Jemds.Com Original Research Article
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prevalence of Developmental Oral Mucosal Lesions Among a Sample of Denture Wearing Patients Attending College of Dentistry Clinics in Aljouf University
European Scientific Journal August 2016 edition vol.12, No.24 ISSN: 1857 – 7881 (Print) e - ISSN 1857- 7431 Prevalence Of Developmental Oral Mucosal Lesions Among A Sample Of Denture Wearing Patients Attending College Of Dentistry Clinics In Aljouf University Abdalwhab M.A .Zwiri Assistant professor of oral medicine, Aljouf University, Sakaka, Aljouf , Saudi Arabia Santosh Patil Assistant professor of Radiology, Aljouf University, Sakaka, Aljouf , Saudi Arabia Fadi AL- Omair Intern dentist, Aljouf University, Sakaka, Aljouf , Saudi Arabia Mohammed Assayed Mousa Lecturer of prosthodontics, Aljouf University, Sakaka, Aljouf , Saudi Arabia Ibrahim Ali Ahmad Department of Dentistry, AlWakra Hospital, Hamad Medical Corporation, AlWakra, Qatar doi: 10.19044/esj.2016.v12n24p352 URL:http://dx.doi.org/10.19044/esj.2016.v12n24p352 Abstract Introduction: developmental oral lesions represent a group of normal lesions that can be found at birth or evident in later life. These lesions include fissured and geographic tongue, Fordyce’s granules and leukoedema. Study aims: to investigate the prevalence of some developmental oral mucosal lesions among dental patients wearing dentures who were attending college of dentistry clinics in Aljouf University, and specialized dental center of ministry of health. Methods and subjects: a retrospective design was conducted to collect data from 344 wearing denture dental patients who were attending college of dentistry clinics in Aljouf University, and specialized dental center of ministry of health. A working excel sheet was created for patients and included data related to personal information such as age and gender; and oral developmental lesions. The software SPSS version 20 was used to analyze data. Statistical tests including frequency, percentages, and One way Anova were used to describe data. -

Update on Genital Dermatoses
UPDATE ON GENITAL DERMATOSES Sangeetha Sundaram Consultant GUM/HIV Southampton 07/11/2018 Normal variants • Fordyce spots • Vestibular papillae • Pearly penile papules • Angiokeratoma • Epidermal cysts • Skin tags Inflammatory dermatoses • Irritant dermatitis • Lichen sclerosus • Lichen simplex chronicus • Lichen planus • Seborrhoeic dermatitis • Psoriasis History • Itching? Where exactly? Waking up at night scratching? • Soreness/burning/raw? Where exactly? When? • Pain with sex? Where exactly? When exactly? • Discharge? • Skin trouble elsewhere? • Mouth ulcers? • Irritants in lifestyle Examination Irritants • Soap and shower gel (even Dove, Simple and Sanex…) • Sanitary pads and panty liners (especially when worn daily) • Moistened wipes • Synthetic underwear • Tight clothing • Feminine washes • Topical medication (creams and gels) • Urine, faeces, excessive vaginal discharge • Lubricants • Spermicides Basic vulval toolkit • Stop soap/shower gel (even Dove and Simple and Sanex!) • Stop pads/ panty liners (except during menses) • Loose cotton pants • Emollient soap substitute and barrier ointment Lichen simplex chronicus • Itching wakes her at night • Scratches in her sleep • Always same place(s) Lichen simplex chronicus - management • Stop soap/shower gel • Stop pads/ panty liners (except during menses) • Loose cotton pants • Emollient soap substitute and barrier ointment • Identify underlying condition(s), if any • Dermovate ointment every night for 2 weeks, then alternate nights for 2 weeks, then twice weekly for 2 weeks, then stop -

