When Randomization Is Not Possible
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Survey Experiments
IU Workshop in Methods – 2019 Survey Experiments Testing Causality in Diverse Samples Trenton D. Mize Department of Sociology & Advanced Methodologies (AMAP) Purdue University Survey Experiments Page 1 Survey Experiments Page 2 Contents INTRODUCTION ............................................................................................................................................................................ 8 Overview .............................................................................................................................................................................. 8 What is a survey experiment? .................................................................................................................................... 9 What is an experiment?.............................................................................................................................................. 10 Independent and dependent variables ................................................................................................................. 11 Experimental Conditions ............................................................................................................................................. 12 WHY CONDUCT A SURVEY EXPERIMENT? ........................................................................................................................... 13 Internal, external, and construct validity .......................................................................................................... -
Analysis of Variance and Analysis of Variance and Design of Experiments of Experiments-I
Analysis of Variance and Design of Experimentseriments--II MODULE ––IVIV LECTURE - 19 EXPERIMENTAL DESIGNS AND THEIR ANALYSIS Dr. Shalabh Department of Mathematics and Statistics Indian Institute of Technology Kanpur 2 Design of experiment means how to design an experiment in the sense that how the observations or measurements should be obtained to answer a qqyuery inavalid, efficient and economical way. The desigggning of experiment and the analysis of obtained data are inseparable. If the experiment is designed properly keeping in mind the question, then the data generated is valid and proper analysis of data provides the valid statistical inferences. If the experiment is not well designed, the validity of the statistical inferences is questionable and may be invalid. It is important to understand first the basic terminologies used in the experimental design. Experimental unit For conducting an experiment, the experimental material is divided into smaller parts and each part is referred to as experimental unit. The experimental unit is randomly assigned to a treatment. The phrase “randomly assigned” is very important in this definition. Experiment A way of getting an answer to a question which the experimenter wants to know. Treatment Different objects or procedures which are to be compared in an experiment are called treatments. Sampling unit The object that is measured in an experiment is called the sampling unit. This may be different from the experimental unit. 3 Factor A factor is a variable defining a categorization. A factor can be fixed or random in nature. • A factor is termed as fixed factor if all the levels of interest are included in the experiment. -

The Politics of Random Assignment: Implementing Studies and Impacting Policy
The Politics of Random Assignment: Implementing Studies and Impacting Policy Judith M. Gueron Manpower Demonstration Research Corporation (MDRC) As the only nonacademic presenting a paper at this conference, I see it as my charge to focus on the challenge of implementing random assignment in the field. I will not spend time arguing for the methodological strengths of social experiments or advocating for more such field trials. Others have done so eloquently.1 But I will make my biases clear. For 25 years, I and many of my MDRC colleagues have fought to implement random assignment in diverse arenas and to show that this approach is feasible, ethical, uniquely convincing, and superior for answering certain questions. Our organization is widely credited with being one of the pioneers of this approach, and through its use producing results that are trusted across the political spectrum and that have made a powerful difference in social policy and research practice. So, I am a believer, but not, I hope, a blind one. I do not think that random assignment is a panacea or that it can address all the critical policy questions, or substitute for other types of analysis, or is always appropriate. But I do believe that it offers unique power in answering the “Does it make a difference?” question. With random assignment, you can know something with much greater certainty and, as a result, can more confidently separate fact from advocacy. This paper focuses on implementing experiments. In laying out the ingredients of success, I argue that creative and flexible research design skills are essential, but that just as important are operational and political skills, applied both to marketing the experiment in the first place and to helping interpret and promote its findings down the line. -

