2010 NON MEL by Code
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genetic Causes.Pdf
1 September 2015 Genetic causes of childhood apraxia of speech: Case‐based introduction to DNA, inheritance, and clinical management Beate Peter, Ph.D., CCC‐SLP Assistant Professor Dpt. of Speech & Hearing Science Arizona State University Adjunct Assistant Professor AG Dpt. of Communication Sciences & Disorders ATAGCT Saint Louis University T TAGCT Affiliate Assistant Professor Dpt. of Speech & Hearing Sciences University of Washington 1 Disclosure Statement Disclosure Statement Dr. Peter is co‐editor of a textbook on speech development and disorders (B. Peter & A. MacLeod, Eds., 2013), for which she may receive royalty payments. If she shares information about her ongoing research study, this may result in referrals of potential research participants. She has no financial interest or related personal interest of bias in any organization whose products or services are described, reviewed, evaluated or compared in the presentation. 2 Agenda Topic Concepts Why we should care about genetics. Case 1: A sporadic case of CAS who is missing a • Cell, nucleus, chromosomes, genes gene. Introduction to the language of genetics • From genes to proteins • CAS can result when a piece of DNA is deleted or duplicated Case 2: A multigenerational family with CAS • How the FOXP2 gene was discovered and why research in genetics of speech and language disorders is challenging • Pathways from genes to proteins to brain/muscle to speech disorder Case 3: One family's quest for answers • Interprofessional teams, genetic counselors, medical geneticists, research institutes • Early signs of CAS, parent education, early intervention • What about genetic testing? Q&A 3 “Genetic Causes of CAS: Case-Based Introduction to DNA, Inheritance and Clinical Management,” Presented by: Beate Peter, PhD, CCC-SLP, September 29, 2015, Sponsored by: CASANA 2 Why should you care about genetics? 4 If you are a parent of a child with childhood apraxia of speech … 5 When she was in preschool, He doesn’t have any friends. -

Therapy for Speech Sound Disorders.Pdf
2018 Fall Conference Salem, Oregon Friday, October 12, 2018 Therapy for Speech Sound Disorders: What Works and Why NSOME Don't Work Presented by: Gregory L. Lof, PhD, CCC-SLP, FASHA Educational Consultant Professor Emeritus MGH Institute of Health Professions, Boston, MA Theory and Evidence Against the Use of Nonspeech Oral Motor Exercises (NSOME) to Change Speech Sound Productions in Children Gregory L. Lof, PhD, CCC-SLP, FASHA October, 2018 Nonspeech Oral Motor Movements Defined • NSOMs are motor acts performed by various parts of the speech musculature to accomplish specific movement or postural goals that are not sufficient in themselves to have phonetic identity (Kent, 2015). Nonspeech Oral Motor Exercises (NSOME) Defined • Any technique that does not require the child to produce a speech sound but is used to influence the development of speaking abilities (Lof & Watson, 2008). • A collection of nonspeech methods and procedures that claim to influence tongue, lip, and jaw resting postures, increase strength, improve muscle tone, facilitate range of motion, and develop muscle control (Ruscello, 2008). • Oral-motor exercises (OMEs) are nonspeech activities that involve sensory stimulation to or actions of the lips, jaw, tongue, soft palate, larynx, and respiratory muscles which are intended to influence the physiologic underpinnings of the oropharyngeal mechanism and thus improve its functions. They include active muscle exercise, muscle stretching, passive exercise, and sensory stimulation (McCauley, Strand, Lof, et al., 2009). Do SLPs use NSOME? What Kind? • 85% of SLPs in the USA use NSOME to change speech sound productions (Lof & Watson, 2008); 85% of Canadian SLPs use NSOME (Hodge et al., 2005); 79% in Kentucky (Cima et al., 2009); 81% in South Carolina (Lemmon et al., 2010); 46% in Minnesota (Louma & Collins, 2012); 91% in India (Thomas & Kaipa, 2015); 49% in Australia (Rumbach, Rose, & Cheah, 2018). -

Code Description
