Effects on the Pituitary–Adrenal Axis in Rhesus Monkeys
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Midazolam Injection, USP
Midazolam Injection, USP 2 mg per 2 mL | NDC 70860-600-02 50 mg per 10 mL | NDC 70860-601-10 ATHENEX AccuraSEETM PACKAGING AND LABELING BIG, BOLD AND BRIGHT — TO HELP YOU SEE IT, SAY IT AND PICK IT RIGHT DIFFERENTIATION IN EVERY LABEL, DESIGNED TO HELP REDUCE MEDICATION ERRORS PLEASE SEE FULL PRESCRIBING INFORMATION, INCLUDING BOXED WARNING, FOR MIDAZOLAM INJECTION, USP, ENCLOSED. THE NEXT GENERATION OF PHARMACY INNOVATION To order, call 1-855-273-0154 or visit www.Athenexpharma.com Midazolam Injection, USP 2 5 mg NDC 70860-600-02 0 NDC 70860-601-10 2 mg per 2 mL mg 50 mg per 10 mL DESCRIPTION Glass Vial DESCRIPTION Glass Vial CONCENTRATION 1 mg per mL CONCENTRATION 5 mg per mL CLOSURE 13 mm CLOSURE 20 mm UNIT OF SALE 25 vials UNIT OF SALE 10 vials BAR CODED Yes BAR CODED Yes STORAGE Room Temp. STORAGE Room Temp. • AP RATED • PRESERVATIVE-FREE • AP RATED • NOT MADE WITH NATURAL RUBBER LATEX • NOT MADE WITH NATURAL RUBBER LATEX CHOOSE AccuraSEETM FOR YOUR PHARMACY Our proprietary, differentiated and highly-visible label designs can assist pharmacists in accurate medication selection. With a unique label design for every Athenex product, we’re offering your pharmacy added AccuraSEE. The idea is simple: “So what you see is exactly what you get.” Athenex, AccuraSEE and all label designs are copyright of Athenex. ©2020 Athenex. 000527 To order, call 1-855-273-0154 or visit www.Athenexpharma.com • Midazolam hydrochloride mufti-dose vial, is not intended for intrathecal or epidural • Anesthetic and sedation drugs are a necessary part of the care of children needing Midazolam Injection, USP administration, and is contraindicated for use in premature infants, because the formulation surgery, other procedures, or tests that cannot be delayed, and no specific medications INDICATIONS AND USAGE contains benzyl alcohol as a preservative. -

Determination of Barbiturates and 11-Nor-9-Carboxy-Δ9-THC in Urine
Determination of Barbiturates and 11-Nor-9-carboxy- 9-THC in Urine using Automated Disposable Pipette Extraction (DPX) and LC/MS/MS Fred D. Foster, Oscar G. Cabrices, John R. Stuff, Edward A. Pfannkoch GERSTEL, Inc., 701 Digital Dr. Suite J, Linthicum, MD 21090, USA William E. Brewer Department of Chemistry and Biochemistry, University of South Carolina, 631 Sumter St. Columbia, SC 29208, USA KEYWORDS DPX, LC/MS/MS, Sample Preparation, High Throughput Lab Automation ABSTRACT This work demonstrates the use of disposable pipette extraction (DPX) as a fast and automated sample preparation technique for the determination of barbiturates and 11-nor-9- carboxy- 9-THC (COOH-THC) in urine. Using a GERSTEL MultiPurpose Sampler (MPS) with DPX option coupled to an Agilent 6460 LC-MS/MS instrument, 8 barbiturates and COOH-THC were extracted and their concentrations determined. The resulting average cycle time of 7 min/ sample, including just-in-time sample preparation, enabled high throughput screening. Validation results show that the automated DPX-LC/ AppNote 1/2013 MS/MS screening method provides adequate sensitivity for all analytes and corresponding internal standards that were monitored. Lower limits of quantitation (LLOQ) were found to be 100 ng/mL for the barbiturates and 10 ng/mL for COOH-THC and % CVs were below 10 % in most cases. INTRODUCTION The continuously growing quantity of pain management sample extract for injection [1-2]. The extraction of the drugs used has increased the demand from toxicology Barbiturates and COOH-THC is based on the DPX-RP- laboratories for more reliable solutions to monitor S extraction method described in an earlier Application compliance in connection with substance abuse and/or Note detailing monitoring of 49 Pain Management diversion. -