Key Items to Get Right When Conducting Randomized Controlled Trials of Social Programs
Key Items to Get Right When Conducting Randomized Controlled Trials of Social Programs February 2016 This publication was produced by the Evidence-Based Policy team of the Laura and John Arnold Foundation (now Arnold Ventures). This publication is in the public domain. Authorization to reproduce it in whole or in part for educational purposes is granted. We welcome comments and suggestions on this document ([email protected]). 1 Purpose This is a checklist of key items to get right when conducting a randomized controlled trial (RCT) to evaluate a social program or practice. The checklist is designed to be a practical resource for researchers and sponsors of research. It describes items that are critical to the success of an RCT in producing valid findings about a social program’s effectiveness. This document is limited to key items, and does not address all contingencies that may affect a study’s success.1 Items in this checklist are categorized according to the following phases of an RCT: 1. Planning the study; 2. Carrying out random assignment; 3. Measuring outcomes for the study sample; and 4. Analyzing the study results. 1. Key items to get right in planning the study Choose (i) the program to be evaluated, (ii) target population for the study, and (iii) key outcomes to be measured. These should include, wherever possible, ultimate outcomes of policy importance. As illustrative examples: . An RCT of a pregnancy prevention program preferably should measure outcomes such as pregnancies or births, and not just intermediate outcomes such as condom use. An RCT of a remedial reading program preferably should measure outcomes such as reading comprehension, and not just participants’ ability to sound out words. -
How to Randomize?
TRANSLATING RESEARCH INTO ACTION How to Randomize? Roland Rathelot J-PAL Course Overview 1. What is Evaluation? 2. Outcomes, Impact, and Indicators 3. Why Randomize and Common Critiques 4. How to Randomize 5. Sampling and Sample Size 6. Threats and Analysis 7. Project from Start to Finish 8. Cost-Effectiveness Analysis and Scaling Up Lecture Overview • Unit and method of randomization • Real-world constraints • Revisiting unit and method • Variations on simple treatment-control Lecture Overview • Unit and method of randomization • Real-world constraints • Revisiting unit and method • Variations on simple treatment-control Unit of Randomization: Options 1. Randomizing at the individual level 2. Randomizing at the group level “Cluster Randomized Trial” • Which level to randomize? Unit of Randomization: Considerations • What unit does the program target for treatment? • What is the unit of analysis? Unit of Randomization: Individual? Unit of Randomization: Individual? Unit of Randomization: Clusters? Unit of Randomization: Class? Unit of Randomization: Class? Unit of Randomization: School? Unit of Randomization: School? How to Choose the Level • Nature of the Treatment – How is the intervention administered? – What is the catchment area of each “unit of intervention” – How wide is the potential impact? • Aggregation level of available data • Power requirements • Generally, best to randomize at the level at which the treatment is administered. Suppose an intervention targets health outcomes of children through info on hand-washing. What is the appropriate level of randomization? A. Child level 30% B. Household level 23% C. Classroom level D. School level 17% E. Village level 13% 10% F. Don’t know 7% A. B. C. D. -

Chapter 5 Experiments, Good And
Chapter 5 Experiments, Good and Bad Point of both observational studies and designed experiments is to identify variable or set of variables, called explanatory variables, which are thought to predict outcome or response variable. Confounding between explanatory variables occurs when two or more explanatory variables are not separated and so it is not clear how much each explanatory variable contributes in prediction of response variable. Lurking variable is explanatory variable not considered in study but confounded with one or more explanatory variables in study. Confounding with lurking variables effectively reduced in randomized comparative experiments where subjects are assigned to treatments at random. Confounding with a (only one at a time) lurking variable reduced in observational studies by controlling for it by comparing matched groups. Consequently, experiments much more effec- tive than observed studies at detecting which explanatory variables cause differences in response. In both cases, statistically significant observed differences in average responses implies differences are \real", did not occur by chance alone. Exercise 5.1 (Experiments, Good and Bad) 1. Randomized comparative experiment: effect of temperature on mice rate of oxy- gen consumption. For example, mice rate of oxygen consumption 10.3 mL/sec when subjected to 10o F. temperature (Fo) 0 10 20 30 ROC (mL/sec) 9.7 10.3 11.2 14.0 (a) Explanatory variable considered in study is (choose one) i. temperature ii. rate of oxygen consumption iii. mice iv. mouse weight 25 26 Chapter 5. Experiments, Good and Bad (ATTENDANCE 3) (b) Response is (choose one) i. temperature ii. rate of oxygen consumption iii. -

