Building Resilient Health Systems: Lessons from International, National
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Local Council Ward Boundary Delimitation Report
April 2008 NATIONAL ELECTORAL COMMISSION Sierra Leone Local Council Ward Boundary Delimitation Report Volume One February 2008 This page is intentionally left blank TABLE OF CONTENTS Foreword 1 Executive Summary 3 Introduction 5 Stages in the Ward Boundary Delimitation Process 7 Stage One: Establishment of methodology including drafting of regulations 7 Stage Two: Allocation of Local Councils seats to localities 13 Stage Three: Drawing of Boundaries 15 Stage Four: Sensitization of Stakeholders and General Public 16 Stage Five: Implement Ward Boundaries 17 Conclusion 18 APPENDICES A. Database for delimiting wards for the 2008 Local Council Elections 20 B. Methodology for delimiting ward boundaries using GIS technology 21 B1. Brief Explanation of Projection Methodology 22 C. Highest remainder allocation formula for apportioning seats to localities for the Local Council Elections 23 D. List of Tables Allocation of 475 Seats to 19 Local Councils using the highest remainder method 24 25% Population Deviation Range 26 Ward Numbering format 27 Summary Information on Wards 28 E. Local Council Ward Delimitation Maps showing: 81 (i) Wards and Population i (ii) Wards, Chiefdoms and sections EASTERN REGION 1. Kailahun District Council 81 2. Kenema City Council 83 3. Kenema District Council 85 4. Koidu/New Sembehun City Council 87 5. Kono District Council 89 NORTHERN REGION 6. Makeni City Council 91 7. Bombali District Council 93 8. Kambia District Council 95 9. Koinadugu District Council 97 10. Port Loko District Council 99 11. Tonkolili District Council 101 SOUTHERN REGION 12. Bo City Council 103 13. Bo District Council 105 14. Bonthe Municipal Council 107 15. -

Esia Volume 1: Executive Summary & Main Report
ENVIRONMENTAL AND SOCIAL IMPACT ASSESSMENT STUDY FOR CT IN LUGBU CHIEFDOM BO DISTRICT ESIA VOLUME 1: EXECUTIVE SUMMARY & MAIN REPORT Prepared by CEMMATS Group Ltd on behalf of: SIERRA TROPICAL LIMITED (STL) June 2018 Freetown, Sierra Leone Environmental and Social Impact Assessment (ESIA) for the Sierra Tropical Ltd Agricultural Project Volume 1: Executive Summary and Main Report DOCUMENT HISTORY Version History Date Reviewer Environmental and Social Impact Assessment for the Sierra Tropical Ltd Title Agricultural Project Volume 1: Executive Summary and Main Report Anthony Mansaray; Arnold Okoni-Williams; Bartholomew Bockarie; Joe Authors Lappia; Leonard B. Buckle; Ralph Bona; Rashidu Sinnah; Vanessa James Date Written September 2016; updated June 2018 Subject Environmental and Social Impact Assessment Publisher CEMMATS Group Ltd Type Client Report Description ESIA for the Sierra Tropical Ltd Contributors Joseph Gbassa; Josephine Turay; Mariama Jalloh Format Source Text Rights © CEMMATS Group Ltd Identifier Language English Relation © CEMMATS Group Ltd, October 2016 ii Environmental and Social Impact Assessment (ESIA) for the Sierra Tropical Ltd Agricultural Project Volume 1: Executive Summary and Main Report CEMMATS Group Ltd (hereafter, 'CEMMATS') has prepared this Environmental and Social Impact Assessment (ESIA) Report for the sole use of the Client and for the intended purposes as stated in the Contract between the Client and CEMMATS under which this work was completed. This ESIA Report may not be relied upon by any other party without the express written agreement of CEMMATS and/or the Client. CEMMATS has exercised due and customary care in conducting this ESIA but has not, save as specifically stated, independently verified information provided by others. -

(Smes) As Agent of National Development in Sierra Leone
International Journal of Science and Research (IJSR) ISSN (Online): 2319-7064 Index Copernicus Value (2015): 78.96 | Impact Factor (2015): 6.391 Small and Medium Scale Enterprises (SMEs) as Agent of National Development in Sierra Leone Momodu Sahid Kanu, Bob Karankay Conteh School Of Agriculture, Njala University, Njala Campus, Private Mail Bag, Freetown, Sierra Leone, West Africa University of Makeni Abstract: This study, Small and Medium Enterprises (SMEs) as agent of national development was undertaken in Bo district. In all, 470 small and medium business enterprise owners were selected randomly and interviewed using questionnaires. Other methods of data collection were desk survey and observation; Data collected were analyzed using