Veterinary Anesthetic and Analgesic Formulary 3Rd Edition, Version G
Veterinary Anesthetic and Analgesic Formulary 3rd Edition, Version G I. Introduction and Use of the UC‐Denver Veterinary Formulary II. Anesthetic and Analgesic Considerations III. Species Specific Veterinary Formulary 1. Mouse 2. Rat 3. Neonatal Rodent 4. Guinea Pig 5. Chinchilla 6. Gerbil 7. Rabbit 8. Dog 9. Pig 10. Sheep 11. Non‐Pharmaceutical Grade Anesthetics IV. References I. Introduction and Use of the UC‐Denver Formulary Basic Definitions: Anesthesia: central nervous system depression that provides amnesia, unconsciousness and immobility in response to a painful stimulation. Drugs that produce anesthesia may or may not provide analgesia (1, 2). Analgesia: The absence of pain in response to stimulation that would normally be painful. An analgesic drug can provide analgesia by acting at the level of the central nervous system or at the site of inflammation to diminish or block pain signals (1, 2). Sedation: A state of mental calmness, decreased response to environmental stimuli, and muscle relaxation. This state is characterized by suppression of spontaneous movement with maintenance of spinal reflexes (1). Animal anesthesia and analgesia are crucial components of an animal use protocol. This document is provided to aid in the design of an anesthetic and analgesic plan to prevent animal pain whenever possible. However, this document should not be perceived to replace consultation with the university’s veterinary staff. As required by law, the veterinary staff should be consulted to assist in the planning of procedures where anesthetics and analgesics will be used to avoid or minimize discomfort, distress and pain in animals (3, 4). Prior to administration, all use of anesthetics and analgesic are to be approved by the Institutional Animal Care and Use Committee (IACUC). -

International Classification of Diseases
INTERNATIONAL CLASSIFICATION OF DISEASES MANUAL OF THE INTERNATIONAL STATISTICAL CLASSIFICATION OF DISEASES, INJURIES, AND CAUSES OF DEATH Based on the Recommendations of the Eighth Revision Conference, 1965, and Adopted by the Nineteenth World Health Assembly Volume 2 ALPHABETICAL INDEX WORLD HEALTH ORGANIZATION GENEVA 1969 Volume 1 Introduction List of Three-digit Categories Tabular List of Inclusions and Four-digit Sub- categories Medical Certification and Rules for Classification Special Lists for Tabulation Definitions and Recommendations Regulations Volume 2 Alphabetical Index PRINTED IN ENGLAND CONTENTS Introduction Page General arrangement of the Index ....................................... VIII Main sections ............................................................... VIII Structure ..................................................................... IX Code numbzrs .............................................................. x Primary and secondary conditions. ................................... x Multiple diagnoses. ........................................................ XI Spelling....................................................................... XI Order of listing ............................................................. Conventions used in the Index ........................................... XII Parentheses. ................................................................. XII Cross-referexes ........................................................... XI1 Abbreviation NEC. ...................................................... -

The Emergence of New Psychoactive Substance (NPS) Benzodiazepines
Issue: Ir Med J; Vol 112; No. 7; P970 The Emergence of New Psychoactive Substance (NPS) Benzodiazepines. A Survey of their Prevalence in Opioid Substitution Patients using LC-MS S. Mc Namara, S. Stokes, J. Nolan HSE National Drug Treatment Centre Abstract Benzodiazepines have a wide range of clinical uses being among the most commonly prescribed medicines globally. The EU Early Warning System on new psychoactive substances (NPS) has over recent years detected new illicit benzodiazepines in Europe’s drug market1. Additional reference standards were obtained and a multi-residue LC- MS method was developed to test for 31 benzodiazepines or metabolites in urine including some new benzodiazepines which have been classified as New Psychoactive Substances (NPS) which comprise a range of substances, including synthetic cannabinoids, opioids, cathinones and benzodiazepines not covered by international drug controls. 200 urine samples from patients attending the HSE National Drug Treatment Centre (NDTC) who are monitored on a regular basis for drug and alcohol use and which tested positive for benzodiazepine class drugs by immunoassay screening were subjected to confirmatory analysis to determine what Benzodiazepine drugs were present and to see if etizolam or other new benzodiazepines are being used in the addiction population currently. Benzodiazepine prescription and use is common in the addiction population. Of significance we found evidence of consumption of an illicit new psychoactive benzodiazepine, Etizolam. Introduction Benzodiazepines are useful in the short-term treatment of anxiety and insomnia, and in managing alcohol withdrawal. 1 According to the EMCDDA report on the misuse of benzodiazepines among high-risk opioid users in Europe1, benzodiazepines, especially when injected, can prolong the intensity and duration of opioid effects. -

Drug and Medication Classification Schedule
KENTUCKY HORSE RACING COMMISSION UNIFORM DRUG, MEDICATION, AND SUBSTANCE CLASSIFICATION SCHEDULE KHRC 8-020-1 (11/2018) Class A drugs, medications, and substances are those (1) that have the highest potential to influence performance in the equine athlete, regardless of their approval by the United States Food and Drug Administration, or (2) that lack approval by the United States Food and Drug Administration but have pharmacologic effects similar to certain Class B drugs, medications, or substances that are approved by the United States Food and Drug Administration. Acecarbromal Bolasterone Cimaterol Divalproex Fluanisone Acetophenazine Boldione Citalopram Dixyrazine Fludiazepam Adinazolam Brimondine Cllibucaine Donepezil Flunitrazepam Alcuronium Bromazepam Clobazam Dopamine Fluopromazine Alfentanil Bromfenac Clocapramine Doxacurium Fluoresone Almotriptan Bromisovalum Clomethiazole Doxapram Fluoxetine Alphaprodine Bromocriptine Clomipramine Doxazosin Flupenthixol Alpidem Bromperidol Clonazepam Doxefazepam Flupirtine Alprazolam Brotizolam Clorazepate Doxepin Flurazepam Alprenolol Bufexamac Clormecaine Droperidol Fluspirilene Althesin Bupivacaine Clostebol Duloxetine Flutoprazepam Aminorex Buprenorphine Clothiapine Eletriptan Fluvoxamine Amisulpride Buspirone Clotiazepam Enalapril Formebolone Amitriptyline Bupropion Cloxazolam Enciprazine Fosinopril Amobarbital Butabartital Clozapine Endorphins Furzabol Amoxapine Butacaine Cobratoxin Enkephalins Galantamine Amperozide Butalbital Cocaine Ephedrine Gallamine Amphetamine Butanilicaine Codeine -