Code Description 0061 Chronic intestinal amebiasis without mention of abscess 0062 Amebic nondysenteric colitis 0063 Amebic liver abscess 0064 Amebic lung abscess 00642 West Nile fever with other neurologic manifestation 00649 West Nile fever with other complications 0065 Amebic brain abscess 0066 Amebic skin ulceration 0068 Amebic infection of other sites 0069 Amebiasis, unspecified 0070 Other protozoal intestinal diseases, balantidiasis (Infection by Balantidium coli) 0071 Other protozoal intestinal diseases, giardiasis 0072 Other protozoal intestinal diseases, coccidiosis 0073 Other protozoal intestinal diseases, trichomoniasis 0074 Other protozoal intestinal diseases, cryptosporidiosis 0075 Other protozoal intestional disease cyclosporiasis 0078 Other specified protozoal intestinal diseases 0079 Unspecified protozoal intestinal disease 01000 Primary tuberculous infection, unspecified 01001 Primary tuberculous infection bacteriological or histological examination not done 01002 Primary tuberculous infection, bacteriological or histological examination results unknown 01003 Primary tuberculous infection, tubercle bacilli found by microscopy 01004 Primary tuberculous infection, tubercle bacilli found by bacterial culture 01005 Primary tuberculous infection, tubercle bacilli confirmed histolgically 01006 Primary tuberculous infection, tubercle bacilli found by other methods 01010 Tuberculous pleurisy in primary progressive tuberculosis unspecified 01011 Tuberculous pleurisy bacteriological or histological examination not done 01012 Tuberculous -

Speech-Language Pathology: Student Clinical Handbook
DEPARTMENT OF COMMUNICATION DISORDERS SPEECH-LANGUAGE PATHOLOGY: STUDENT CLINICAL HANDBOOK 1 Table of Contents Page Overview of LSUHSC Graduate Program A. Departmental Mission 4 B. Sources of Information 5 1. LSUHSC Catalogue/Bulletin 5 2. LSUHSC Department of Communication Disorders 5 3. ASHA Certification Handbook 5 4. Speech-Language Pathology Handbook 5 General In-House Clinic Policies A. Timeliness 6 B. Illness 6 C. Dress Code 6 D. Attendance 7 E. Clinical Resources 8 F. Infection Control Procedures 9 G. Clinic Cleanup 10 H. Emergency Procedures 11 1. Medical Emergencies or Accidents 11 2. Fire Procedures 11 I. Confidentiality 12 J. Medical Records 13 Clinic Practicum A. Observations 15 B. Clinic: Treatment 16 1. Client Preparation 16 2. Telephone Contact 16 3. Treatment Room Sign-Up 16 4. First Week of Treatment Session 17 5. Program Planning 17 6. Treatment Documentation: Routing 17 7. Types of Treatment Documentation 18 8. Conferencing 19 9. End of Semester Duties 19 C. Clinic: Diagnostics/Evaluations 20 1. Assignments 20 2. Confirmation Phone Call 20 3. Illness 21 4. Greeting Client 21 5. Client Conference/Counseling 21 6. Concluding the Evaluation 22 7. Filing of Test Forms 22 8. Diagnostic/Evaluation Documentation: Routing 22 9. Diagnostic Protocols 23 10. Case Staffing 23 2 D. Patient Satisfaction Surveys 23 E. Grading Policy for Students in Clinic 24 1. Observations 24 2. Clinical Practicum 24 F. Procedures for Student Experiencing Clinic Difficulty 24 G. Evaluation of Clinical Supervisor 25 H. Recording Clinical Hours 25 Complaints, Comments and Concerns 27 Appendices A. Confirmation Phone Scripts 29 B. -
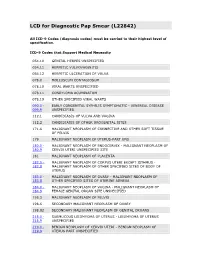
LCD for Diagnostic Pap Smear (L22842)
LCD for Diagnostic Pap Smear (L22842) All ICD-9 Codes (diagnosis codes) must be carried to their highest level of specification. ICD-9 Codes that Support Medical Necessity 054.10 GENITAL HERPES UNSPECIFIED 054.11 HERPETIC VULVOVAGINITIS 054.12 HERPETIC ULCERATION OF VULVA 078.0 MOLLUSCUM CONTAGIOSUM 078.10 VIRAL WARTS UNSPECIFIED 078.11 CONDYLOMA ACUMINATUM 078.19 OTHER SPECIFIED VIRAL WARTS 090.0 - EARLY CONGENITAL SYPHILIS SYMPTOMATIC - VENEREAL DISEASE 099.9 UNSPECIFIED 112.1 CANDIDIASIS OF VULVA AND VAGINA 112.2 CANDIDIASIS OF OTHER UROGENITAL SITES 171.6 MALIGNANT NEOPLASM OF CONNECTIVE AND OTHER SOFT TISSUE OF PELVIS 179 MALIGNANT NEOPLASM OF UTERUS-PART UNS 180.0 - MALIGNANT NEOPLASM OF ENDOCERVIX - MALIGNANT NEOPLASM OF 180.9 CERVIX UTERI UNSPECIFIED SITE 181 MALIGNANT NEOPLASM OF PLACENTA 182.0 - MALIGNANT NEOPLASM OF CORPUS UTERI EXCEPT ISTHMUS - 182.8 MALIGNANT NEOPLASM