Mastering the Care of the Hospitalized Patient
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Urology Residency Program of the Icahn School of Medicine at Mount Sinai
THE UROLOGY RESIDENCY PROGRAM OF THE ICAHN SCHOOL OF MEDICINE AT MOUNT SINAI Overview The Icahn School of Medicine at Mount Sinai Urology Residency Program is an ACGME-accredited program with a training format consisting of one year of preliminary training in general surgery followed by four years of urology. Its home institution is The Mount Sinai Hospital in New York City. The program is currently approved for a complement of five residents per training year. The program curriculum assures that over the course of training, every resident receives ample experience and didactic grounding in all of the core domains and techniques of urology while acquiring the professional skills and competencies that are characteristic of excellent physicians. Each of the rotations that comprise the curriculum include experience in both in-patient and out- patient treatment settings, with selected rotations offering concentrated experience in areas such as pediatric urology, urodynamics, endourology, female urology, infertility and oncology. An overarching schedule of conferences (led by faculty, fellow residents and guest lecturers), collaborative research projects and support for participation in professional organizations and special programs knit the residents’ clinical experience into the fabric of current urologic scholarship. Our home and affiliated institutions offer an immersive experience in three distinct health care delivery models: the tertiary care academic medical center, the community hospital and the municipal hospital system. Our graduates finish the program with an enviable understanding of the options that are open to them, and well equipped to pursue the urology careers of their choosing. Home and Affiliated Institutions The Mount Sinai Health System consists of seven hospital campuses, each of them a venerable New York institution, located in Manhattan, Brooklyn and Queens. -

2020-2021 Neurology Training at the Mount Sinai Hospital
2020-2021 Neurology Training at The Mount Sinai Hospital “The moment I stepped into the sun and tree-filled atrium of Mount Sinai Hospital, I knew I wanted to train here. The architectural thoughtfulness provides a respite for patients, families, and staff. In a similar way, the importance of emotional well-being is recognized by our program leaders. While residency is inherently challenging, our faculty cultivate a culture of support. During my Mount Sinai interview dinner, I remember overhearing several residents offer to cover an overnight shift for another resident so she could attend a family wedding. The kindness of my fellow residents and the beauty of our hospital inspire me every day.” – Bridget Mueller, Class of 2019 Contacts Barbara Vickrey, MD, MPH System Chair, Department of Neurology [email protected] Aaron Miller, MD Vice Chair for Education, Department of Neurology [email protected] Michelle Fabian, MD Residency Program Director [email protected] Laura K. Stein, MD, MPH Residency Program Associate Director [email protected] Faye Francisco Education Program Manager, Department of Neurology [email protected] 212-241-7074 Follow us on Twitter: @MSHSNeurology 2020-2021 Neurology Training at The Mount Sinai Hospital “I loved how just within the first 2 weeks of starting PGY 2, I felt as though I was already a part of the Mount Sinai Neurology family. Everyone I met has been so collegial, open, and friendly. Whether it was sharing stories during morning report or bonding while responding to stroke codes in the middle of the night, I couldn’t imagine a better start working with my co-residents and mentors.” - Kenneth Leung, Class of 2020 Contents Message from the Residency Program Directors 2 Welcome from the Chair and Vice Chair of Education 4 Department of Neurology 6 Our Commitment to Diversity and Inclusion 7 Neurology Divisions and Centers 8 Corinne Goldsmith Dickinson (CGD) Center for Multiple Sclerosis 8 Vascular Neurology Division 9 Robert and John M. -