Randomized Experimentsexperiments Randomized Trials
Impact Evaluation RandomizedRandomized ExperimentsExperiments Randomized Trials How do researchers learn about counterfactual states of the world in practice? In many fields, and especially in medical research, evidence about counterfactuals is generated by randomized trials. In principle, randomized trials ensure that outcomes in the control group really do capture the counterfactual for a treatment group. 2 Randomization To answer causal questions, statisticians recommend a formal two-stage statistical model. In the first stage, a random sample of participants is selected from a defined population. In the second stage, this sample of participants is randomly assigned to treatment and comparison (control) conditions. 3 Population Randomization Sample Randomization Treatment Group Control Group 4 External & Internal Validity The purpose of the first-stage is to ensure that the results in the sample will represent the results in the population within a defined level of sampling error (external validity). The purpose of the second-stage is to ensure that the observed effect on the dependent variable is due to some aspect of the treatment rather than other confounding factors (internal validity). 5 Population Non-target group Target group Randomization Treatment group Comparison group 6 Two-Stage Randomized Trials In large samples, two-stage randomized trials ensure that: [Y1 | D =1]= [Y1 | D = 0] and [Y0 | D =1]= [Y0 | D = 0] • Thus, the estimator ˆ ˆ ˆ δ = [Y1 | D =1]-[Y0 | D = 0] • Consistently estimates ATE 7 One-Stage Randomized Trials Instead, if randomization takes place on a selected subpopulation –e.g., list of volunteers-, it only ensures: [Y0 | D =1] = [Y0 | D = 0] • And hence, the estimator ˆ ˆ ˆ δ = [Y1 | D =1]-[Y0 | D = 0] • Only estimates TOT Consistently 8 Randomized Trials Furthermore, even in idealized randomized designs, 1. -

How to Do Random Allocation (Randomization) Jeehyoung Kim, MD, Wonshik Shin, MD
Special Report Clinics in Orthopedic Surgery 2014;6:103-109 • http://dx.doi.org/10.4055/cios.2014.6.1.103 How to Do Random Allocation (Randomization) Jeehyoung Kim, MD, Wonshik Shin, MD Department of Orthopedic Surgery, Seoul Sacred Heart General Hospital, Seoul, Korea Purpose: To explain the concept and procedure of random allocation as used in a randomized controlled study. Methods: We explain the general concept of random allocation and demonstrate how to perform the procedure easily and how to report it in a paper. Keywords: Random allocation, Simple randomization, Block randomization, Stratified randomization Randomized controlled trials (RCT) are known as the best On the other hand, many researchers are still un- method to prove causality in spite of various limitations. familiar with how to do randomization, and it has been Random allocation is a technique that chooses individuals shown that there are problems in many studies with the for treatment groups and control groups entirely by chance accurate performance of the randomization and that some with no regard to the will of researchers or patients’ con- studies are reporting incorrect results. So, we will intro- dition and preference. This allows researchers to control duce the recommended way of using statistical methods all known and unknown factors that may affect results in for a randomized controlled study and show how to report treatment groups and control groups. the results properly. Allocation concealment is a technique used to pre- vent selection bias by concealing the allocation sequence CATEGORIES OF RANDOMIZATION from those assigning participants to intervention groups, until the moment of assignment. -

Random Assignment
7 RANDOM ASSIGNMENT Just as representativeness can be secured by the method of chance . so equivalence may be secured by chance.1distribute —W. A. McCall or LEARNING OBJECTIVES • Understand what random assignment does and how it works. • Produce a valid randomization processpost, for an experiment and describe it. • Critique simple random assignment, blocking, matched pairs, and stratified random assignment. • Explain the importance of counterbalancing. • Describe a Latincopy, square design. ust as the mantra in real estate is “location, location, location,” the motto in experi- Jmental design is “random assignment, random assignment, random assignment.” This notbook has discussed random assignment all throughout. It bears repeating that ran- dom assignment is the single most important thing a researcher can do in an experiment. Everything else pales in comparison to having done this correctly.2 Random assignment is what distinguishes a true experiment from a quasi, natural, or pre-experimental design. In Dochapter 1, experiments were referred to as the gold standard. Without successful random 173 Copyright ©2019 by SAGE Publications, Inc. This work may not be reproduced or distributed in any form or by any means without express written permission of the publisher. 174 Designing Experiments for the Social Sciences assignment, however, they can quickly become “the bronze standard.”3 This chapter will review some of the advantages of random assignment, discuss the details of how to do it, and explore related issues of counterbalancing. THE PURPOSE OF RANDOM ASSIGNMENT People vary. That is, they are different. Were this not so, there would be no reason to study them. Everyone would be the same, reacting the same way to different teaching techniques, advertisements, health interventions, and political messages. -

