No Moral Panic: Public Health Responses to Illicit Fentanyls
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Law Reform: Beyond Prohibition
THE AUSTRALIA INSTITUTE Drug Law Reform Beyond Prohibition Andrew Macintosh Discussion Paper Number 83 February 2006 ISSN 1322-5421 ii © The Australia Institute. This work is copyright. It may be reproduced in whole or in part for study or training purposes only with the written permission of the Australia Institute. Such use must not be for the purposes of sale or commercial exploitation. Subject to the Copyright Act 1968, reproduction, storage in a retrieval system or transmission in any form by any means of any part of the work other than for the purposes above is not permitted without written permission. Requests and inquiries should be directed to the Australia Institute. The Australia Institute iii Table of Contents Tables and Figures v Acknowledgements vi Summary vii 1. Introduction 1 2. Definitional and conceptual issues 4 2.1 What is a drug? 4 2.2 Licit and illicit drugs 4 2.3 Classifying psychoactive drugs 4 2.4 Other useful drug terms 5 2.5 What legislative options exist for drugs? 7 2.6 What do the terms ‘decriminalisation’ and ‘legalisation’ mean? 8 2.7 Diversion programs 9 3. A brief history of Australia’s drug laws 13 4. The theory behind Australia’s drug laws 23 4.1 Why have strict drug laws? 23 4.2 Reducing negative externalities and overcoming market failure 23 4.3 Reducing harm to individuals 28 4.4 Promoting and protecting moral values 30 5. Flaws in the strict prohibition approach 33 5.1 The direct costs of prohibition 33 5.2 The indirect costs of prohibition 34 6. -

Drug Free Workplace
QUESTAR III BOARD POLICY NO. 3-110 DRUG FREE WORKPLACE I. Prohibition of Drugs and Other Substances. The Board of Cooperative Educational Services is committed to the prevention of alcohol, tobacco, or other substance use and abuse. Of particular concern to the Board is the use and abuse of alcohol, tobacco, or other substances in the BOCES workplaces. The Board therefore establishes that at all sites, facilities, and properties owned by or under the control of the Board, and at all activities and programs operated or sponsored by the Board, it shall be strictly prohibited to use, manufacture, possess, possess with the intent to sell, dispense, sell, or distribute alcohol and other substances, and to use or possess drug paraphernalia. The possession and appropriate exclusive personal use of over-the-counter drugs or drugs that have been prescribed by and that are being used under the supervision of a physician are exempted from this prohibition. Also exempted is the mere possession of otherwise legal tobacco products. II. Drugs and Substances Prohibited. The term "alcohol or other substances" shall be construed hereunder to refer to, but not be limited to, alcohol, including beer and wine, tobacco in any form, inhalants, marijuana, cocaine, LSD, PCP, amphetamines, heroin, steroids, look- alikes, any substances referred to commonly as "designer drugs," and any other drug that is illegal under state or federal law. The inappropriate use of prescription and over-the-counter drugs is likewise prohibited. Ill. Employee Obligation to Report Conviction. Any employee of the BOCES who is convicted for violating a criminal drug statute shall notify the District Superintendent no later than five (5) days after such conviction. -

Current Approaches and Controversies: Legalization and Non-Legalization of Drugs
How to Cite Estevez, A. G., Espinosa, A. H. R., Rodríguez, D. L., & Leyva, T. F. (2019). Current approaches and controversies: legalization and non-legalization of drugs. International Journal of Health & Medical Sciences, 2(1), 26-32. https://doi.org/10.31295/ijhms.v2n1.85 Current Approaches and Controversies: Legalization and Non- Legalization of Drugs Ailén Galano Estevez Universidad de Oriente, Santiago, Cuba [email protected] Ana Hortensia Rodríguez Espinosa Villa Colibrí Therapeutic Community, Santiago, Cuba [email protected] Dilka Leyva Rodríguez Universidad de Oriente, Santiago, Cuba [email protected] Thalia Fuentes Leyva Universidad Técnica de Manabí, Portoviejo, Ecuador [email protected] Abstract When a critical analysis to date has made of, the historical aspects related to the topic of drugs, we could distinguish the existence of contrary positions regarding the possibility of legalizing them or not legalizing them. This dilemma is a very topical and important issue since opting for one position or another has economic, political and social implications that are necessary to keep track of. Therefore, the present study aims to; evaluate the advantages and disadvantages that would imply the legalization and non-legalization of drugs. Scientific journals from five years ago have consulted to date, theses and dissertations on the subject, digital and printed books that appear in libraries. Personal communication has made with researchers in the area of addictions. The main results were that the legalization of drugs is very dangerous for society due to its highly addictive and harmful effects on human beings. Likewise, specialists in addictions affirm that legalization can send the wrong message that consuming marijuana and other illegal drugs does not represent risks, which in turn can generate the wrong perception of safety and promote the promotion of consumption. -