OF OTHER SPECIFIED SITES OF BODY OF UTERUS 183.0 - MALIGNANT NEOPLASM OF OVARY - MALIGNANT NEOPLASM OF 183.8 OTHER SPECIFIED SITES OF UTERINE ADNEXA 184.0 - MALIGNANT NEOPLASM OF VAGINA - MALIGNANT NEOPLASM OF 184.9 FEMALE GENITAL ORGAN SITE UNSPECIFIED 195.3 MALIGNANT NEOPLASM OF PELVIS 198.6 SECONDARY MALIGNANT NEOPLASM OF OVARY 198.82 SECONDARY MALIGNANT NEOPLASM OF GENITAL ORGANS 218.0 - SUBMUCOUS LEIOMYOMA OF UTERUS - LEIOMYOMA OF UTERUS 218.9 UNSPECIFIED 219.0 - BENIGN NEOPLASM OF CERVIX UTERI - BENIGN NEOPLASM OF 219.9 UTERUS PART UNSPECIFIED 220 BENIGN NEOPLASM OF OVARY 221.0 - BENIGN NEOPLASM OF FALLOPIAN TUBE AND UTERINE LIGAMENTS - 221.9 BENIGN NEOPLASM -
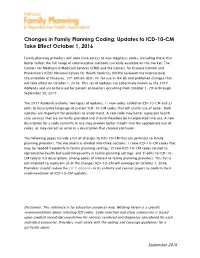
Updates to ICD-10-CM Take Effect October 1, 2016
Changes in Family Planning Coding: Updates to ICD-10-CM Take Effect October 1, 2016 Family planning providers will soon have access to new diagnosis codes, including those that better reflect the full range of contraceptive methods currently available on the market. The Centers for Medicare & Medicaid Services (CMS) and the Centers for Disease Control and Prevention's (CDC) National Center for Health Statistics (NCHS) reviewed the International Classification of Diseases, 10th Edition (ICD-10) for use in the US and published changes that will take effect on October 1, 2016. This set of updates are collectively known as the 2017 Addenda and are to be used for patient encounters occurring from October 1, 2016 through September 30, 2017. The 2017 Addenda includes two types of updates: 1) new codes added to ICD-10-CM and 2) edits to descriptive language of current ICD-10-CM codes that will clarify use of codes. Both updates are important for providers to understand. A new code may better represent health care services that are currently provided and should therefore be incorporated into use. A new description for a code currently in use may provide better insight into the appropriate use of codes, or may correct an error in a description that created confusion. The following pages include a list of changes to ICD-10-CM that are pertinent to family planning providers. The document is divided into three sections: 1) new ICD-10-CM codes that may be needed frequently in family planning settings; 2) new ICD-10-CM codes related to reproductive health but used infrequently in family planning settings; and 3) edits to ICD-10- CM tabular list descriptions among codes of interest to family planning providers. -

CTRI Trial Data
PDF of Trial CTRI Website URL - http://ctri.nic.in Clinical Trial Details (PDF Generation Date :- Thu, 30 Sep 2021 12:17:01 GMT) CTRI Number CTRI/2020/07/026410 [Registered on: 07/07/2020] - Trial Registered Prospectively Last Modified On 06/07/2020 Post Graduate Thesis Yes Type of Trial Interventional Type of Study Drug Medical Device Ayurveda Study Design Randomized, Parallel Group Trial Public Title of Study Clinical Study To Assess The Efficacy of Ayurvedic Formulations In PCOS Scientific Title of A Randomized Control Open Label Clinical Trial On The Efficacy Of Shatapushpa Churna And Study Madhutailika Basti In Nashtartava w.s.r. To Polycystic Ovarian Syndrome Secondary IDs if Any Secondary ID Identifier NIL NIL Details of Principal Details of Principal Investigator Investigator or overall Name Dr Shalvi Sharma Trial Coordinator (multi-center study) Designation M.S. Scholar Affiliation National Institute of Ayurveda, Jaipur Address Department of Prasuti Tantra evam Stri Roga National Institute of Ayurveda Madhav Villas Palace Jorawar Singh Gate Amer road Jaipur RAJASTHAN 302020 India Phone 8988071274 Fax Email [email protected] Details Contact Details Contact Person (Scientific Query) Person (Scientific Name Dr K Bharathi Query) Designation Professor and H.O.D. Affiliation National Institute of Ayurveda, Jaipur Address Department of Prasuti Tantra evam Stri Roga National Institute of Ayurveda Madhav Villas Palace Jorawar Singh Gate Amer road Jaipur RAJASTHAN 302020 India Phone 9982678508 Fax Email [email protected] Details Contact -

Clinical Guide to Assessment and Treatment of Communication Disorders Best Practices in Child and Adolescent Behavioral Health Care
