Suicide Survivors Resource Pack
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Living the GOOD and BEAUTIFUL Life 1 INSTRUCTIONS
APPRENTICE SERIES CURRICULUM TheLiving Good and Beautiful LElifeADER GUIDE by Matthew Johnson TABLE OF CONTENTS Instructions ........................................................................................................................................................2 Study Schedule .................................................................................................................................................2 12 The Good and Beautiful Life ........................................................................................................3 13 The Gospel Many People Have Never Heard ........................................................................6 14 The Grand Invitation ........................................................................................................................8 15 Learning to Live Without Anger ..............................................................................................11 “Exploring Anger” Handout .....................................................................................................................14 16 Learning to Live Without Lust ................................................................................................ 15 Silent Retreat .......................................................................................................................................21 “Scripture for Silent Reflection” Handout .............................................................................................25 17 Learning to Live -

Download This Newsletter
NEWS VOL. 35 • NUMBER 1 • DECEMBER 2017 The Unfolding of Centering Prayer he essence and heart of Centering Prayer is consenting to God’s presence T and action within. It leads to contemplation and its continuing development. The following qualities reveal how this consent deepens through daily practice. 1. Silence arises in consenting to God’s presence within. External silence supports this movement and leads to interior silence. 2. Solitude flows from interior silence. It disregards the endless conversation Thomas Keating we have with ourselves and rests in the experience of God’s presence. 3. Solidarity is the growing awareness of our oneness with the whole human family and with all creation. It is sensitive to the ever-present inspirations of the Spirit, not only during the time of formal prayer, but in the details of everyday life. 4. Service is an expression of solidarity that is an inner call to serve God and others based on the realization that God is loving and serving them through us. In other words, God in us is serving God in others. 5. Stillness is what Jesus called “prayer in secret” (Matt. 6:6). This is the experience of God’s presence beyond rational concepts and preoccupation with our thoughts and desires. Interior silence tends to move into solitude and then into stillness. Stillness is the habitat of contemplative prayer. As Saint John of the Cross teaches, contemplation is the inflowing of God into our souls, and in the Christian tradition, is looked upon as pure gift. In actual fact, it is a gift that has already been given. -

Welcome, We Have Been Archiving This Data for Research and Preservation of These Early Discs. ALL MP3 Files Can Be Sent to You B
Welcome, To our MP3 archive section. These listings are recordings taken from early 78 & 45 rpm records. We have been archiving this data for research and preservation of these early discs. ALL MP3 files can be sent to you by email - $2.00 per song Scroll until you locate what you would like to have sent to you, via email. If you don't use Paypal you can send payment to us at: RECORDSMITH, 2803 IRISDALE AVE RICHMOND, VA 23228 Order by ARTIST & TITLE [email protected] S.O.S. Band - Finest, The 1983 S.O.S. Band - Just Be Good To Me 1984 S.O.S. Band - Just The Way You Like It 1980 S.O.S. Band - Take Your Time (Do It Right) 1983 S.O.S. Band - Tell Me If You Still Care 1999 S.O.S. Band with UWF All-Stars - Girls Night Out S.O.U.L. - On Top Of The World 1992 S.O.U.L. S.Y.S.T.E.M. with M. Visage - It's Gonna Be A Love. 1995 Saadiq, Raphael - Ask Of You 1999 Saadiq, Raphael with Q-Tip - Get Involved 1981 Sad Cafe - La-Di-Da 1979 Sad Cafe - Run Home Girl 1996 Sadat X - Hang 'Em High 1937 Saddle Tramps - Hot As I Am 1937 (Voc 3708) Saddler, Janice & Jammers - My Baby's Coming Home To Stay 1993 Sade - Kiss Of Life 1986 Sade - Never As Good As The First Time 1992 Sade - No Ordinary Love 1988 Sade - Paradise 1985 Sade - Smooth Operator 1985 Sade - Sweetest Taboo, The 1985 Sade - Your Love Is King Sadina - It Comes And Goes 1966 Sadler, Barry - A Team 1966 Sadler, Barry - Ballad Of The Green Berets 1960 Safaris - Girl With The Story In Her Eyes 1960 Safaris - Image Of A Girl 1963 Safaris - Kick Out 1988 Sa-Fire - Boy, I've Been Told 1989 Sa-Fire - Gonna Make it 1989 Sa-Fire - I Will Survive 1991 Sa-Fire - Made Up My Mind 1989 Sa-Fire - Thinking Of You 1983 Saga - Flyer, The 1982 Saga - On The Loose 1983 Saga - Wind Him Up 1994 Sagat - (Funk Dat) 1977 Sager, Carol Bayer - I'd Rather Leave While I'm In Love 1977 1981 Sager, Carol Bayer - Stronger Than Before 1977 Sager, Carol Bayer - You're Moving Out Today 1969 Sagittarius - In My Room 1967 Sagittarius - My World Fell Down 1969 Sagittarius (feat. -
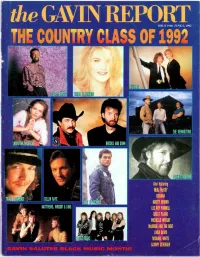
The GAVIN REPORT the COUNTRY CLASS of 1992
the GAVIN REPORT THE COUNTRY CLASS OF 1992 _; Also featuring NEAL McCOY DIXIANA COLLIN RAYE MARTY BROWN LEE ROY PARNELL GREAT PLAINS MICHELLE WRIGHT McBRIDE AND THE RIDE LINDA DAVIS MICHAEL WHITE SAMMY KERSHAW GAVIN e A K.lLITES BLACK MUSIC MdfleekrTlW In the dictionary, next to the wo -d "summer,' is a picture of the Love Shack. The video for "Roam" changed the way you eat bagels and bananas forever. Cosmic Thing comes to nearly four million pieces of history. T{ -at about cover; the last lime tl-e B -52's made a reco-d.Thisigk, the first ry direction. s Produced by Don Was Direct Manage -rent Group -Stemmei Jensen & Martin Krkup 9 ®' 992 Reprise Recoris. ft s a sock hop it +our own private Idc óo the GAVIN REPORT GAVIN AT A * Indicates Tie it» 4rv URBAN MOST ADDED MOST ADDED THE CURE EN VOGUE YO YO Friday I'm In Love (Fiction/Elektra) Giving Him Something He Can Feel (Atco/EastWest Home Girl Don't Play Dat (Atco/EastWest America) DEF LEPPARD America) ERIC B & RAKIM Make Love Like A Man (Mercury) TLC Don't Sweat The Technique (MCA) TOAD THE WET SPROCKET Baby -Baby -Baby (LaFace/Arista) X -CLAN Xodus (Polydor/PLG) All I Want (Columbia) ALYSON WILLIAMS Just My Luck (RAL/OBR/Columbia) HEAVY D. & THE BOYZ RECORD TO WATCH RECORD TO WATCH RETAIL MERYN CADELL DAVID BLACK You Can't See What I Can See The Swea er (Sire/Reprise) Nobody But You (Bust It/Capitol) (MCA) itAe RADIO SHANTE RICHARD MARX MARIAN CAREY Big Mama (Livin' Large/ Take This Heart (Capitol) I'll Be There (Columbia) Tommy Boy) COUNTRY MOST ADDED MOST ADDED MOST ADDED RICHARD -
Viii. Daily Proceedings
NORTH TEXAS CONFERENCE JOURNAL—2009 139 VIII. DAILY PROCEEDINGS SUNDAY AFTERNOON AND EVENING June 7, 2009 Laity Session and Dinner St. Andrew United Methodist Church, Plano, Texas, 3:30 p.m. The laity session of The North Texas Conference was held at St. Andrew United Methodist Church of Plano. Conference Lay Leader, Richard Hearne, welcomed the lay members of annual conference and Doug Meyer opened the session in prayer. Bishop W. Earl Bledsoe spoke to the laity session via DVD, saying that the laity will be a key part in the strategic planning. Bishop Bledsoe’s wife Leslie was recognized as a special guest. Hearne noted the provision for annual conference sessions divided half and half laity and clergy. He asked all first-time lay members to stand. They represented approximately one-third of the gathering. Ben Bennett, lay leader for Paris/Sulphur Springs District, led the memorial service for lay members of conference who have died within the past year. Linda Parks, conference lay-leader elect, reported on the Bishop’s Strategic Plan Team, legislative item #22, reminding laity that the Strategic Planning Team consists of twenty clergy and nine laity. She reminded everyone that Hopes and Dreams cards are available and may be turned in at the opening worship or any time until July 31 at www.holyconferencing.com website. Richard Stanford briefed lay members on constitutional amendments being offered for vote. The closing prayer also served as a blessing, and the members had dinner at St. Andrew United Methodist Church. Clergy Session First United Methodist Church, Plano, Texas, 3:30 p.m. -