BIMJ April 2013
Original Article Brunei Int Med J. 2013; 9 (5): 290-301 Yellow lesions of the oral cavity: diagnostic appraisal and management strategies Faraz MOHAMMED 1, Arishiya THAPASUM 2, Shamaz MOHAMED 3, Halima SHAMAZ 4, Ramesh KUMARASAN 5 1 Department of Oral & Maxillofacial Pathology, Dr Syamala Reddy Dental College Hospital & Research Centre, Bangalore, India 2 Department of Oral Medicine & Radiology, Dr Syamala Reddy Dental College Hospital & Research Centre, Bangalore, India 3 Department of Community & Public Health Dentistry, Faculty of Dentistry, Amrita University, Cochin, India 4 Amrita center of Nanosciences, Amrita University, Cochin, India 5 Oral and Maxillofacial Surgery, Faculty of Dentistry, AIMST University, Kedah, Malaysia ABSTRACT Yellow lesions of the oral cavity constitute a rather common group of lesions that are encountered during routine clinical dental practice. The process of clinical diagnosis and treatment planning is of great concern to the patient as it determines the nature of future follow up care. There is a strong need for a rational and functional classification which will enable better understanding of the basic disease process, as well as in formulating a differential diagnosis. Clinical diagnostic skills and good judgment forms the key to successful management of yellow lesions of the oral cavity. Keywords: Yellow lesions, oral cavity, diagnosis, management INTRODUCTION INTRODUCTI Changes in colour have been traditionally low lesions have a varied prognostic spec- used to register and classify mucosal and soft trum. The yellowish colouration may be tissue pathology of the oral cavity. Thus, the- caused by lipofuscin (the pigment of fat). It se lesions have been categorised as white, may also be the result of other causes such red, white and red, blue and/or purple, as accumulation of pus, aggregation of lym- brown, grey and/or black and yellow. -

Fordyce's Granules Or Heterotopic/Ectopic Sebaceous Gland (Neville Et Al, 2009)
Republic of Iraq Ministry of Higher Education And scientific Research University of Baghdad College of Dentistry Fordyce’s granules A project submitted to the Council of the College of Dentistry at the University of Baghdad, Department of Oral Medicine, in partial fulfillment of the requirement for B.D.S. degree Done by: Zahraa Fakher Abd_Algany Supervisor RanaMurtadha Hassan )B.D.S., M.Sc( 2017-2018 List of content Subject Page NO. List of content I List of figures II List of table II Introduction 1 Aim of study 2 Chapter one: Review of literature 3 1.1 oral cavity 3 1.2 Definition 4 1.3 Epidemiology 4 1.4 etiology 5 1.5 Classification 5 1.6 clinical 6 1.7 Histology 8 1.8 Complications 10 1.9 Prognosis 10 1.10 Diagnosis and Treatment 11 1.10.1 Treatment of Fordyce Spots With CO2 Laser 11 1.10.2 bichloracetic acid 13 1.10.2.1 The Advantages of bichloracetic acid 13 treatment 1.10.2.2 Risk of bichloracetic acid treatment 14 1.10.3 5-aminolevulinic acid photodynamic therapy 15 1.10.3.1 Low cure rate in Fordyce spots by 5- 16 aminolevulinic acid photodynamic therapy is caused by Chapter two: Materials and methods 18 Chapter Three: RESULTS 19 3.1 Age 19 3.2 Gender 21 3.3 site 22 3.4 Geographic: 23 Chapter Four: Discussion 25 4.1 Age 25 4.2 site 25 4.3 Geographic 25 Chapter five :Conclusion 26 References 27 List of figure Fig. no. subject Page no. -

Fordyce's Disease Treated with Pimacrolimus: a Rare Case Report