Statistical Package for Social Sciences (SPSS 16 and 23) applied on the data. A number of results, indices, frequency distributions, chi-square correlation, contingency tables, p-values, tests statistics etc., were generated with several interactions. The overall objective of this study is to identify the effect of SMEs as agents of national development and based on the findings make recommendations for the improvement of the performances of the business. The findings showed that most of the small and medium business owners were Sierra Leoneans (91.7%) and the rest were Guineans (8.2%) and Lebanese (8.2%).The majority of the respondents were in their productive age. Most of them were not educated; those educated had primary and/or secondary education. The respondents were fairly spread across a wide range of sectors, less than three-fourths of the sectors.(71.1%) in the economy, majority of them came from; Export 8(2.0%), services 187(38.9%), manufacturing 72(15.3%) and Trading 70(14.9%) and the others (28.4%). -

The Constitution of Sierra Leone Act, 1991
CONSTITUTIONAL INSTRUMENT SUPPLEMENT TO THE SIERRA LEONE GAZETTE EXTRAORIDARY VOL. CXXXVIII, NO. 16 dated 18th April, 2007 CONSTITUTIONAL INSTRUMENT NO. 5 OF 2007 Published 18th April, 2007 THE CONSTITUTION OF SIERRA LEONE, 1991 (Act No. 6 of 1991) PARLIAMENTARY ELECTIONS (DECLARATION OF CONSTITUENCIES) Short tittle ORDER, 2007 In exercise of the powers conferred upon him by Subsection (1) of section 38 of the Constitution of Sierra Leone 1991, the Electoral Commission hereby makes the following Order:- For the purpose of electing the ordinary Members of Parliament, Division of Sierra Leone Sierra Leone is hereby divided into one hundred and twelve into Constituencies. constituencies as described in the Schedule. 2 3 Name and Code Description SCHEDULE of Constituency EASTERN REGION KAILAHUN DISTRICT Kailahun This Constituency comprises of the whole of upper Bambara and District part of Luawa Chiefdom with the following sections; Gao, Giehun, Costituency DESCRIPTION OF CONSTITUENCIES 2 Lower Kpombali and Mende Buima. Name and Code Description of Constituency (NEC The constituency boundary starts in the northwest where the Chiefdom Const. 002) boundaries of Kpeje Bongre, Luawa and Upper Bambara meet. It follows the northern section boundary of Mende Buima and Giehun, then This constituency comprises of part of Luawa Chiefdom southwestern boundary of Upper Kpombali to meet the Guinea with the following sections: Baoma, Gbela, Luawa boundary. It follows the boundary southwestwards and south to where Foguiya, Mano-Sewallu, Mofindo, and Upper Kpombali. the Dea and Upper Bambara Chiefdom boundaries meet. It continues along the southern boundary of Upper Bambara west to the Chiefdom (NEC Const. The constituency boundary starts along the Guinea/ Sierra Leone boundaries of Kpeje Bongre and Mandu. -
Sierraleone Local Council Ward Boundary Delimitation Report
NATIONAL ELECTORAL COMMISSION Sierra Leone Local Council Ward Boundary Delimitation Report Volume Two Meets and Bounds April 2008 Table of Contents Preface ii A. Eastern region 1. Kailahun District Council 1 2. Kenema City Council 9 3. Kenema District Council 12 4. Koidu/New Sembehun City Council 22 5. Kono District Council 26 B. Northern Region 1. Makeni City Council 34 2. Bombali District Council 37 3. Kambia District Council 45 4. Koinadugu District Council 51 5. Port Loko District Council 57 6. Tonkolili District Council 66 C. Southern Region 1. Bo City Council 72 2. Bo District Council 75 3. Bonthe Municipal Council 80 4. Bonthe District Council 82 5. Moyamba District Council 86 6. Pujehun District Council 92 D. Western Region 1. Western Area Rural District Council 97 2. Freetown City Council 105 i Preface This part of the report on Electoral Ward Boundaries Delimitation process is a detailed description of each of the 394 Local Council Wards nationwide, comprising of Chiefdoms, Sections, Streets and other prominent features defining ward boundaries. It is the aspect that deals with the legal framework for the approved wards _____________________________ Dr. Christiana A. M Thorpe Chief Electoral Commissioner and Chair ii CONSTITUTIONAL INSTRUMENT No………………………..of 2008 Published: THE LOCAL GOVERNMENT ACT, 2004 (Act No. 1 of 2004) THE KAILAHUN DISTRICT COUNCIL (ESTABLISHMENT OF LOCALITY AND DELIMITATION OF WARDS) Order, 2008 Short title In exercise of the powers conferred upon him by subsection (2) of Section 2 of the Local Government Act, 2004, the President, acting on the recommendation of the Minister of Internal Affairs, Local Government and Rural Development, the Minister of Finance and Economic Development and the National Electoral Commission, hereby makes the following Order:‐ 1. -

Fragmentation and the Temne: from War Raids Into Ethnic Civil Wars
chapter 4 Fragmentation and the Temne: From War Raids into Ethnic Civil Wars The Temne and Their Neighbours: A Long-Standing Scenario of Inter-ethnic Hostilities? The former British colony of Sierra Leone is today regarded as one of the classic cases of a society that is politically polarised by ethnic antagonism. By the 1950s, the decade before independence, ethnic fault lines had an impact on local political life and the inhabitants of the colony appeared to practise ethnic voting. Both the Sierra Leone People’s Party (slpp) government formed after 1957, led by Milton Margai, and the All People’s Congress (apc) government of Siaka Stevens coming to power in 1967/68, relied on ethnic support and cre- ated ethnic networks: the slpp appeared to be ‘southern’ and ‘eastern’, and Mende-dominated, the apc ‘northern’ and Temne-led.1 Between 1961 and the 1990s, such voting behaviour can be found in sociological and political science survey data.2 However, the period of brutal civil war in the 1990s weakened some of these community links, as local communities were more interested in their survival than in ethnic solidarities.3 We have seen that the 2007 legislative elections contradicted this apparent trend. Before the second half of the nineteenth century, the territory of present-day Sierra Leone was politically fragmented into a number of different small structures, which were often much smaller than the pre-colonial states of Senegambia (Map 4). The only regional exception was the ‘federation’ of Morea, which, however, was an unstable entity. The slave trade and the ‘legitimate commerce’ in palm 1 Cartwright, John R., Politics in Sierra Leone 1947–67 (Toronto – Buffalo: University of Toronto Press, 1970), 101–2, 128; Fisher, ‘Elections’, 621–3; Riddell, J. -

The Chiefdoms of Sierra Leone
The Chiefdoms of Sierra Leone Tristan Reed1 James A. Robinson2 July 15, 2013 1Harvard University, Department of Economics, Littauer Center, 1805 Cambridge Street, Cambridge MA 02138; E-mail: [email protected]. 2Harvard University, Department of Government, IQSS, 1737 Cambridge Street., N309, Cambridge MA 02138; E-mail: [email protected]. Abstract1 In this manuscript, a companion to Acemoglu, Reed and Robinson (2013), we provide a detailed history of Paramount Chieftaincies of Sierra Leone. British colonialism transformed society in the country in 1896 by empowering a set of Paramount Chiefs as the sole authority of local government in the newly created Sierra Leone Protectorate. Only individuals from the designated \ruling families" of a chieftaincy are eligible to become Paramount Chiefs. In 2011, we conducted a survey in of \encyclopedias" (the name given in Sierra Leone to elders who preserve the oral history of the chieftaincy) and the elders in all of the ruling families of all 149 chieftaincies. Contemporary chiefs are current up to May 2011. We used the survey to re- construct the history of the chieftaincy, and each family for as far back as our informants could recall. We then used archives of the Sierra Leone National Archive at Fourah Bay College, as well as Provincial Secretary archives in Kenema, the National Archives in London and available secondary sources to cross-check the results of our survey whenever possible. We are the first to our knowledge to have constructed a comprehensive history of the chieftaincy in Sierra Leone. 1Oral history surveys were conducted by Mohammed C. Bah, Alimamy Bangura, Alieu K. -

Executive Summary & Main Report
ENVIRONMENTAL AND SOCIAL IMPACT ASSESSMENT STUDY FOR SIERRA TROPICAL LTD’s AGRICULTURAL PROJECT IN LUGBU CHIEFDOM BO DISTRICT EXECUTIVE SUMMARY & MAIN REPORT Prepared by CEMMATS Group Ltd on behalf of: SIERRA TROPICAL LIMITED (STL) September Freetown, Sierra Leone 2016 Environmental and Social Impact Assessment (ESIA) for the Sierra Tropical Ltd Agricultural Project: Executive Summary and Main Report DOCUMENT HISTORY Version History Date Reviewer Environmental and Social Impact Assessment for the Sierra Tropical Ltd Title Agricultural Project: Executive Summary and Main Report Anthony Mansaray; Arnold Okoni-Williams; Bartholomew Bockarie; Joe Authors Lappia; Leonard B. Buckle; Ralph Bona; Rashidu Sinnah; Vanessa James Date September 2016 Subject Environmental and Social Impact Assessment Publisher CEMMATS Group Ltd Type Client Report Description ESIA for the Sierra Tropical Ltd Contributors Joseph Gbassa; Josephine Turay; Mariama Jalloh Format Microsoft™ Word 2007 Source Text Rights © CEMMATS Group Ltd Identifier Language English Relation Coverage Sierra Leone, 2016 © CEMMATS Group Ltd, October 2016 ii Environmental and Social Impact Assessment (ESIA) for the Sierra Tropical Ltd Agricultural Project: Executive Summary and Main Report CONSULTANT’S DISCLAIMER CEMMATS Group Ltd (hereafter, 'CEMMATS') has prepared this Environmental and Social Impact Assessment (ESIA) Report for the sole use of the Client and for the intended purposes as stated in the Contract between the Client and CEMMATS under which this work was completed. This ESIA Report may not be relied upon by any other party without the express written agreement of CEMMATS and/or the Client. CEMMATS has exercised due and customary care in conducting this ESIA but has not, save as specifically stated, independently verified information provided by others. -
2006 Report on Electoral Constituency
August 2006 Preface This part of the report on Electoral Constituency Boundaries Delimitation process is a detailed description of each approved constituency. It comprises the chiefdoms, streets and other prominent features defining constituency boundaries. It is the aspect that deals with the legal framework for the approved constituencies. Ms. Christiana A. M. Thorpe (Dr.) Chief Electoral Commissioner and Chairperson. I Table of Contents Page A. Eastern Region…………………..……………………1 1. Kailahun District ……………………………………1 2. Kenema District………………………..……………5 3. Kono District……………………….………………14 B. Northern Region………………………..……………19 1. Bombali District………………….………..………19 2. Kambia District………………………..…..………25 3. Koinadugu District………………………….……31 4. Port Loko District……………………….…………34 5. Tonkolili District……………………………………43 C. Southern District……………………………………47 1. Bo District…………………………..………………47 2. Bonthe District………………………………………54 3. Moyamba District……………….…………………56 4. Pujehun District……………………………………60 D. Western Region………………………….……………64 1. Western Rural …………………….…………….....64 2. Western Urban ………………………………………81 II EASTERN REGION KAILAHUN DISTRICT (01) DESCRIPTION OF CONSTITUENCIES Name & Code Description of Constituency Kailahun District This constituency comprises of part of Luawa chiefdom with the Constituency 1 following sections: Baoma, Gbela, Luawa Foguiya, ManoSewallu, Mofindo, and Upper Kpombali. (NEC Const. 001) The constituency boundary starts along the Guinea/Sierra Leone international boundary northeast where the chiefdom boundaries of Kissi Kama and Luawa meet. It follows the Kissi Kama Luawa chiefdom boundary north and generally southeast to the meeting point of Kissi Kama, Luawa and Kissi Tongi chiefdoms. It continues along the Luawa/Kissi Tongi boundary south, east then south to meet the Guinea boundary on the southeastern boundary of Upper Kpombali section in Luawa chiefdom. It continues west wards along the international boundary to the southern boundary of Upper Kpombali section. -

Environmental and Social Impact Assessment (ESIA) for the Sierra Tropical Ltd Agricultural Project: Executive Summary and Main Report
ENVIRONMENTAL AND SOCIAL IMPACT ASSESSMENT STUDY FOR SIERRA TROPICAL LTD’s AGRICULTURAL PROJECT IN LUGBU CHIEFDOM BO DISTRICT EXECUTIVE SUMMARY & MAIN REPORT Prepared by CEMMATS Group Ltd on behalf of: SIERRA TROPICAL LIMITED (STL) September Freetown, Sierra Leone 2016 Environmental and Social Impact Assessment (ESIA) for the Sierra Tropical Ltd Agricultural Project: Executive Summary and Main Report DOCUMENT HISTORY Version History Date Reviewer Environmental and Social Impact Assessment for the Sierra Tropical Ltd Title Agricultural Project: Executive Summary and Main Report Anthony Mansaray; Arnold Okoni-Williams; Bartholomew Bockarie; Joe Authors Lappia; Leonard B. Buckle; Ralph Bona; Rashidu Sinnah; Vanessa James Date September 2016 Subject Environmental and Social Impact Assessment Publisher CEMMATS Group Ltd Type Client Report Description ESIA for the Sierra Tropical Ltd Contributors Joseph Gbassa; Josephine Turay; Mariama Jalloh Format Microsoft™ Word 2007 Source Text Rights © CEMMATS Group Ltd Identifier Language English Relation Coverage Sierra Leone, 2016 © CEMMATS Group Ltd, October 