Recommended Methods for the Identification and Analysis of Fentanyl and Its Analogues in Biological Specimens
Recommended methods for the Identification and Analysis of Fentanyl and its Analogues in Biological Specimens MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES Laboratory and Scientific Section UNITED NATIONS OFFICE ON DRUGS AND CRIME Vienna Recommended Methods for the Identification and Analysis of Fentanyl and its Analogues in Biological Specimens MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES UNITED NATIONS Vienna, 2017 Note Operating and experimental conditions are reproduced from the original reference materials, including unpublished methods, validated and used in selected national laboratories as per the list of references. A number of alternative conditions and substitution of named commercial products may provide comparable results in many cases. However, any modification has to be validated before it is integrated into laboratory routines. ST/NAR/53 Original language: English © United Nations, November 2017. All rights reserved. The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. Mention of names of firms and commercial products does not imply the endorse- ment of the United Nations. This publication has not been formally edited. Publishing production: English, Publishing and Library Section, United Nations Office at Vienna. Acknowledgements The Laboratory and Scientific Section of the UNODC (LSS, headed by Dr. Justice Tettey) wishes to express its appreciation and thanks to Dr. Barry Logan, Center for Forensic Science Research and Education, at the Fredric Rieders Family Founda- tion and NMS Labs, United States; Amanda L.A. -

UCSF UC San Francisco Previously Published Works
UCSF UC San Francisco Previously Published Works Title Fentanyl, fentanyl analogs and novel synthetic opioids: A comprehensive review Permalink https://escholarship.org/uc/item/8xh0s7nf Authors Armenian, Patil Vo, Kathy Barr-Walker, Jill et al. Publication Date 2017-10-01 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Fentanyl, fentanyl analogs and novel synthetic opioids: A comprehensive review Patil Armenian, Kathy Vo, Jill Barr-Walker, Kara Lynch University of California, San Francisco-Fresno and University of California, San Francisco Keywords: opioid, synthetic opioids, fentanyl, fentanyl analog, carfentanil, naloxone Abbreviations: 4-ANPP: 4-anilino-N-phenethyl-4-piperidine; ANPP 4Cl-iBF: 4-chloroisobutyryfentanyl 4F-iBF: 4-fluoroisobutyrfentanyl AEI: Advanced electronic information AMF: alpha-methylfentanyl CBP: US Customs and Border Protection CDC: Centers for Disease Control CDSA: Controlled Drug and Substance Act (Canada) CNS: central nervous system DEA: US Drug Enforcement Agency DTO: Drug trafficking organization ED: Emergency department ELISA: enzyme-linked immunosorbent assay EMCDDA: European Monitoring Centre for Drug and Drug Addiction FDA: US Food and Drug Administration GC-MS: gas chromatography mass spectrometry ICU: intensive care unit IN: intranasal IV: intravenous LC-HRMS: liquid chromatography high resolution mass spectrometry LC-MS/MS: liquid chromatography tandem mass spectrometry MDA: United Kingdom Misuse of Drugs Act NPF: non-pharmaceutical fentanyl THF-F: tetrahydrofuranfentanyl US: United States USPS: US Postal Service UNODC: United Nations office on drugs and crime 1. Introduction The death rate due to opioid analgesics nearly quadrupled in the US from 1999 to 2011 and was responsible for 33,091 deaths in 2015 (CDC, 2014; Rudd et al., 2016). -

Richard Nixon's Drug War: Politics Over Pragmatism
Richard Nixon's Drug War: Politics over Pragmatism Edmund Carlton April 20, 2012 Abstract: This thesis is an historical observation Richard Nixon's role as the instigator of America's Drug War. This Drug War is a war fought both against international drug smugglers and America's own citizens. This thesis will summarize some major trends of the politicization of the drug issue and give an in-depth analysis of how race played a role in both winning Richard Nixon the presidency in 1968 as well as how that victory has inflected itself back on to the American race dynamic. This thesis will utilize the substantial wealth of academic publications on the subject and will serve as a survey of sorts of the major drug politic academia discussing the years 1967-1972. I will also be utilizing films from this era in order to illustrate the social and race dynamic that were being negotiated in post-Civil Rights Act America. This thesis will utilize two primary documents from Richard Nixon, a Reader's Digest article from October, 1967, and a pivotal message to Congress given on July 14th, 1969 which accompanied the proposal of the Comprehensive Drug Abuse Prevention and Control Act which was passed a year later in 1970. Table of Contents Introduction P. 3 THE RELEVANT HISTORY OF DRUGS IN FILM p. 8 Its Racial Implications p.13 THE RHETORICAL PRE-AMBLE TO RICHARD NIXON's PRESIDENTIAL p.15 CAMPAIGN: The Reader Digest article "What Has Happened to America" White Backlash p. 22 RICHARD NIXON'S PIVOTAL MESSAGE TO CONGRESS p. -