Actions of the Council on Podiatric Medical Education
ACTIONS OF THE COUNCIL ON PODIATRIC MEDICAL EDUCATION April 2019 MEETING, MAIL BALLOTS, AND CONFERENCE CALLS March 1 – May 15, 2019 Approval as a PMSR (effective April 27, 2019) Coney Island Hospital, Brooklyn, New York 1/1/1 New York Community Hospital, Brooklyn, NY, 2/2/2 Approval as PMSR/RRA (effective April 27, 2019) Beaumont Hospital-Wayne, Wayne, MI, 3/3/3 Christus Saint Patrick Hospital, Lake Charles, LA, 1/1/1 Henry Ford Wyandotte Hospital, Wyandotte, MI, 3/3/3 Jackson South Community Hospital, Miami, FL, 1/1/1 James H. Quillen Veterans Affairs Medical Center, Mountain Home, TN, 1/1/1 John Peter Smith Hospital, Fort Worth, TX, 2/2/2 Kennedy University Hospital, Stratford, NJ, 3/3/3 Kingwood Medical Center, Kingwood, TX, 3/3/3 Mercy Health Regional Medical Center, Lorain, OH, 6/6/6 Mount Sinai Beth Israel Medical Center, New York, NY, 4/4/4/4 (The curriculum of the PMSR/RRA program requires completion of 48 months of training.) (effective July 1, 2019) NYU Winthrop Hospital, Mineola, NY, 2/2/2 Ochsner Clinic Foundation, New Orleans, LA, 3/3/3 Richmond University Medical Center, Staten Island, NY, 2/2/2 Roger Williams Medical Center, Providence, RI, 3/3/3 St. Vincent Evansville, Evansville, IN, 2/2/2 Surgical Hospital of Oklahoma, LLC and Cleveland Clinic Foundation, Oklahoma City, OK, 2/2/2 UnityPoint Health - Trinity Regional Medical Center, Fort Dodge, IA, 1/1/1 Veterans Affairs Puget Sound Health Care System, Seattle, WA, 2/2/2 Wake Forest Baptist Health, Winston-Salem, NC, 3/3/3 (effective July 1, 2019) Westchester General Hospital, Miami, FL, 4/4/4 White Memorial Medical Center, Los Angeles, CA, 2/2/2 Probation as PMSR/RRA (Candidate for withdrawal, effective July 1, 2020) Cooper University Hospital, Camden, NJ, 2/2/2 Fountain Valley Regional Hospital and Medical Center, Fountain Valley, CA, 1/1/1 Surgeons Choice Medical Center, Southfield, MI, 3/3/3 Rush University Medical Center, Chicago, IL, 3/3/3 Approval of Program Transfer Captain James A. -

The Urology Residency Program of the Icahn School of Medicine at Mount Sinai
THE UROLOGY RESIDENCY PROGRAM OF THE ICAHN SCHOOL OF MEDICINE AT MOUNT SINAI Overview The Icahn School of Medicine at Mount Sinai Urology Residency Program is an ACGME-accredited program with a training format consisting of one year of preliminary training in general surgery followed by four years of urology. Its home institution is The Mount Sinai Hospital in New York City. The program is currently approved for a complement of four residents per training year, though as a result of a recent merger with our sister program at Mount Sinai Beth Israel, the current enrollment includes four residents in the PGY 2 year, and five in each of PGY’s 3 through 5. The program curriculum assures that over the course of training, every resident receives ample experience and didactic grounding in all of the core domains and techniques of urology while acquiring the professional skills and competencies that are characteristic of excellent physicians. Each of the 19 rotations that comprise the curriculum include experience in both in-patient and out-patient treatment settings, with selected rotations offering concentrated experience in areas such as pediatric urology, urodynamics, endourology, female urology, infertility and oncology. An overarching schedule of conferences (led by faculty, fellow residents and guest lecturers), collaborative research projects and support for participation in professional organizations and special programs knit the residents’ clinical experience into the fabric of current urologic scholarship. Our home and affiliated institutions offer an immersive experience in three distinct health care delivery models: the tertiary care academic medical center, the community hospital and the municipal hospital system. -