Bias in Rcts: Confounders, Selection Bias and Allocation Concealment
Vol. 10, No. 3, 2005 Middle East Fertility Society Journal © Copyright Middle East Fertility Society EVIDENCE-BASED MEDICINE CORNER Bias in RCTs: confounders, selection bias and allocation concealment Abdelhamid Attia, M.D. Professor of Obstetrics & Gynecology and secretary general of the center of evidence-Based Medicine, Cairo University, Egypt The double blind randomized controlled trial that may distort a RCT results and how to avoid (RCT) is considered the gold-standard in clinical them is mandatory for researchers who seek research. Evidence for the effectiveness of conducting proper research of high relevance and therapeutic interventions should rely on well validity. conducted RCTs. The importance of RCTs for clinical practice can be illustrated by its impact on What is bias? the shift of practice in hormone replacement therapy (HRT). For decades HRT was considered Bias is the lack of neutrality or prejudice. It can the standard care for all postmenopausal, be simply defined as "the deviation from the truth". symptomatic and asymptomatic women. Evidence In scientific terms it is "any factor or process that for the effectiveness of HRT relied always on tends to deviate the results or conclusions of a trial observational studies mostly cohort studies. But a systematically away from the truth2". Such single RCT that was published in 2002 (The women's deviation leads, usually, to over-estimating the health initiative trial (1) has changed clinical practice effects of interventions making them look better all over the world from the liberal use of HRT to the than they actually are. conservative use in selected symptomatic cases and Bias can occur and affect any part of a study for the shortest period of time. -
Introduction to Impact Evaluation in Social Epidemiology and Public Health
Introduction to Impact Evaluation in Social Epidemiology and Public Health Sam Harper Arijit Nandi McGill University Epi Tools Workshop Series, UCSF, 13 April 2017 1 / 194 Outline 1 What is Impact Evaluation? 2 Evaluating: Randomized studies Pre-randomization phase Randomization phase 3 Evaluating: Non-randomized studies Problems with non-randomized studies Instrumental Variables Regression discontinuity ITS and Difference-in-Differences 4 Concluding thoughts 5 References 2 / 194 This is an “Epi Tools” workshop What’s in your toolbox? 4 / 194 Causation, Association, and Confounding Causal effect: Do individuals randomly assigned (i.e., SET) to treatment have better outcomes? E (Y jSET [Treated]) − E (Y jSET [Untreated]) Association: Do individuals who happen to be treated have better outcomes? E (Y jTreated) − E(Y jUntreated) Confounding [Omitted Variable Bias] : E (Y jSET [Treated]) − E (Y jSET [Untreated]) 6= E (Y jTreated) − E (Y jUntreated) 5 / 194 Effect of what? Questions about effects are expressed as counterfactual contrasts. We can write the average causal effect (ACE) or average treatment effect (ATE) in terms of potential outcomes: E Y a=1 − E Y a=0 indicating potential outcomes for an individual under two possible treatments. Consistency assumption: Y a = a for every individual with A = a. Problematic when there are multiple versions of the treatment, or when we do not have control over treatment assignment. We need well-defined treatments. Hernan 2016[1], among others. 6 / 194 Here’s a question: Does obesity shorten life? The increased emphasis on causal inference in epidemiology has generated some acrimonious debate:* Vandenbroucke, Pearce, Broadbent, Krieger, Davey Smith, Ebrahim, Schwartz, etc.. -
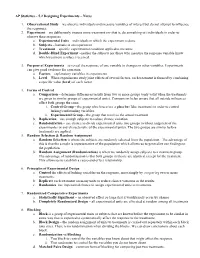
AP Statistics – 5.2 Designing Experiments – Notes
AP Statistics – 5.2 Designing Experiments – Notes 1. Observational Study – we observe individuals and measure variables of interest but do not attempt to influence the responses. 2. Experiment – we deliberately impose some treatment on (that is, do something to) individuals in order to observe their responses. a. Experimental Units – individuals in which the experiment is done b. Subjects – humans in an experiment c. Treatment – specific experimental condition applied to the units d. Double-Blind Experiment –neither the subjects nor those who measure the response variable know which treatment a subject received. 3. Purpose of Experiments – to reveal the response of one variable to changes in other variables. Experiments can give good evidence for causation. a. Factors – explanatory variables in experiments b. Level – When experiments study joint effects of several factors, each treatment is formed by combining a specific value (level) of each factor. 4. Forms of Control a. Comparison – determine differences/results from two or more groups (only valid when the treatments are given to similar groups of experimental units). Comparison helps ensure that all outside influences affect both groups the same. i. Control Group – the group which receives a placebo (fake treatment) in order to control lurking/confounding variables. ii. Experimental Group – the group that receives the actual treatment b. Replication – use enough subjects to reduce chance variation. c. Randomization – use chance to divide experimental units into groups (without judgment of the experimenter or any characteristic of the experimental units). The two groups are similar before treatments are applied. 5. Random Selection & Random Assignment a. Random Selection is where the subjects are randomly selected from the population.