Listening: a Sacred Path February 17-April 4, 2021
Listening: A Sacred Path February 17-April 4, 2021 Westminster Presbyterian Church 1200 Marquette Ave S | Minneapolis, MN westminstermpls.org 1 Cover: Incarnation, by Dao Zi, Chinese ink wash and gold powder, Bejing, China 2019 2 This page: and the Word became flesh...and we have seen his glory..., by Kirsten Malcolm Berry, watercolor on paper, 2018 Dear friends, Since September 2020, at Westminster we have committed ourselves to A Year of Listening in our life as a congregation. In light of all that has been revealed over the last 12 months about our nation – health disparities laid bare by Covid, deeply imbedded racism shown once again in the death of unarmed Black persons at the hands of police, widespread accep- tance of falsehood in our politics – we acknowledge our need to be attentive in new ways to voices we may not have previously heard. This collection of reflections on Westminster’s 2021 Lenten theme, The Listening Season, offers rich insight into the practice of listening in the spiritual lives of our church members. We thank the writers; I encourage you to listen carefully to their voices. These essays are written and included here with minimal editing. In its public language, Westminster customarily uses non-gendered language in reference to God. Here the authors speak from personal experience, using their own words. Recognizing these intimate expressions reflect particular perspectives, we have not edited the use of pronouns for God. As my own hearing disability has worsened in recent years I have grown increasingly aware of how hard we have to work at listening. -
Shanice Inner Child Mp3, Flac, Wma
Shanice Inner Child mp3, flac, wma DOWNLOAD LINKS (Clickable) Genre: Hip hop / Funk / Soul Album: Inner Child Country: UK Released: 1991 Style: RnB/Swing, Soul MP3 version RAR size: 1197 mb FLAC version RAR size: 1562 mb WMA version RAR size: 1874 mb Rating: 4.7 Votes: 747 Other Formats: MP4 DXD AUD MP1 VQF VOC FLAC Tracklist Hide Credits 1 Keep Your Inner Child Alive (Interlude) 2 I Love Your Smile 3 Forever In Your Love 4 I'm Cryin' 5 I Hate To Be Lonely 6 Stop Cheatin' On Me 7 Silent Prayer 8 Peace In The World 9 Lovin' You 10 You Ain't All That 11 Shanice & Mookie Meet Homey (Interlude) 12 You Didn't Think I'd Come Back This Hard 13 You Were The One I Love Your Smile (Driza Bone Remix) 14 Remix – Drizabone 15 Goodnight (Interlude) Credits Mastered By – Bob Ludwig Mixed By – David Frazer Producer – Narada Michael Walden Notes 1st press Barcode and Other Identifiers Barcode (Scanned): 4988017031582 Rights Society: JASRAC Other versions Category Artist Title (Format) Label Category Country Year 530 007-1 Shanice Inner Child (LP, Album) Motown 530 007-1 US 1991 MOTC 6319 Shanice Inner Child (Cass, Album, Club) Motown MOTC 6319 US 1991 374 636 319-4 Shanice Inner Child (Cass, Album) Motown 374 636 319-4 Canada 1991 3746363194 Shanice Inner Child (Cass, Album) Motown 3746363194 US 1991 530 008-4 Shanice Inner Child (Cass, Album) Motown 530 008-4 US 1991 Related Music albums to Inner Child by Shanice Funk / Soul / Pop Shanice Featuring Johnny Gill - Silent Prayer Rock / Pop Desmond Child - Legends, the Music of Hip hop / Pop Shanice - Saving Forever For You Funk / Soul / Pop Shanice - Lovin' You Reggae J.C. -

You Are Enough: You Do