Best Practices in Child and Adolescent Behavioral Health Care Series Editor: Fred R. Volkmar Patricia A. Prelock Ti any L. Hutchins Clinical Guide to Assessment and Treatment of Communication Disorders Best Practices in Child and Adolescent Behavioral Health Care Series Editor Fred R. Volkmar Yale University New Haven, CT, USA Best Practices in Child and Adolescent Behavioral Health Care series explores a range of topics relevant to primary care providers in managing a broad range of child and adolescent mental health problems. These include specific disorders, such as anxiety; relevant topics in related disciplines, including psychological assessment, communication assessment, and disorders; and such general topics as management of psychiatric emergencies. The series aims to provide primary care providers with leading-edge information that enables best-care management of behavioral health issues in children and adolescents. The volumes published in this series provide concise summaries of the current research base (i.e., what is known), best approaches to diagnosis and assessment, and leading evidence-based management and treatment strategies. The series also provides information and analysis that primary care providers need to understand how to interpret and implement best treatment practices and enable them to interpret and implement recommendations from specialists for children and effectively monitor interventions. More information about this series at http://www.springer.com/series/15955 Patricia A. Prelock • Tiffany L. Hutchins -

Don't Wait-And-See, Research Suggests
Don’t wait-and-see, research suggests By Lauren Lowry Hanen S-LP and Clinical Staff Writer Historically, intervening with the group of children known as “late talkers” has been the source of some debate within the field of speech language pathology (Hawa & Spanoudis, 2014). Late talkers are children who: Late talkers are children who: • are between 18 – 20 months and have fewer than 10 words; OR • are between 21 - 24 months and have fewer than 25 words; OR • are between 24 – 30 months and have fewer than 50 words and/or no two-word combinations; AND • have no major areas of concern in other areas of development (e.g. understanding, play, social, motor, cognitive skills) (Rescorla, Mirak, & Singh, 2000) While some researchers and professionals have advocated early intervention in order to prevent future difficulties, others have adopted a wait-and-see approach, whereby a child is not referred for intervention, despite failing a language screening (Capone Singleton, 2018). The wait-and-see approach is based on the idea that this group of children is likely to catch up to their peers on their own. However, two recent articles by Capone Singleton (2018) and Hawa et al. (2014) remind us of the body of research which strongly suggests that the wait-and-see approach is outdated, and that an ounce of prevention may be worth a pound of cure when it comes to late talkers. Late talker, late bloomer, language disorder – what’s the difference? It’s important to sort out some terminology before we go any further: • “Late talkers” are children with early language delay despite typical cognition, sensory and motor systems, and the absence of genetic or neurologic disease. -

Frequently Used ICD-10 Codes
ICD-10 codes The RCSLT Online Outcome Tool uses the International Classification of Diseases, Tenth Edition (ICD-10)1, developed by the World Health Organization. More information about this coding and classification system is available at: http://www.who.int/classifications/icd/en/ This document provides ICD-10 codes commonly used by SLTs using the ROOT for both communication and swallowing disorder descriptors and medical diagnoses. Communication and swallowing disorder descriptors: frequently used ICD-10 codes (F50) Eating disorders (R13.13) Dysphagia, pharyngeal phase (F80.0) Specific speech articulation (R13.14) Dysphagia, pharyngoesophageal disorder phase (F80.1) Expressive language disorder (R41.841) Cognitive communication (F80.2) Receptive language disorder deficit (F80.82) Social (pragmatic) (R47.0) Dysphasia/aphasia