A Fast Analytical LC/MS/MS Method for the Simultaneous Analysis of Barbiturates and 11-Nor-9-Carboxy-Δ9- Tetrahydrocannabinol (THC-A) in Urine
Application Note Clinical Research A Fast Analytical LC/MS/MS Method for the Simultaneous Analysis of Barbiturates and 11-nor-9-carboxy-Δ9- tetrahydrocannabinol (THC-A) in Urine Using ESI negative ionization mode and alternating column regeneration Authors Abstract Andre Szczesniewski and Most of the compounds in large drug panels are analyzed using positive ionization Carrie J. Adler mode. However, barbiturates and 11-nor-9-carboxy-Δ9-THC (THC-A) perform better Agilent Technologies, Inc. using electrospray ionization (ESI) in negative mode with the mobile phase pH favorable for negative ionization. This work developed a fast analytical method combining eight barbiturates and THC-A in a single analysis using alternating column regeneration (ACR) to increase sample throughput. Moving the analytes preferring negative ionization into a separate test increases the analytical sensitivity of the compounds, allowing for greater research capabilities. The simple sample preparation techniques used provided rapid analysis, good analytical sensitivity, and quantitation over a wide dynamic range. This analysis used an Agilent 6470 triple quadrupole mass spectrometer with Agilent Jet Stream technology in ESI negative ionization mode and an Agilent Infinity II 1290 UHPLC system. A second pump and 2-position 10-port switching valve were added to facilitate use of the ACR. A 100 µL aliquot of human urine was used for the analysis of barbiturates and THC-A. Chromatographic separation of the analytes was achieved in less than 3 minutes using a gradient method composed of a H2O:acetonitrile mixture with 5 mM ammonium acetate and two Agilent Poroshell 120 EC-C18, 2.1 × 100 mm, 1.9 μm columns. -
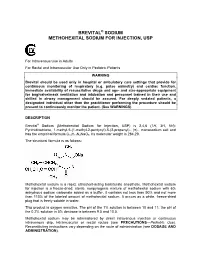
Brevital Sodium Methohexital Sodium for Injection
BREVITAL® SODIUM METHOHEXITAL SODIUM FOR INJECTION, USP For Intravenous Use in Adults For Rectal and Intramuscular Use Only in Pediatric Patients WARNING Brevital should be used only in hospital or ambulatory care settings that provide for continuous monitoring of respiratory (e.g. pulse oximetry) and cardiac function. Immediate availability of resuscitative drugs and age- and size-appropriate equipment for bag/valve/mask ventilation and intubation and personnel trained in their use and skilled in airway management should be assured. For deeply sedated patients, a designated individual other than the practitioner performing the procedure should be present to continuously monitor the patient. (See WARNINGS) DESCRIPTION Brevital® Sodium (Methohexital Sodium for Injection, USP) is 2,4,6 (1H, 3H, 5H)- Pyrimidinetrione, 1-methyl-5-(1-methyl-2-pentynyl)-5-(2-propenyl)-, (±)-, monosodium salt and has the empirical formula C14H17N2NaO3. Its molecular weight is 284.29. The structural formula is as follows: Methohexital sodium is a rapid, ultrashort-acting barbiturate anesthetic. Methohexital sodium for injection is a freeze-dried, sterile, nonpyrogenic mixture of methohexital sodium with 6% anhydrous sodium carbonate added as a buffer. It contains not less than 90% and not more than 110% of the labeled amount of methohexital sodium. It occurs as a white, freeze-dried plug that is freely soluble in water. This product is oxygen sensitive. The pH of the 1% solution is between 10 and 11; the pH of the 0.2% solution in 5% dextrose is between 9.5 and 10.5. Methohexital sodium may be administered by direct intravenous injection or continuous intravenous drip, intramuscular or rectal routes (see PRECAUTIONS—Pediatric Use). -

The Waterloo Wellington Palliative Sedation Protocol
The Waterloo Wellington Palliative Sedation Protocol Waterloo Wellington Interdisciplinary HPC Education Committee; PST Task Force Chair: Dr. Deborah Robinson MD CCFP(F), Focused practice in Oncology and Palliative Care Co-chairs: Cathy Joy, Palliative Care Consultant, Waterloo Region Chris Bigelow, Palliative Care Consultant, Wellington County Revision due: November 2016 Last revised and activated: November 13, 2013 Committee responsible for revisions: WW Interdisciplinary HPC Education Committee Table of Contents Purpose and Definitions .................................................................................................................... 2 Indications for the use of PST .............................................................................................................. 3 Criteria for Initiation of PST ............................................................................................................... 4 Process ............................................................................................................................................. 4 Documentation for Initiation of PST .................................................................................................. 5 Medications ......................................................................................................................................... 6 1st Line (Initiating PST) ...................................................................................................................... 6 2nd Line (When 1st -