Rethinking America's Illegal Drug Policy
NBER WORKING PAPER SERIES RETHINKING AMERICA'S ILLEGAL DRUG POLICY John J. Donohue III Benjamin Ewing David Peloquin Working Paper 16776 http://www.nber.org/papers/w16776 NATIONAL BUREAU OF ECONOMIC RESEARCH 1050 Massachusetts Avenue Cambridge, MA 02138 February 2011 The authors wish to thank Jonathan Caulkins, Phil Cook, Louis Kaplow, Rob MacCoun, Jeffrey Miron, Peter Reuter, and participants at two NBER conferences and the Harvard Law School Law and Economics workshop for valuable comments. We are also particularly grateful to Jeffrey Miron and Angela Dills for sharing their national time series data on drug prohibition enforcement and crime. The views expressed herein are those of the authors and do not necessarily reflect the views of the National Bureau of Economic Research. © 2011 by John J. Donohue III, Benjamin Ewing, and David Peloquin. All rights reserved. Short sections of text, not to exceed two paragraphs, may be quoted without explicit permission provided that full credit, including © notice, is given to the source. Rethinking America's Illegal Drug Policy John J. Donohue III, Benjamin Ewing, and David Peloquin NBER Working Paper No. 16776 February 2011, Revised March 2011 JEL No. K0 ABSTRACT This paper provides a critical review of the empirical and theoretical literatures on illegal drug policy, including cross-country comparisons, in order to evaluate three drug policy regimes: criminalization, legalization and “depenalization.” Drawing on the experiences of various states, as well as countries such as Portugal and the Netherlands, the paper attempts to identify cost-minimizing policies for marijuana and cocaine by assessing the differing ways in which the various drug regimes would likely change the magnitude and composition of the social costs of each drug. -
Questions and Answers on the Issue of a Regulated Market for Currently Illegal Drugs
Questions and answers on the issue of a regulated market for currently illegal drugs Mark Haden Vancouver Coastal Health Draft: June 2010 For the past decade I have been involved with public presentations which explore the failures of drug prohibition. In these presentations I recommend a public health, human rights model of drug control which brings all currently illegal drugs into a regulatory framework. The following is a list of the most common challenges I experience: Q: Are you saying that you want to legalize all drugs? A: No: Legalization is often interpreted to mean that the current capitalist free market system would be used to advertise and distribute currently illegal drugs. The goal of the free market is to increase consumption. The concept of a regulated market is different as the goal is to reduce the health and social problems associated with drugs. Q: What do you mean by a regulated market for illegal drugs? A: A regulated market would actively control drugs based on the principles of public health and human rights. Prohibition paradoxically stimulates a illegal market that makes concentrated and sometimes toxic, drugs widely available. The goal is to greatly reduce or shut down the illegal market and regulate drugs in a way that reduces harm to individuals, families and our society as a whole. Seeing drug use as primarily a health and social issue rather than a criminal issue allows us to explore a wide range of tools to manage the problems associated with drugs in a more effective way. Q: Are you saying “yes” to drugs? A: No – but we are saying “yes” to using more effective ways of controlling drugs and their problems. -

OCFENTANIL Critical Review Report Agenda Item 4.5
OCFENTANIL Critical Review Report Agenda Item 4.5 Expert Committee on Drug Dependence Thirty-ninth Meeting Geneva, 6-10 November 2017 39th ECDD (2017) Agenda item 4.5 Ocfentanil Page 2 of 17 39th ECDD (2017) Agenda item 4.5 Ocfentanil Contents Acknowledgements .......................................................................................................................... 5 Summary .......................................................................................................................................... 6 1. Substance identification ........................................................................................................... 7 A. International non-proprietary name (INN) ...................................................................................... 7 B. Chemical Abstract Service (CAS) registry number .......................................................................... 7 C. Other names ..................................................................................................................................... 7 D. Trade names ..................................................................................................................................... 7 E. Street names ..................................................................................................................................... 7 F. Physical properties ........................................................................................................................... 7 G. WHO review history ........................................................................................................................ -