communication disorder (R47.1) Dysarthria/anarthria (F80.8) Other developmental disorders of (R48.0) Dyslexia/alexia speech and language (R48.2) Speech articulation impairment (F80.9) Developmental disorder of due to apraxia speech and language, unspecified (R49.0) Dysphonia (F94.0) Elective mutism (R49.21) Hypernasality (F98.2) Feeding disorder of infancy and (R49.22) Hyponasality childhood (R49.8) Other voice and unspecified voice (F98.5) Stuttering [stammering] disorders (F98.6) Cluttering (R62.0) Delayed milestone (late talker) (P92.9) Feeding problem of newborn, (R69) Unknown and unspecified causes unspecified of morbidity (R13.10) Dysphagia, unspecified (Z71.1) Person with feared complaint in (R13.11) Dysphagia, oral phase whom no diagnosis is made (R13.12) Dysphagia, oropharyngeal phase 1 The RCSLT is aware that ICD-11 has now been released. Following adoption by Member States, ICD-11 will come into effect in January 2022. -
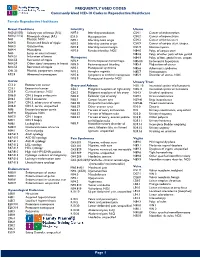
Commonly Used ICD-10 Codes in Reproductive Healthcare
FREQUENTLY USED CODES Commonly Used ICD-10 Codes in Reproductive Healthcare Female Reproductive Healthcare Breast Conditions Infertility Uterus N60.(01/02) Solitary cyst of breast (R/L) N97.0 Infertility-anovulation C54.1 Cancer of endometrium N60.(11/12) Fibrocystic change (R/L) E23.0 Hypopituarism C54.2 Cancer of myometrium N61 Mastitis, NOS N97.1 Infertility-tubal origin C54.3 Cancer of fundus uteri N64.0 Fissure and fistula of nipple N97.2 Infertility-uterine origin C54.9 Cancer of corpus uteri, unspec. N64.3 Galactorrhea N97.8 Infertility-cervical origin D25.9 Uterine myoma N64.4 Mastodynia N97.9 Female infertility, NOS N84.0 Polyp of corpus uteri N63 Lump or mass in breast N84.8 Polyp of other parts of fem genital N64.51 Induration of breast Menopause N84.9 Polyptract of fem. genital tract, unspec. N64.53 Retraction of nipple N92.4 Perimenopausal menorrhagia N85.00 Endometrial hyperplasia N64.59 Other signs/ symptoms in breast N95.0 Postmenopausal bleeding N85.4 Malposition of uterus N64.53 Retraction of nipple N95.1 Menopausal syndrome N85.6 Asherman’s syndrome O91.23 Mastitis, postpartum, unspec. N95.2 Atrophic vaginitis N85.7 Hematometra R92.8 Abnormal mammogram N95.8 Symptoms w artificial menopause N85.9 Disorder of uterus, NOS N95.9 Menopausal disorder NOS Cervix Urinary Tract C53.0 Endocervical cancer Ovary and Adnexa N30. 10 Interstitial cystitis w/o hematuria C53.1 Exocervical cancer C56.1 Malignant neoplasm of right ovary N30.11 Interstitial cystitis w/ hematuria C53.9 Cervical cancer, NOS C56.2 Malignant neoplasm of left -

2010 ICD-9-CM Diagnosis Codes
2010 ICD-9-CM Diagnosis Codes Related to Speech and Hearing Disorders CONTENTS ICD-9-CM DIAGNOSIS CODES LIST...................................................................2 ICD-9-CM - VOLUME 1 ........................................................................................3 V CODES............................................................................................................20 ICD-9-CM - VOLUME 3 ......................................................................................22 CODING NORMAL RESULTS QUESTIONS AND ANSWERS ..........................24 CODE TO THE HIGHEST DEGREE OF SPECIFICITY .....................................27 ICD–9 Diagnosis Codes 1 ICD-9-CM Diagnostic Codes Overview: The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) is based on the World Health Organization’s Ninth Revision, International Classification of Diseases (ICD-9). ICD-9-CM is the official system of assigning codes to diagnoses and procedures associated with hospital utilization in the United States. The ICD-9 is used to code and classify mortality data from death certificates. The ICD-9-CM consists of: A tabular list containing a numerical list of the disease code numbers in tabular form; An alphabetical index to the disease entries, and A classification system for surgical, diagnostic, and therapeutic procedures (alphabetic index and tabular list). The National Center for Health Statistics (NCHS) and the Centers for Medicare and Medicaid Services are the U.S. governmental agencies