Chloral Hydrate: Summary Report
Chloral Hydrate: Summary Report Item Type Report Authors Yuen, Melissa V.; Gianturco, Stephanie L.; Pavlech, Laura L.; Storm, Kathena D.; Yoon, SeJeong; Mattingly, Ashlee N. Publication Date 2020-02 Keywords Compounding; Food, Drug, and Cosmetic Act, Section 503B; Food and Drug Administration; Outsourcing facility; Drug compounding; Legislation, Drug; United States Food and Drug Administration; Chloral Hydrate Rights Attribution-NoDerivatives 4.0 International Download date 26/09/2021 09:06:16 Item License http://creativecommons.org/licenses/by-nd/4.0/ Link to Item http://hdl.handle.net/10713/12087 Summary Report Chloral Hydrate Prepared for: Food and Drug Administration Clinical use of bulk drug substances nominated for inclusion on the 503B Bulks List Grant number: 2U01FD005946 Prepared by: University of Maryland Center of Excellence in Regulatory Science and Innovation (M-CERSI) University of Maryland School of Pharmacy February 2020 This report was supported by the Food and Drug Administration (FDA) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award (U01FD005946) totaling $2,342,364, with 100 percent funded by the FDA/HHS. The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement by, the FDA/HHS or the U.S. Government. 1 Table of Contents REVIEW OF NOMINATION ..................................................................................................... 4 METHODOLOGY ................................................................................................................... -

Midazolam Injection, USP
Midazolam Injection, USP Rx only PHARMACY BULK PACKAGE – NOT FOR DIRECT INFUSION WARNING ADULTS AND PEDIATRICS: Intravenous midazolam has been associated with respiratory depression and respiratory arrest, especially when used for sedation in noncritical care settings. In some cases, where this was not recognized promptly and treated effectively, death or hypoxic encephalopathy has resulted. Intravenous midazolam should be used only in hospital or ambulatory care settings, including physicians’ and dental offices, that provide for continuous monitoring of respiratory and cardiac function, i.e., pulse oximetry. Immediate availability of resuscitative drugs and age- and size-appropriate equipment for bag/valve/mask ventilation and intubation, and personnel trained in their use and skilled in airway management should be assured (see WARNINGS). For deeply sedated pediatric patients, a dedicated individual, other than the practitioner performing the procedure, should monitor the patient throughout the procedures. The initial intravenous dose for sedation in adult patients may be as little as 1 mg, but should not exceed 2.5 mg in a normal healthy adult. Lower doses are necessary for older (over 60 years) or debilitated patients and in patients receiving concomitant narcotics or other central nervous system (CNS) depressants. The initial dose and all subsequent doses should always be titrated slowly; administer over at least 2 minutes and 1 allow an additional 2 or more minutes to fully evaluate the sedative effect. The dilution of the 5 mg/mL formulation is recommended to facilitate slower injection. Doses of sedative medications in pediatric patients must be calculated on a mg/kg basis, and initial doses and all subsequent doses should always be titrated slowly. -

Barbiturates
URINE DRUG TEST INFORMATION SHEET BARBITURATES Classification: Central nervous system depressants insomnia, anxiety or tension due to their very high (CNS Depressants) risk of physical dependence and fatal overdose. Due to the structural nature of barbiturates, the duration Background: Barbiturates are a group of drugs of action does not always correlate well with the that act as central nervous system depressants. biological half-life. Opiates, benzodiazepines and alcohol are also CNS depressants, and like their use, the effect seems to Physiological Effects: Lowered blood pressure, the user as an overall sense of calm. Barbiturates respiratory depression, fatigue, fever, impaired were introduced in 1903, dominating the sedative- coordination, nystagmus, slurred speech and ataxia hypnotic market for the first half of the twentieth century. Unfortunately, because barbiturates have Psychological Effects: Drowsiness, dizziness, unusual a relatively low therapeutic-to-toxic index and excitement, irritability, poor concentration, sedation, substantial potential for abuse, they quickly became confusion, impaired judgment, addiction, euphoria, a major health problem. Barbiturates are commonly decreased anxiety and a loss of inhibition abused for their sedative properties and widespread Toxicity: Barbiturates are especially more availability. The introduction of benzodiazepines in dangerous when abused with alcohol, opiates and the 1960s quickly supplanted the barbiturates due benzodiazepines because they act on the same to their higher safety