Hispanic/Latino Heritage Month Banner.Indd
PROFILES OF FACULTY AND LEADERS Celebrating Hispanic/Latino Heritage NURSE EDUCATION MANAGER, MOUNT SINAI BROOKLYN MEDICAL DIRECTOR, AMBULATORY CARE, THE MOUNT SINAI HOSPITAL Cynthia Morales, MSN, RN Ms. Morales, who is of Puerto Rican heritage along Cameron R. Hernandez, MD with European, African, Indian, and Filipino ancestry, As a physician of Mexican and Scott ish descent, views diversity and inclusion as valuing each Dr. Hernandez views diversity and inclusion as individual’s diff erences and coming together to reach the organization’s greatest strength. As part of the a common goal. As an educator, her multicultural team spearheading the shi� from an individualized background has enabled her to bett er relate to and approach to a multi-disciplinary team approach in connect with students and colleagues on providing culturally competent caring for patients through the Mount Sinai Visiting care - a notion which is especially relevant in healthcare, where Doctors Program and ambulatory care clinics, he strongly supports understanding a patient’s beliefs o� en leads to bett er health outcomes. mentorship and creating opportunities for underrepresented populations - believing that diversity brings growth and enhances patient care. VICE CHAIR OF OPERATIONS, OBSTETRICS AND PLASTIC AND RECONSTRUCTIVE HEAD AND NECK SURGERY, GYNECOLOGY, MOUNT SINAI BETH ISRAEL NEW YORK EYE AND EAR INFIRMARY OF MOUNT SINAI Zoe I. Rodriguez, MD, FACOG Joseph J. Rousso, MD, FACS Dr. Zoe Rodriguez’s experiences as a fi rst-generation For Dr. Rousso, who spends most of his day American of Cuban and Venezuelan descent communicating in Spanish, his Cuban and Spanish have taught her the value of creating an inclusive heritage provides him the cultural awareness to environment for the talented clinicians and identify with and off er specialized care to patients administrators whom she recruits and supports. -
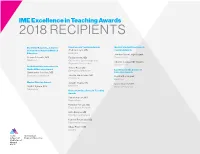
2018 Recipients
IME Excellence in Teaching Awards 2018 RECIPIENTS Dr. Arthur H. Aufses, Jr. Career Excellence in Teaching Awards Medical Student Excellence in Achievement Award in Medical Andrew Coyle, MD Teaching Awards Medicine Education Joe-Ann Moser, MD Student Steven Itzkowitz, MD Farida Nentin, MD Class of 2019 Medicine Obstetrics, Gynecology and Charles Sankey, MD Student Reproductive Science Class of 2020 Dr. Nathan Kase Innovations in Trevor Pour, MD Medical Education Award Emergency Medicine Excellence in the Service of Christopher Strother, MD Education Awards Emergency Medicine Jessica Reid-Adam, MD Cynthia Dominguez Pediatrics Medicine Master Clinician Award Joseph Truglio, MD Grace Oluoch, MBA DeWitt Pyburn, MD Medicine Medical Education Neurology House Staff Excellence in Teaching Awards Samira Farouk, MD Nephrology Hannibal Person, MD Triple Board Program Colin Pesyna, MD Emergency Medicine Kamron Pourmand, MD Gastroenterology Hillary Prince, MD Surgery IME Excellence in Teaching Awards 2016 RECIPIENTS Dr. Arthur H. Aufses, Jr. Career Excellence in Teaching Awards Medical Student Excellence in Achievement Award in Medical Andrew Alexis, MD, MPH Teaching Awards Education Dermatology Giselle Lynch, MD Student Scott H. Barnett, MD Carrie L. Ernst, MD Class of 2017 Pediatrics, Medical Education Psychiatry, Medical Education LGBTQ+ People in Medicine at Mount Sinai Master Clinician Award Craig L. Katz, MD Psychiatry, Medical Education Excellence in the Service of Steven Neustein, MD Education Awards Anesthesiology Staci A. Leisman, MD Renee Bischoff, MPH, LMSW Medicine, Medical Education Global Health Richard H. Stern, MD Rachel Pinotti, MLIS Radiology I nformation and Education House Staff Excellence in Services, Levy Library Teaching Awards Jeremy S. Faust, MD Emergency Medicine Parissa Tabrizian, MD Surgery IME Excellence in Teaching Awards 2015 RECIPIENTS Dr. -

Community Health Needs Assessment
Community Health Needs Assessment Prepared for THE MOUNT SINAI HOSPITAL The Mount Sinai Hospital Mount Sinai Queens By VERITÉ HEALTHCARE CONSULTING, LLC December 31, 2020 ABOUT VERITÉ HEALTHCARE CONSULTING Verité Healthcare Consulting, LLC (Verité) was founded in May 2006 and is located in Arlington, Virginia. The firm serves clients throughout the United States as a resource that helps health care providers conduct Community Health Needs Assessments and develop Implementation Strategies to address significant health needs. Verité has conducted more than 50 needs assessments for hospitals, health systems, and community partnerships nationally since 2010. The firm also helps hospitals, hospital associations, and policy makers with community benefit reporting, program infrastructure, compliance, and community benefit-related policy and guidelines development. Verité is a recognized national thought leader in community benefit and Community Health Needs Assessments. The community health needs assessment prepared for the Mount Sinai Hospital was directed by the firm’s Vice President with a senior associate supporting the work. The firm’s staff hold graduate degrees in relevant fields. More information on the firm and its qualifications can be found at www.VeriteConsulting.com. The Mount Sinai Hospital 1 Community Health Needs Assessment TABLE OF CONTENTS ABOUT VERITÉ HEALTHCARE CONSULTING ................................................................................................ 1 TABLE OF CONTENTS ........................................................................................................................................... -

The Transformation of Mount Sinai Beth Israel June 8Th Presentation Before PHHPC
The Transformation of Mount Sinai Beth Israel June 8th Presentation before PHHPC 1 Building to Meet Our Communities' Needs Mount Sinai Health System: Who We Are . Integrated Health System of 7 hospitals with more than 200 community locations . Anchored by a medical school . More than 150,000 inpatient admissions and more than 3 million outpatient visits . More than 2,000 residents – the largest teaching program in the country . 38,000 employees and 7,000 physicians . Provides significant care for Medicaid, Medicare, and patients eligible for financial assistance . Mount Sinai is 100% committed to serving all of their patients regardless of their financial situation 4+ million patient visits Largest Teaching Program in the U.S. 2 Building to Meet Our Communities' Needs The Reality at Mount Sinai Beth Israel . An aging and outmoded infrastructure . A rapidly decreasing inpatient census – dropping roughly 10% annually since 2012 . On average, more than 50% of the hospital’s licensed beds are unoccupied . MSBI has sustained losses of $350 Million over the past 4 years; if it were a stand-alone hospital, it would have already run out of cash . Rebuilding MSBI would require a $1.3 billion investment and ultimately not meet community’s evolving need for local access to care 3 Building to Meet Our Communities' Needs Trends in Healthcare . Hospital use is declining as patients get more care in non-hospital settings . 18 NYC hospitals closed over the past 13 years; many others are financially strapped . Government is prioritizing funding for coordinated care and treating patients in non- hospital settings . The rate of overall empty beds in NYC has increased in the past several years, despite hospital closures New York Hospitals in Critical Condition as Deficit Looms: Hospital stays citywide dropped over 5 percent between 2012 and 2014. -

June 4–9, 2021
THE SCIENCE OF TOMORROW STARTS TODAY ATC2021 VirtualCONNECT atcmeeting.org JUNE 4–9, 2021 Registration Brochure & Scientific Program DISCOUNTED REGISTRATION DEADLINE MAY 5, 2021 #ATC2021VirtualConnect ATC2021 VirtualCONNECT All-New Enhanced Experience! We are excited to announce ATC 2021 Virtual Live Connect, an all-new, completely enhanced virtual Broadcast Dates: meeting experience. Gain immediate access to innovators in the field and have your voice heard June 4 – 9, 2021 through various types of interaction Real-Time Interactivity Over 200 Education Credit The 2021 program will provide ample and Contact Hours opportunities for real-time interactivity through: ATC provides CME, ANCC, ACPE, and ABTC credits/contact hours. Yearlong access allows • Live Video Discussions you to take advantage of the over 200 • Invigorating Q&A Discussions Post- credits/contact hours available. This is the Presentation most credits/contact hours ATC has ever been • Live Presentations by Abstract Presenters able to provide! • Engaging, Unconventional Networking Breaks Continue to check the ATC website for final • Live Symposia Presentations credit/contact hour details, www.atcmeeting.org. Mobile Responsive Access In-Depth Symposia Included You’ll be able to access Virtual Connect on-the-go, in Virtual Connect earn your education credit or contact hours, hear Included with ATC 2021 Virtual Connect are the latest innovations, and build your professional 9 In-Depth Symposia. These symposia will be network – all from the comfort and safety of your live broadcasted on Friday, June 4, 2021, and home or office. then available in the OnDemand format until June 3, 2022. Yearlong Access to OnDemand Content Time Zone Schedule of By registering to attend ATC 2021 Virtual Connect, Program – Eastern Time Zone you also will gain yearlong access to all Live The program schedule is built in Eastern Time Broadcast sessions available in an OnDemand Zone. -

Milan B. Shah M.D
M ILAN B. SHAH M.D. ¡ ¢ £ ¤ ¥ ¦ § ¤ ¨ © ¥ ¤ © 722 45 th Street ! Brooklyn, NY 11220 ¦ © ¥ © ¦ ¢ (415) 234-3997 ! [email protected] EDUCATION & EMPLOYMENT UROLOGY GROUP OF SOUTHERN CALIFORNIA , Los Angeles, CA 8/2019 ¥ Attending Urologist LOMA LINDA UNIVERSITY MEDICAL CENTER , Loma Linda, CA 7/2018 Ð 7/2019 ¥ Fellow in Endourology & Urinary Stone Disease, Department of Urology MOUNT SINAI HOSPITAL , Icahn School of Medicine at Mount Sinai, New York, NY 7/2014 Ð 6/2018 ¥ PGY-2, PGY-3, PGY-4 & PGY-5 (Chief Resident), Department of Urology MOUNT SINAI BETH ISRAEL , Icahn School of Medicine at Mount Sinai, New York, NY 7/2013 Ð 6/2014 ¥ Intern, Department of General Surgery SUNY DOWNSTATE COLLEGE OF MEDICINE , Brooklyn, NY 8/2009 Ð 5/2013 ¥ M.D. UNIVERSITY OF PENNSYLVANIA , Philadelphia, PA 9/2005 Ð 5/2008 ¥ B.A. Biological Basis of Behavior, magna cum laude ¥ GPA 3.75 BOSTON UNIVERSITY , Boston, MA 9/2004 Ð 5/2005 ¥ GPA 3.84 PROFESSIONAL EXPERIENCE GOOGLE INCORPORATED , People Operations, Mountain View, CA 8/2008 Ð 8/2009 Reporting and Analytics ¥ Used Microstrategy and PeopleView, reporting and analysis tools, to pull and analyze company data ¥ Provided technical support to over 100 Microstrategy and PeopleView users Google Health ¥ Organized vaccination schedules for the Google health website