CASE REPORT Fordyce's Disease Treated with Pimacrolimus: A Rare Case Report *T Hoque1, AZMM Islam2 ABSTRACT Fordyce's disease, a rarely found disease of lips has been reported recently in department of Skin and VD, Gonosashthaya Somaj Vittic Medical College Hospital, Savar, Dhaka. Occasionally it may not be possible to identify the cause. The patient presented with identical features of Fordyce's disease and lip biopsy for histopathology showed the features of Fordyce's disease. Then patient was treated with Pimecrolimus cream and improved. Fordyce's disease is an extremely rare disorder. So its cutaneous findings, histopathology and treatments are highlighted here. Key Words: Fordyce's disease, histopathology, Pimacrolimus. Introduction Fordyce's disease is ectopically located sebaceous common cause behind the condition. The glands, over mucous membrane of the mouth and development of yellowish papules and their location lips1,14, characterized by the presence of whitish or may indicate actopic sebaceous glands due to yellowish, scanty or abundant, discrete, aggravated abnormal disposition during embroyonic and often coalescent milium like bodies.2 It occurs development.5 Sometimes warts are mistakenly commonly inside of the mouth laterally along the diagnosed as Fordyce's condition, because of line of the teeth as far back as the last molar and similarity in involvement of vermilion border in both possibly somewhat less frequently on the vermilion cases.6 In cases the Fordyce's condition affected or mucous and inner surface of the lips, cheeks, less genital area that need for biopsy or blood often glans penis, labia mejora and minora.1,15 The examination considering the similarity in appearance lesions are from 1mm to 3 mm in size and usually of with some of Sexually transmitted diseases. -

Clinicopathologic Manifestations of Patients with Fordyce's Spots
Clinicopathologic Manifestations of Fordyce Spots Ann Dermatol Vol. 24, No. 1, 2012 http://dx.doi.org/10.5021/ad.2012.24.1.103 LETTER TO THE EDITOR Clinicopathologic Manifestations of Patients with Fordyce’s Spots Ji Hyun Lee, M.D., Ji Hae Lee, M.D., Na Hyun Kwon, M.D., Dong Soo Yu, M.D., Gyong Moon Kim, M.D., Chul Jong Park, M.D., Jeong Deuk Lee, M.D., Si Yong Kim, M.D. Department of Dermatology, College of Medicine, The Catholic University of Korea, Seoul, Korea Editor: The male to female ratio was 11:5. The average patient In 1896, Fordyce1 described whitish spots on the vermilion age was 34.3 years and ranged from 17∼67 years (mean± border of the lips, oral mucosa and, rarely, genital mu- S.D., 34.3±15.0 years). The average age was 41.1 years cosa. Fordyce’s spots are ectopically located sebaceous old in men and 19.4 years old in women. Duration of glands1-4. illness prior to diagnosis ranged from several days to five To date, few reports have been published to describe the years, and the mean incubation period was 1.9 years. clinicopathologic study of Fordyce’s spots in the Korean Most patients were asymptomatic. However, one patient population. We herein review the clinicopathologic cha- with concurrent contact dermatitis complained of pruritus. racteristics of Korean patients with Fordyce’s spots. The observed lesions were multi-centric and whitish to Data were collected retrospectively from the medical yellowish in color. Slightly elevated papules and plaques records of patients diagnosed with Fordyce’s spots bet- with sizes ranging from 1 to 3 mm were seen. -
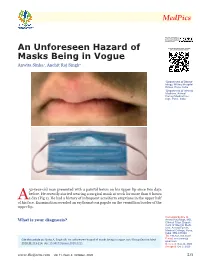
An Unforeseen Hazard of Masks Being in Vogue
An Unforeseen Hazard of Masks Being in Vogue Anwita Sinha1, Anchit Raj Singh2 1Department of Derma- tology, Military Hospital Kirkee, Pune, India 2Department of Internal Medicine, Armed Forces Medical Col- lege, Pune, India 32-year-old man presented with a painful lesion on his upper lip since two days before. He recently started wearing a surgical mask at work for more than 6 hours A a day (Fig 1). He had a history of infrequent acneiform eruptions in the upper half of his face. Examination revealed an erythematous papule on the vermillion border of the upper lip. Correspondence to What is your diagnosis? Anchit Raj Singh, MD, Clinical Tutor, Depart- ment of Internal Medi- cine, Armed Forces Medical College, Pune, India. PIN-411040 Tel: +91-841-103-8539 Cite this article as: Sinha A, Singh AR. An unforeseen hazard of masks being in vogue. Int J Occup Environ Med E-mail: anc.umars@ gmail.com 2020;11:213-214. doi: 10.34172/ijoem.2020.2211 Received: Sep 22, 2020 Accepted: Oct 3, 2020 www.theijoem.com Vol 11, Num 4; October, 2020 213 medpics Maskne continuous usage of masks for more than Maskne 6 hours is recommended; use of moistur- cne mechanica in the COVID-19 izers and face wash both before and after pandemic, colloquially known as wearing PPE are also beneficial. Use of A“maskne,” is a variant of facial der- protective dressings and alcohol-free liq- matosis seen in areas with friction from uid skin protectants can help reduce dam- use of masks, respirators, and personal age at pressure sites.6 protective equipment (PPE).1 Increased In our patient, the lesion was associ- levels of interleukin-1a, produced by fric- ated with friction over lips from prolonged tion, are implicated in the pathogenesis of use of a surgical mask, as evidenced by this disease.2 Maskne is a broad umbrella areas of wear on the mask (Fig 1). -

Clinical Characteristics of Oral Mucosal Lesions in Patients with Systemic Lupus Erythematosus and Their Association with Clinical and Laboratory Parameters
Clinical characteristics of oral mucosal lesions in patients with systemic lupus erythematosus and their association with clinical and laboratory parameters Lilly Esquivel-Pedraza 1, 2, Laura Fernández-Cuevas 3, Alba Cicero-Casarrubias 4, *, Sergio Ponce de León- Rosales 5, Mónica Fernández-Sánchez 1, 6, Rocío Orozco-Topete 1, 7, Carla Archer-Dubon 1, Ana Lilia Ruelas- Villavicencio 1, Marcela Saeb-Lima 8, Ma. Guadalupe Ortíz-Pedroza 1, Linda García-Hidalgo 1, Ma. Josefina Carbajosa-Martínez 1, María del Pilar Milke-García 9, Judith Domínguez-Chérit 1 and Silvia Méndez-Flores 1 1 Department of Dermatology, Instituto Nacional de Ciencias Médicas y Nutrición “Salvador Zubirán”, Mexico City, Mexico. 2 Department of Health Care, Universidad Autónoma Metropolitana. Mexico City, Mexico. 3 Oral Pathology Department, Centro Dermatológico “Dr. Ladislao de la Pascua”, Mexico City, Mexico. 4 Department of Immunology and Rheumatology, Instituto Nacional de Ciencias Médicas y Nutrición “Salvador Zubirán”, Mexico City, Mexico. 5 Department of Education, Instituto Nacional de Ciencias Médicas y Nutrición “Salvador Zubirán”, Mexico City, Mexico. 6 Centro de Investigación de Enfermedades Infecciosas. Instituto Nacional de Enfermedades Respiratorias, Mexico City, Mexico. 7 Hospital Médica Sur 8 Pathology Department, Instituto Nacional de Ciencias Médicas y Nutrición “Salvador Zubirán”, Mexico City, Mexico. 9 Nutrition Division. Instituto Nacional de Ciencias Médicas y Nutrición “Salvador Zubirán”, Mexico City, Mexico. GSC Advanced Research and Reviews, 2021, 06(02), 001–012 Publication history: Received on 22 January 2021; revised on 30 January 2021; accepted on 02 February 2021 Article DOI: https://doi.org/10.30574/gscarr.2021.6.2.0013 Abstract Introduction. Systemic lupus erythematosus (SLE) is an autoimmune disease that includes a broad spectrum of mucocutaneous manifestations. -

Dermatologic Manifestations of Stis Disclosures Objectives Outline
4/7/18 Disclosures • Research funding from: – NIH Dermatologic Manifestations of STIs – CDC – Becton-Dickenson Laura H. Bachmann, M.D., M.P.H – Atlas Genetics, Inc. Professor of Medicine, Wake Forest University Health Sciences Winston-Salem, NC Medical Director Guilford County Department of Health Objectives Outline At the end of this presentation, each participant will be able to: • What’s Normal? 1. Describe at least two normal variants commonly found on • What is not… genital examination – Flesh-colored papules – 2. Implement appropriate treatment for contact dermatitis Inflammatory plaques and papules – Vesicles, bullae and erosions 3. Utilize CDC recommended treatment approaches for the – White patches and plaques management of scabies infection – Non-infectious genital ulcers • Ectoparasites 1 4/7/18 Physiologic hyperpigmentation - Normal Normal Variants Perianal High-grade Dysplasia – Not Normal Angiokeratomas - Normal 2 4/7/18 Pearly Penile Papules (post-circumcision) Vestibular Papillae • Present in 1/3rd of women • Symmetrical • Rounded rather than acuminate tips • Discrete base • Rx - reassurance Edwards L and Lynch PJ. Genital Dermatology Atlas and Manual. 3rd Edition. Wolters Kluwer 2018 Fordyce Spots • Asymptomatic • Pin-point yellowish papules Flesh-colored papules • Normal sebaceous glands • Mucosal surfaces • Vermillion border of lips • No treatment Edwards L and Lynch PJ. Genital Dermatology Atlas and Manual. 3rd Edition. Wolters Kluwer 2018 3 4/7/18 ? Molluscum Molluscum Contagiosum • Poxvirus (molluscum bodies) • Asymptomatic, self-limited • Flesh-colored, smooth, umbilicated • Rx – liquid NO2, TCA, curettage, cantharidin, imiquimod, podophyllotoxin cream (0.5%), tretinoin, 10% KOH Edwards L and Lynch PJ. Genital Dermatology Atlas and Manual. 3rd Edition. Wolters Kluwer 2018 Disseminated cryptococcal infection Lichen Nitidus • Inflammatory skin disorder • No age, race or gender predominance • Asymptomatic • Tiny flesh or pink-colored papules • Appear follicular • Kobner phenomenon • Treatment: reassurance Edwards L and Lynch PJ. -
Cysts of the Oral and Maxillofacial Regions - LEK4R
Cysts of the Oral and Maxillofacial Regions - LEK4R http://lek4r.net/index.php?showtopic=11114&st=0 [26/3/2008 4:25:24 μμ] Cysts of the Oral and Maxillofacial Regions Fourth edition Mervyn Shear BDS, MDS, DSc (Dent), HDipDent, FRCPath, FRSSAf, LLD (hc), DChD (hc), Hon FCD (CMSA), Hon FCPath (CMSA) Professor Emeritus, University of the Witwatersrand, Johannesburg and Paul Speight BDS, PhD, FDRCPS (Glasg), FDSRCS (Eng), FDSRCS (Edin), FRCPath Professor of Oral Pathology, University of Sheffield © Shear & Speight 1976, 1983, 1992, 2007 Editorial offices: Blackwell Publishing Ltd, 9600 Garsington Road, Oxford OX4 2DQ, UK Tel: +44 (0)1865 776868 Blackwell Publishing Professional, 2121 State Avenue, Ames, Iowa 50014–8300, USA Tel: +1 515 292 0140 Blackwell Publishing Asia Pty Ltd, 550 Swanston Street, Carlton, Victoria 3053, Australia Tel: +61 (0)3 8359 1011 The right of the Author to be identified as the Author of this Work has been asserted in accordance with the Copyright, Designs and Patents Act 1988. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photo- copying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher. ISBN: 978-14051-4937-2 First edition published as Cysts of the Oral Regions by Butterworth-Heinemann 1976 Second edition 1983 Third edition 1992 Fourth edition, with amended title, published 2007 by Blackwell Munksgaard Library of Congress Cataloging-in-Publication Data Shear, Mervyn. Cysts of the oral and maxillofacial regions / Mervyn Shear and Paul Speight. -

Small White Spots on the Lips
PHOTO CHALLENGE Small White Spots on the Lips Peggy Rachel Cyr, MD, MS; Leigh Pemberton Johnson, MD A 27-year-old woman presented with multiple small white spots on the upper lip of several years’ duration. The lesions were slightly raised, nonpain- ful, nonpruritic, and nonpurulent. She had a history of tinea versicolor, acne vulgaris, and seborrheic dermatitis, with no history of tobacco use and no family history of skin disease. On physical exami- nation, she was afebrile and appeared healthy. More than 10 pale yellow, 1- to 2-mm papules were present oncopy the upper lip. WHAT’S THE DIAGNOSIS? a. Fordycenot granules b. granular cell tumors c. herpes simplex virus type 1 d. mucoceles Doe. oral leukoplakia PLEASE TURN TO PAGE E16 FOR THE DIAGNOSIS CUTIS Dr. Cyr is from Maine Medical Partners Portland Family Medicine. Dr. Johnson is from the Tufts University School of Medicine Maine Track, Maine Medical Center, Portland. The authors report no conflict of interest. Correspondence: Peggy Rachel Cyr, MD, MS, Maine Medical Partners Portland Family Medicine, 272 Congress St, Portland, ME 04101 ([email protected]). WWW.MDEDGE.COM/DERMATOLOGY VOL. 103 NO. 1 I JANUARY 2019 E15 Copyright Cutis 2019. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. PHOTO CHALLENGE DISCUSSION THE DIAGNOSIS: Fordyce Granules ordyce granules are prevalent benign anatomic of unknown etiology. It is a clinical diagnosis of exclusion. variations that occur in approximately 80% of the The patient may present with a hoarse voice and history F population.1 The spots usually present as multiple of tobacco use. -

Oral Medicine and Radiology
4A.4.2 SYLLABUS ( Including Teaching Hours.) MUST KNOW 1.Oral medicine and diagnostic AIDS: Section A-Diagnostic Methods 06 HRS (1) Definition and importance of Diagnosis and various types of diagnosis (2) Method of clinical examinations. (a) General Physical examination by inspection. (b) Oro-facial region by inspection, palpation and other means (c) To train the students about the importance, role, use of saliva and techniques of diagnosis of saliva as part of oral disease (d) Examination of lesions like swellings, ulcers, erosions, sinus, fistula, growths, pigmented lesions, white and red patches (e) Examination of lymph nodes (3) Investigations (a) Biopsy and exfoliative cytology (b) Hematological, Microbiological and other tests and investigations necessary for diagnosis and prognosis Section B- Diagnosis, Differential Diagnosis 04 HRS (1) Teeth: Developmental abnormalities, causes of destruction of teeth and their sequelae and discoloration of teeth (2) Inflamation – Injury, infection and sperad of infection,fascial space infections, osteoradionecrosis. (3) Temparomandibular joint: Developmental abnormalities of the condyle. Rheumatoid arthritis, Osteoarthritis, Subluxation and luxation. (4) Periodontal diseases: Gingival hyperplasia, gingivitis, periodontitis, pyogenic granuloma (5) Common cysts and Tumors: CYSTS: Cysts of soft tissue: Mucocele and Ranula 07 HRS Cysts of bone: Odontogenic and nonodontogenic. TUMORS: Soft Tissue: Epithelial: Papilloma, Carcinoma, Melanoma Connective tissue: Fibroma, Lipoma, Fibrosarcoma Vascular: Haemangioma, Lymphangioma Nerve Tissue: Neurofibroma, Traumatic Neuroma, Neurofibromatosis Salivary Glands: Pleomorphic adenoma, Adenocarcinoma, Warthin’s Tumor, Adenoid cystic carcinoma. (6) Teeth: Developmental abnormalities, causes of destruction of teeth and their sequelae and discoloration of teeth (7) Inflamation – Injury, infection and sperad of infection,fascial space infections, osteoradionecrosis. (8) Temparomandibular joint: Developmental abnormalities of the condyle.