Digital Galley Edition This is uncorrected advance content collected for your reviewing convenience. Please check with publisher or refer to the finished product whenever you are excerpting or quoting in a review. Copyright © 2018 by Amanda Hale Cover design by TK. Cover copyright © 2018 by Hachette Book Group, Inc. Hachette Book Group supports the right to free expression and the value of copyright. The purpose of copyright is to encourage writers and artists to produce the creative works that enrich our culture. The scanning, uploading, and distribution of this book without permission is a theft of the author’s intellectual property. If you would like permission to use material from the book (other than for review purposes), please contact [email protected]. Thank you for your support of the author’s rights. FaithWords Hachette Book Group 1290 Avenue of the Americas, New York, NY 10104 faithwords.com twitter.com/faithwords First Edition: November 2018 FaithWords is a division of Hachette Book Group, Inc. The FaithWords name and logo are trademarks of Hachette Book Group, Inc. The publisher is not responsible for websites (or their content) that are not owned by the publisher. The Hachette Speakers Bureau provides a wide range of authors for speaking events. To find out more, go to www.hachettespeakersbureau.com or call (866) 376-6591. Scriptures noted (MSG) are taken from The Message. Copyright © 1993, 1994, 1995, 1996, 2000, 2001, 2002. Used by permission of NavPress Publishing Group. Scriptures noted (NIV) are taken from the Holy Bible, New International Version®, NIV®. Copyright © 1973, 1978, 1984, 2011 by Biblica, Inc.™ Used by permission of Zondervan. -

Poetry/Prayers and Pleasure
POETRY/PRAYERS AND PLEASURE DEDICATION I dedicate this book to my children and grandchildren in hopes that they may glean from my writings various lessons, thoughts and ideas to help them in life. No part of this book may be reproduced in any way from photostat, microfilm or other means, without written permission of the author or his children. COPYRIGHT 1996 First Edition 1996 Second Revised Edition, 2006 INTRODUCTION This is a collection of poems that I’ve written over the years. Each poem relates to an incident or an experience. I may have seen or read something that sparked the need for me to write about it. Some poems could actually be prayers. We all know that prayers can take many forms. A healthy laugh or a happy attitude can be a prayer. Songs can be prayers. Admiring the beauty of nature can be a silent prayer. Telling wonderful stories to children can be a form of prayer. Prayer has many ingredients, such as, gratitude, humor, love, kindness, consideration and commitment. So who is to say that poetry is not a prayer, for poetry is sacred ground of personal thoughts that very well may have been inspired by God. Some of these poems are light and frivolous and others are of a more serious vein. Prayers can be that way. There are probably as many different ways to pray as there are Saints in Heaven. I must admit many of the poems are not even close to a prayer but are, in fact, a light poetic expression of thought. -

Holladay Dissertation
ABSTRACT Jesus on the Radio: Theological Reflection and Prophetic Witness of American Popular Music Meredith Anne Holladay, Ph.D. Mentor: Christopher Marsh, Ph.D. The image of God in humanity is the image of the creator, the creative spirit, the imagination, manifest in our ability to understand, appreciate, and reflect on the beauty of God in creation. Therefore, the spirit of imagination, beauty, and creativity is intrinsic to the fullness of a life of faith. Art is a boon to a life of faith; additionally art and creativity allow for and create a space for genuine theological reflection. Arguments made about art in general can be applied to forms of popular culture. The foundation for this project explores the nuances between definitions of “popular culture”, and asserts that popular culture can be and often is meaning-making and identity-forming. The theological significance of popular culture is couched in terms of theological reflection and prophetic witness. The implicit assumption that anything dubbed “Christian” maintains theological depth, and creations lacking that distinction are ‘secular,’ or ‘profane,’ and therefore devoid of any moral good or theological import, is false, and a distinction this project serves in dissolving. The third chapter asserts a strong link between theological and prophetic tasks, one flowing from the other. Genuine theological reflection must result in an outward and public response. Theological reflection connects to the truth of one’s lived experience, and speaks honestly about the human story; out of that experience, voices of prophetic witness speak truth to power, out of and in solidarity with lived experiences. -

Book of Prayers
Book Of Prayers "I was a revolutionary when I was young and all my prayer to God was ‘Lord, give me the energy to change the world.’ "As I approached middle age and realized that half my life was gone without my changing a single soul, I changed my prayer to ‘Lord, give me the grace to change all those who come in contact with me. Just my family and friends, and I shall be satisfied.’ "Now that I am an old man and my days are numbered, my one prayer is, ‘Lord, give me the grace to change myself.’ If I had prayed for this right from the start I should not have wasted my life." (Bayazid)15 CONTRIBUTORS FOREWORD PREFACE Guidelines for Lay Prayer at Base Events 1. SPECIAL RELIGIOUS DAY/SEASONS Advent All Saints Day Christmas Eve Christmas Christmas/Hanukkah Hanukkah Epiphany Sundays after Christmas First Sunday After Christmas Season After Epiphany Lent Ash Wednesday Holy Week 1 Palm Sunday Maundy Thursday Good Friday The Easter Vigil Easter Sunday Passover Pentecost Season After Pentecost Ramadan Rosh Hashanah Rosh Hashanah and Tishrei Rosh Hashanah and Yom Kippur Yom Kippur Shavuot Trinity Season 2. PATRIOTIC/NON RELIGIOUS SPECIAL DAYS Armed Forces Day Earth Day Father’s Day Flag Day Independence Day Labor Day Lincoln’s Birthday Martin Luther King, Jr Day Memorial Day Mother’s Day New Year's Day Prayer For The Nation Prayer For National Leaders Scout Sunday Secretaries Day Thanksgiving Day Thanksgiving Interfaith Service Thanksgiving Proclamation of President George Washington United Nations Day Valentine’s Day Veteran's Day Washington’s Birthday 3. -

A Catholic Environmental Education
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Minnesota Digital Conservancy RUNNING HEAD: CARING FOR GOD'S CREATION CARING FOR GOD'S CREATION: A CATHOLIC ENVIRONMENTAL EDUCATION CURRICULUM FOR GRADES K-2 AT HOLY ROSARY SCHOOL CURRICULUM PROJECT Presented in Partial Fulfillment of the Requirements for the Master of Education in Environmental Education in the College of Education and Human Service Professions By Katie Jo Greene, B.S. ***** University of Minnesota Duluth 2011 Curriculum Project Committee: Julie Ernst, Ph.D., Chair Daniel J. Glisczinski, Ed.D. Beth Bartlett, Ph.D, ii CARING FOR GOD’S CREATION Abstract The social teachings of the Roman Catholic Church expressly convey that environmental stewardship is a moral duty of Catholics. The purpose of this project was to develop an environmental education curriculum for use in Catholic elementary schools to communicate the Catholic Church‟s position on environmental stewardship to its youngest members. An interdisciplinary curriculum aimed at increasing spiritual connections with nature, environmental sensitivity, and opportunities to develop personal environmental values, while meeting selected diocesan science and religion standards was developed for students in kindergarten, first, and second grades at Holy Rosary School in Duluth, MN. iii CARING FOR GOD’S CREATION Acknowledgements A thousand thanks to my committee, beginning with my chair, Dr. Julie Ernst, for her continuing support, kindness, and commitment, not only to her students, but also to the field of environmental education. I wish to thank Dr. Beth Bartlett; I am remarkably grateful for your time and expertise in helping me scour through the overwhelmingly copious amount of spirituality literature, thank you! To Dr.