Drug Prohibition and Its Alternatives John J. Donohue III Stanford Law School and NBER February 2014
Drug Prohibition and its Alternatives John J. Donohue III Stanford Law School and NBER February 2014 1. Introduction Illegal drugs, alcohol, and tobacco impose large social costs on society, here and in every major developed country. Interestingly, each of these is estimated -- albeit crudely -- to impose about $200 billion per year in social costs on the US (although the costs come in very different forms depending on the nature of the legal regime and enforcement policy). These three substances also share some interesting characteristics: many Americans have a serious attachment to one or more of them, and a sizeable proportion of the consumers use one or more of these in a responsible manner, hence imposing little-to-no external costs to society. The bad news is that a non-trivial subset also uses them irresponsibly, and this irresponsible use tends to create very high social costs. This problem is exacerbated by the fact that restricting use of drugs, alcohol, and tobacco to only those who impose minimal social costs is extremely difficult.1 Cocaine and opiates first became criminalized at the federal level in the United States in 1914, followed by marijuana in 1937. The criminalization of these drugs has led to the modern “war on drugs,” characterized by strict enforcement of drug violations and policing attempts directed at shutting down the drug trade. Scholars and policymakers, however, have questioned whether the “war on drugs” is really the optimal policy, with some suggesting that legalization and regulation may be a better alternative. A remarkable feature of this debate is that strong support exists for almost any position in the drug-policy debate. -
Methoxyacetylfentanyl
JOINT REPORTS ISSN 1977-7868 Methoxyacetylfentanyl EMCDDA–Europol Joint Report on a new psychoactive substance: 2-methoxy-N-phenyl-N-[1-(2-phenylethyl) piperidin-4-yl]acetamide (methoxyacetylfentanyl) In accordance with Article 5 of Council Decision 2005/387/JHA on the information exchange, risk assessment and control of new psychoactive substances About this series EMCDDA–Europol Joint Report publications examine the detailed information provided by the EU Member States on individual new psychoactive substances. Information is collected from the Reitox network, the Europol national units and the national competent authorities of the European Medicines Agency. Each Joint Report serves as the basis upon which the decision to conduct a risk assessment of the new psychoactive substance is taken. It is part of the three-step procedure involving information exchange, risk assessment and decision-making in the framework of Council Decision 2005/387/JHA. EMCDDA–Europol joint publication I Contents 3 I 1. Introduction 3 I 2. Information collection process 4 I 3. Information required by Article 5.2 of the Council Decision 4 I 3.1 Chemical and physical description, including the names under which the new psychoactive substance is known (Article 5.2(a) of the Council Decision) 6 I 3.2 Information on the frequency, circumstances and/or quantities in which a new psychoactive substance is encountered, and information on the means and methods of manufacture of the new psychoactive substance (Article 5.2(b) of the Council Decision) 6 I 3.2.1 Information -
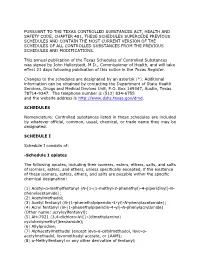
Schedules of Controlled Substances (.Pdf)
PURSUANT TO THE TEXAS CONTROLLED SUBSTANCES ACT, HEALTH AND SAFETY CODE, CHAPTER 481, THESE SCHEDULES SUPERCEDE PREVIOUS SCHEDULES AND CONTAIN THE MOST CURRENT VERSION OF THE SCHEDULES OF ALL CONTROLLED SUBSTANCES FROM THE PREVIOUS SCHEDULES AND MODIFICATIONS. This annual publication of the Texas Schedules of Controlled Substances was signed by John Hellerstedt, M.D., Commissioner of Health, and will take effect 21 days following publication of this notice in the Texas Register. Changes to the schedules are designated by an asterisk (*). Additional information can be obtained by contacting the Department of State Health Services, Drugs and Medical Devices Unit, P.O. Box 149347, Austin, Texas 78714-9347. The telephone number is (512) 834-6755 and the website address is http://www.dshs.texas.gov/dmd. SCHEDULES Nomenclature: Controlled substances listed in these schedules are included by whatever official, common, usual, chemical, or trade name they may be designated. SCHEDULE I Schedule I consists of: -Schedule I opiates The following opiates, including their isomers, esters, ethers, salts, and salts of isomers, esters, and ethers, unless specifically excepted, if the existence of these isomers, esters, ethers, and salts are possible within the specific chemical designation: (1) Acetyl-α-methylfentanyl (N-[1-(1-methyl-2-phenethyl)-4-piperidinyl]-N- phenylacetamide); (2) Acetylmethadol; (3) Acetyl fentanyl (N-(1-phenethylpiperidin-4-yl)-N-phenylacetamide); (4) Acryl fentanyl (N-(1-phenethylpiperidin-4-yl)-N-phenylacrylamide) (Other name: