Feb 2014, Sabah Women and Children Hospital. 2. Sabah Good Clinical Practice (GCP) Workshop 26th – 28th Mar 2014, Hospital Queen Elizabeth II. CRC’s OBJECTIVE 3. Basic to Intermediate Medical Biostatistics Using SPSS Workshop 2014 1. To promote a culture of 14 – 17 April 2014, School Of Medical, University Malaysia research among healthcare Sabah (UMS). workers in Sabah. 4. Advanced Medical Biostatistics Using SPSS Workshop 2014 2 – 6 Jun 2014, School Of Medical, University Malaysia Sabah (UMS). 2. To disseminate skills in Grab this opportunity and never stop Learning! See you there! Methodology, Statistical tools, and techniques in designing and conducting clinical trials. CRC’s Vision 3. To provide healthcare workers the principle of methodology and To be a leading clinical research institution in Asia biostatistics in clinical research CRC’s Mission To improve patients health outcomes through ethical and quality clinical research. ISSUE 3: September – December 2013 CRC Sabah Newsletter MESSAGE AND RESOLUTION CRC SABAH HEAD 2014 First and foremost, I would like to congratulate the editorial team for their success in publishing the third edition of CRC Sabah Newsletter. -

Curriculum Vitae BIODATA Name Zaiton Kamarruddin P.C.M IC 630624-08-5388 Age 58
Curriculum Vitae BIODATA Name Zaiton Kamarruddin P.C.M IC 630624-08-5388 Age 58 Nationalilty Malaysian State Health Deputy Director (Pharmacy) Current State Health Department Position Perak Darul Ridzuan c/o Hospital Bahagia Ulu Kinta 31250 Tanjung Rambutan Address Perak Darul Ridzuan. Email [email protected] Contact Off : 605-5337318 ACADEMIC ACHIEVEMENTS PhD Program ( Health Sciences)( 2001-2005) 2001-2005 CURTIN University of Technology, Perth, WA M.Pharm (Clinical Pharmacy) – University of Science Malaysia (USM). 1994 Penang (1994) 1987 B. Pharm (Hons)- University of Science Malaysia (USM). Penang (1987) WORK ACHIEVEMENTS / AWARD 2013 Excellent Service Award, Public Service MOH 2012, by JKN Selangor 2012 Excellent Service Certificate, December 2012, Hospital Kajang. 2001 Excellent Service Award, Public Service 2012, by JKN Perak Awarded by the Competency Unit, Ministry of Health, Malaysia for Excellent Efficiency. (PTK 4) 2020 Anugerah Darjah Kebesaran, Bintang Dan Pingat Negeri Perak Tahun 2020 - `PADUKA CURA SI MANJA KINI ` (P.C.M) Page 1 of 12 WORK EXPERIENCES Head of Unit (LEAN), 2019 -2020 Centre for Organizational Excellence Development Institute for Health Management, Ministry of Health Malaysia (MOH) Core Business: Research, Training and Consultancy related to LEAN Healthcare / Management 2014-2018 Head of Division, Healthcare Quality Research Division,Institute for Health Systems Research (IHSR),Ministry of Health Malaysia. Project Leader in Lean Healthcare Initiatives of MOH under Government Transformation Program (GTP) -

IOI Corporation Berhad, Sakilan Group Sandakan, Sabah, Malaysia
PUBLIC SUMMARY REPORT INITIAL RSPO CERTIFICATION ASSESSMENT IOI Corporation Berhad, Sakilan Group Sandakan, Sabah, Malaysia Report Author Allan Thomas – 21 st April 2009 [email protected] Tel: +61 412 492 353 BSi Management Systems Singapore Pte Ltd ( Co. Reg. 1995 02096-N) Malaysia Office (Co.Reg. 9942MX) 460 Alexandra Road Suite 19.05 Level 19, Wisma Goldhill #08-01/02 PSA Building 65, Jalan Raja Chulan SINGAPORE 119963 50200 Kuala Lumpur Tel +65 6270 0777 MALAYSIA Fax +65 6270 2777 Tel +60 32032 2252 (Hunting Line) www.bsi-asia.com Fax +60 32032 2253 Soon Leong Chia: [email protected] Teo Chin Siong: [email protected] TABLE of CONTENTS Page N o SUMMARY…… .....................................................................................................................................1 Abbreviations USED................................................................................................................................1 1.0 Scope of Certification Assessment.................................................................................................1 1.1 National Interpretation Used..........................................................................................................1 1.2 Certification Scope.........................................................................................................................1 1.3 Location and Maps.........................................................................................................................1 1.4 Description of Supply -

3Rd Report of the National Cataract Surgery Registry 2004
National Cataract Surgery Registry Ministry of Health Malaysia THE THIRD REPORT OF THE NATIONAL CATARACT SURGERY REGISTRY 2004 Edited by Goh Pik Pin Shamala Retnasabapathy Rajalakshmi Gopal Ronald Arun Das A publication of the National Cataract Surgery Registry And Clinical Research Centre, Ministry of Health October 2004 © National Cataract Surgery Registry, Malaysia. Published by the National Cataract Surgery Registry (NCSR) C/O Clinical Research Centre, Level 3, Dermatology Block, Kuala Lumpur Hospital, Jalan Pahang, 50586 Kuala Lumpur. General Line: 603-2698 0310 Fax: 603-2691 1682 Email [email protected] Website: http://www.crc.gov.my/ncsr Disclaimer The data reported here have been supplied by NCSR. The interpretation and reporting of these data are the responsibility of the Editor and in no way should be seen as an official policy or interpretation of the NCSR. Suggested citation The suggested citation for this report is as follows: Goh Pik Pin, Shamala Retnasabapathy, Rajalakshmi Gopal, Ronald Arun Das.(Eds) THE SECOND REPORT OF THE NATIONAL CATARACT SURGERY 2003 Kuala Lumpur, Malaysia 2004 Electronic version Electronic version of this report can be downloaded at http://www.crc.gov.my/ncsr ISSN 1675-8447 Forward i ACKNOWLEDGMENTS i National Cataract Surgery Registry Advisory Committee i PARTICIPATING CENTRES 1. Angkatan Tentera Kem Terendak Hospital Head, Ophthalmology Department : Lt. Kol. (Dr) Nor Aishah Malik Dr In Charge : - Coordinator : Sarjan Jawariah Ali Participating From : January-November 2002 January-December 2003 2 Alor Setar Hospital Head, Ophthalmology Department : Dr. Ahmad Mat Saad Dr In Charge : Dr. Zaharidah Abd Kadir Coordinator : T/AN Siti Aishah Salim Participating From : January-December 2002 January-December 2003 3 Duchess Of Kent Hospital, Sandakan Head, Ophthalmology Department : Dr. -

Covid-19) Situation in Malaysia
PRESS STATEMENT MINISTRY OF HEALTH MALAYSIA UPDATES ON THE CORONAVIRUS DISEASE 2019 (COVID-19) SITUATION IN MALAYSIA Current Status of Confirmed COVID-19 Cases Who Have Recovered 30 April 2020 – The Ministry of Health (MOH) would like to inform that 84 cases have fully recovered and discharged well today. Cumulatively, 4,171 confirmed COVID-19 cases have fully recovered and discharged well (69.5% of total cumulative cases). Current Situation of COVID-19 in Malaysia 30 April 2020, 12 pm – A total of 57 additional confirmed COVID-19 cases were reported to the National Crisis Preparedness and Response Centre (CPRC) MOH today. Cumulatively there are now 6,002 confirmed COVID-19 cases in Malaysia. Therefore, there are currently 1,729 active and infective COVID-19 cases. They have been isolated and provided treatment. Of these 57 additional cases reported today, 25 are imported cases. The remaining 32 cases are due to local transmission. Currently, 36 confirmed COVID-19 cases are receiving treatment in intensive care units (ICU), and of these, 14 cases are on ventilation support. Regretfully, two (2) additional COVID-19 deaths were reported to the National CPRC MOH today. Cumulatively, there are now 102 COVID-19 deaths in Malaysia (1.7% of total cumulative cases): 1. Death #101: Case 4,657 is a 64 year-old Malaysian man with a history of haematological cancer. He was a close contact to a confirmed COVID-19 case (Case 4,476; from the Bali PUI cluster). He was admitted into Tengku Ampuan Afzan Hospital, Pahang on 12 April 2020 and was pronounced dead on 29 April 2020 at 4.14 pm. -

MJPCH 2010 (Dec); Vol. 1; Supplementary 2
MJPCH 2010 (Dec); Vol. 16; Supplementary 2 MJPCH 2010 (Dec); Vol. 1; Supplementary 2 In conjunction with 32ND MALAYSIAN PAEDIATRIC ASSOCIATION ANNUAL CONGRESS 14-17TH OCTOBER 2010 HILTON HOTEL, KULA LUMPUR ABSTRACTS ORGANISED BY MALAYSIAN PAEDIATRIC ASSOCIATION MJPCH 2010 (Dec); Vol. 16; Supplementary 2 Content YOUNG INVESTIGATOR AWARD PAPERS YIA 1 ASSESSMENT OF MORTALITY PREDICTION TOOLS IN PAEDIATRIC INTENSIVE CARE UNIT UMMC AND ESTABLISHING A NOVEL PAEDIATRIC INTENSIVE CARE REGISTRY (PEDICARE2008) 1 Anis Siham Zainal Abidinl1, LCS Lum2, N Ismail3, M Sabri4 YIA 2 PREVALENCE OF GLUCOSE-6-PHOSPHATE DEHYDROGENASE (G6PD) INTERMEDIATE IN THE NEWBORNS AND THE ACCURACY OF SEMI- QUANTITATIVE FLUORESCENT SPOT TEST (FST) AS SCREENING TOOL 2 Azizan Aziz1, Thong MK2, Lim CT2 YIA 3 JUVENILE IDIOPATHIC ARTHRITIS IN MALAYSIA: THE SELAYANG EXPERIENCE 3 Cham Weng Tarng, Tang Swee Ping YIA 4 HEALTH-RELATED QUALITY OF LIFE IN SABAH CHILDREN WITH TRANSFUSION 4 DEPENDENT THALASSAEMIA Choong Yee Wan, Lee Chee Chan YIA 5 HYPOTHYROXINAEMIA IN PRETERM INFANTS IN SPECIAL CARE NURSERY (SCN), UNIVERSITY MALAYA MEDICAL CENTRE (UMMC) 5 Hannah Wardiah Rosland, Chin-Theam Lim, Fatimah Harun YIA 6 CORONARY ARTERY ABNORMALITY IN COMPLETE KAWASAKI DISEASE CHILDREN 6 TREATED WITH IMMUNOGLOBULIN Amelia Alias1, Chan TL2, Mohd Amin Itam1, Mat Bah MN1 ORAL PRESENTSTIONS ORAL PRESENTATIONS 1 OP1.1 A DESCRIPTIVE STUDY OF APNOEA OF PREMATURITY IN INFANTS LESS THAN 34 WEEKS OF GESTATION AND A COMPARATIVE STUDY OF ORAL CAFFEINE VERSUS ORAL AMINOPHYLLINE IN THE TREATMENT OF APNOEA OF PREMATURITY 7 Lim Boon Soo, Lim Chin Theam OP1.2 HUMAN RHINOVIRUSES AMONG CHILDREN HOSPITALISED WITH ACUTE LOWER RESPIRATORY TRACT INFECTIONS 8 Mohamad Reza Etemadi1, Farid Azizi Jalilian1, Norrashidah Abdul Wahab3, Zamberi Sekawi1, Putri Yubbu2, Zurina Zainudin2, Shamarina Shohaimi4, Norlijah Othman2 MJPCH 2010 (Dec); Vol. -

2 YIA Abstract FA
YOUNG INVESTIGATOR AWARD NHAM CONGRESS 2019 YOUNG INVESTIGATOR AWARD ABSTRACTS Imaging YIA 1 Time: 1040-1055 Global Longitudinal Strain Predicts Adverse Left Ventricular Remodeling After ST-segment Elevation Myocardial Infarction Y.Y. Oon1, K.T. Koh1, K.H. Ho1, C.T. Tan1, F.E.P. Shu1, A. Said1,2, Y.L. Cham1, N.Z. Khiew1, N.H. Mohd Amin1, A.Y.Y. Fong1,3 , T.K. Ong1 1Department of Cardiology, Sarawak Heart Centre 2Faculty of Medicine and Health Sciences, University Malaysia Sarawak 3Clinical Research Centre, Sarawak General Hospital Arrhythmias YIA 2 Time: 1055-1110 Preliminary Results of Smartphone Electrocardiogram for Detecting Atrial Fibrillation After A Cerebral Ischemic Event: A Multi-center Randomised Controlled Trial KT Koh1, Law WC2, Zaw WM2, DHP Foo3, CT Tan1, D Samuel4, TL Fam4, CH Chai4, ZS Wong4, DB Chandan1,5, JSH Tan5, FEP Shu1, KH Ho1, YY Oon1, NZ Khiew1, YL Cham1, A Said1,6, NH Mohd Amin1, AYY Fong1,3, TK Ong1 1Department of Cardiology, Sarawak Heart Centre, Kota Samarahan, Malaysia 2Neurology Unit, Department of Medicine, Sarawak General Hospital, Kuching, Malaysia 3Clinical Research Centre, Sarawak General Hospital, Kuching, Malaysia 4Department of Medicine, Miri Hospital, Malaysia 5Department of Medicine, Bintulu Hospital, Malaysia 6Faculty of Medicine and Health Sciences, Universiti Malaysia Sarawak, Kota Samarahan, Malaysia Arrhythmias YIA 3 Time: 1110-1125 Prevalence of Atrial Fibrillation Detected by Single-Lead ECG among Senior Citizens at Northern Regions of West Malaysia in 2018 J.G. Ang1, H. Mohamed Hasnan1, K.R. Narasamuloo1, D. Karthikesan1, A.S. Mustafa1, S.S Gian Singh1, J.N. Lim2, A.S. Saad1, 1 1 YOUNG1 1 1 1 1 1 A.F.