RWTH AACHEN UNIVERSITY , Department of Neuropsychiatry, Aachen, Germany 6/2007 Ð 9/2007 Research Assistant ¥ Conducted electroencephalography (EEG) on study participants to determine the influence of the visual sensory modality on auditory motion perception; Mentor: Mikhail Zvyagintsev, M.D . UNIVERSITY OF PENNSYLVANIA , Department of Chemistry, Philadelphia, PA 9/2006 Ð 1/2007 Research Assistant ¥ Helped develop innovative technique which reduces amount of catalysts that end up in polymer products, enabling greater commercial usage; Mentor: Virgil Percec, Ph.D. -

Beth Israel OB-GYN | Midwives in Hospitals
Our Midwives | Beth Israel OB-GYN | Midwives in Hospitals Welcome To Our Practice Locations Our Services Bios Education Billing Contact Us Our Midwives Since its inception more than 30 years ago, our Midwifery Services program has grown to become one of the largest services of its kind in New York State. Educated in two professional disciplines - nursing and midwifery - our midwives are all certified by the American College of Nurse Midwives. They manage normal labor and deliveries as well as offering a wide range of well-woman gynecological services. Our gynecological services include: Routine physical exams Pap smears Breast exams Our obstetrical services include: Family planning Prenatal care Labor and delivery Drug prescription Management of normal pregnancies Breastfeeding assistance With a midwife, you can remain at home as long as possible. Your midwife will coach you over the phone through the beginning of labor until you arrive at the hospital. At that point, she will stay with you and manage your pregnancy through your delivery. If the midwife needs assistance at any time, Beth Israel physicians are stationed on the labor floor around-the-clock to help. Meet our Midwives Rochelle Lipshutz attended the State University of New York at Downstate for her midwifery certification. She has been a part of the Beth Israel Ob/Gyn Midwifery Associates since 1989 and has been its director since 1999. As director, she has significantly contributed to developing the BIMC Midwifery Practice into a family- centered, comprehensive, maternal-child health. Joyce Griffin, a graduate of Columbia University’s Midwifery Program, joined the Beth Israel Ob/Gyn Midwifery Associates in 1991. -

Career Day 2018
C A M S 4 T H A N N U A L M E D I C A L S T U D E N T S C A R E E R D A Y S E P T 8 2 0 1 8 9 : 0 0 A M - 1 : 3 0 P M W E I L L C O R N E L L M E D I C I N E | W E I L L A U D I T O R I U M SPONSORED BY WEILL CORNELL MEDICINE & NEW YORK-PRESBYTERIAN LOWER MANHATTAN HOSPITAL BROUGHT TO YOU BY CHINESE AMERICAN MEDICAL SOCIETY IN PARTNERSHIP WITH THE ASIAN SERVICE PROGRAMS AT MAIMONIDES MEDICAL CENTER, MOUNT SINAI BETH ISRAEL, NEWYORK-PRESBYTERIAN BROOKLYN METHODIST HOSPITAL, NEWYORK-PRESBYTERIAN LOWER MANHATTAN HOSPITAL, AND NEWYORK-PRESBYTERIAN QUEENS PLANNING COMMITTEE Co-Chair: Wan Ling Lam, MD Co-Chair: Yick Moon Lee, MD Benjamin Lee, MD Steven Cai, MD John Paul Tracy Ng, MD Warren W. Chin, MD Shan-Chin (Winson) Chen, MD Yu Shia Lin, MD Janice Yang (Maimonides Medical Center) Lucia Chan (Mount Sinai Beth Israel) Frances L. Wong, LCSW (NewYork-Presbyterian Brooklyn Methodist Hospital) Chui-Man Lai (NewYork-Presbyterian Lower Manhattan Hospital) Ada Wong, RHIA (NewYork-Presbyterian Lower Manhattan Hospital) Ming-der Chang, PhD (NewYork-Presbyterian Queens) Billy Yang (SUNY Downstate Medical Center, College of Medicine) Diana Cheung (NYIT College of Osteopathic Medicine) Jack Liu (Albert Einstein College of Medicine) Jessica Tan (Icahn School of Medicine at Mount Sinai) Michael Chen (SUNY Downstate Medical Center, College of Medicine) Ryan Pang (SUNY Downstate Medical Center, College of Medicine) Samantha Ho (A.T.