2016 ii Environmental and Social Impact Assessment (ESIA) for the Sierra Tropical Ltd Agricultural Project: Executive Summary and Main Report CONSULTANT’S DISCLAIMER CEMMATS Group Ltd (hereafter, 'CEMMATS') has prepared this Environmental and Social Impact Assessment (ESIA) Report for the sole use of the Client and for the intended purposes as stated in the Contract between the Client and CEMMATS under which this work was completed. This ESIA Report may not be relied upon by any other party without the express written agreement of CEMMATS and/or the Client. CEMMATS has exercised due and customary care in conducting this ESIA but has not, save as specifically stated, independently verified information provided by others. -
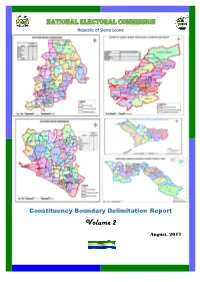
2017 Constituency Boundary Delimitation Report, Vol. 2
NATIONAL ELECTORAL COMMISSION Republic of Sierra Leone Constituency Boundary Delimitation Report Volume 2 August, 2017 Foreword The National Electoral Commission (NEC) is submitting this report on the delimitation of constituency and ward boundaries in adherence to its constitutional mandate to delimit electoral constituency and ward boundaries, to be done “not less than five years and not more than seven years”; and complying with the timeline as stipulated in the NEC Electoral Calendar (2015-2019). The report is subject to Parliamentary approval, as enshrined in the 1991 Constitution of Sierra Leone (Act No 6 of 1991); which inter alia states delimitation of electoral boundaries to be done by NEC, while Section 38 (1) empowers the Commission to divide the country into constituencies for the purpose of electing Members of Parliament (MPs) using Single Member First- Past –the Post (FPTP) system. The Local Government Act of 2004, Part 1 –preliminary, assigns the task of drawing wards to NEC; while the Public Elections Act, 2012 (Section 14, sub-sections 1 &2) forms the legal basis for the allocation of council seats and delimitation of wards in Sierra Leone. The Commission appreciates the level of technical assistance, collaboration and cooperation it received from Statistics Sierra Leone (SSL), the Boundary Delimitation Technical Committee (BDTC), the Boundary Delimitation Monitoring Committee (BDMC), donor partners, line Ministries, Departments and Agencies and other key actors in the boundary delimitation exercise. The hiring of a Consultant, Dr Lisa Handley, an internationally renowned Boundary delimitation expert, added credence and credibility to the process as she provided professional advice which assisted in maintaining international standards and best practices. -

Downloaded Cc-By-Nc from License.Brill.Com09/29/2021 02:25:30AM Via Free Access
chapter 4 Fragmentation and the Temne: From War Raids into Ethnic Civil Wars The Temne and Their Neighbours: A Long-Standing Scenario of Inter-ethnic Hostilities? The former British colony of Sierra Leone is today regarded as one of the classic cases of a society that is politically polarised by ethnic antagonism. By the 1950s, the decade before independence, ethnic fault lines had an impact on local political life and the inhabitants of the colony appeared to practise ethnic voting. Both the Sierra Leone People’s Party (slpp) government formed after 1957, led by Milton Margai, and the All People’s Congress (apc) government of Siaka Stevens coming to power in 1967/68, relied on ethnic support and cre- ated ethnic networks: the slpp appeared to be ‘southern’ and ‘eastern’, and Mende-dominated, the apc ‘northern’ and Temne-led.1 Between 1961 and the 1990s, such voting behaviour can be found in sociological and political science survey data.2 However, the period of brutal civil war in the 1990s weakened some of these community links, as local communities were more interested in their survival than in ethnic solidarities.3 We have seen that the 2007 legislative elections contradicted this apparent trend. Before the second half of the nineteenth century, the territory of present-day Sierra Leone was politically fragmented into a number of different small structures, which were often much smaller than the pre-colonial states of Senegambia (Map 4). The only regional exception was the ‘federation’ of Morea, which, however, was an unstable entity. The slave trade and the ‘legitimate commerce’ in palm 1 Cartwright, John R., Politics in Sierra Leone 1947–67 (Toronto – Buffalo: University of Toronto Press, 1970), 101–2, 128; Fisher, ‘Elections’, 621–3; Riddell, J.