Current Treatment of Multidrug Resistant Tuberculosis in Ethiopia: an Aggregated and Individual Patients' Data Analysis for Ou
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
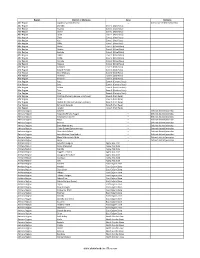
Districts of Ethiopia
Region District or Woredas Zone Remarks Afar Region Argobba Special Woreda -- Independent district/woredas Afar Region Afambo Zone 1 (Awsi Rasu) Afar Region Asayita Zone 1 (Awsi Rasu) Afar Region Chifra Zone 1 (Awsi Rasu) Afar Region Dubti Zone 1 (Awsi Rasu) Afar Region Elidar Zone 1 (Awsi Rasu) Afar Region Kori Zone 1 (Awsi Rasu) Afar Region Mille Zone 1 (Awsi Rasu) Afar Region Abala Zone 2 (Kilbet Rasu) Afar Region Afdera Zone 2 (Kilbet Rasu) Afar Region Berhale Zone 2 (Kilbet Rasu) Afar Region Dallol Zone 2 (Kilbet Rasu) Afar Region Erebti Zone 2 (Kilbet Rasu) Afar Region Koneba Zone 2 (Kilbet Rasu) Afar Region Megale Zone 2 (Kilbet Rasu) Afar Region Amibara Zone 3 (Gabi Rasu) Afar Region Awash Fentale Zone 3 (Gabi Rasu) Afar Region Bure Mudaytu Zone 3 (Gabi Rasu) Afar Region Dulecha Zone 3 (Gabi Rasu) Afar Region Gewane Zone 3 (Gabi Rasu) Afar Region Aura Zone 4 (Fantena Rasu) Afar Region Ewa Zone 4 (Fantena Rasu) Afar Region Gulina Zone 4 (Fantena Rasu) Afar Region Teru Zone 4 (Fantena Rasu) Afar Region Yalo Zone 4 (Fantena Rasu) Afar Region Dalifage (formerly known as Artuma) Zone 5 (Hari Rasu) Afar Region Dewe Zone 5 (Hari Rasu) Afar Region Hadele Ele (formerly known as Fursi) Zone 5 (Hari Rasu) Afar Region Simurobi Gele'alo Zone 5 (Hari Rasu) Afar Region Telalak Zone 5 (Hari Rasu) Amhara Region Achefer -- Defunct district/woredas Amhara Region Angolalla Terana Asagirt -- Defunct district/woredas Amhara Region Artuma Fursina Jile -- Defunct district/woredas Amhara Region Banja -- Defunct district/woredas Amhara Region Belessa -- -

Incidence and Predictors of Tuberculosis Occurrence Among Adults on Antiretroviral Therapy at Debre Markos Referral Hospital, No
Incidence and Predictors of Tuberculosis Occurrence among Adults on Antiretroviral Therapy at Debre Markos Referral Hospital, Northwest Ethiopia: Retrospective Follow-up Study Agazhe Aemro Tseda Health Science college Abebaw Jember University of Gondar Degefaye Zelalem Anlay ( [email protected] ) University of Gondar Research article Keywords: Ethiopia, Incidence, HIV Infection, TB/HIV infection Posted Date: August 13th, 2019 DOI: https://doi.org/10.21203/rs.2.12735/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published at BMC Infectious Diseases on March 26th, 2020. See the published version at https://doi.org/10.1186/s12879-020-04959-y. Page 1/20 Abstract Abstract Background: In resource limited settings, Tuberculosis (TB) is the major cause of morbidity and mortality among patients on antiretroviral treatment. Ethiopia is one of the 30 high TB burden countries and it causes burden in healthcare system and challenge the effectiveness of HIV care. This study was to assess incidence and predictors of Tuberculosis among adults on antiretroviral therapy at Debre Markos Referral Hospital, Northwest Ethiopia, 2019. Methods: Institution based retrospective follow up study was conducted among adults on ART newly enrolled from 2014 to 2018 at Debre Markos Referral Hospital. Simple random sampling technique was used to select charts. Data was entered to EPI- INFO version 7.2.2.6 and analyzed using Stata 14.0. Tuberculosis incidence rate was computed and described using frequency tables. Both bivariable and multivariable Cox proportional hazard models was tted to identify predictors of TB. -

Bibliographic Guide to Further Reading
BIBLIOGRAPHIC GUIDE TO FURTHER READING The historical, memoir, travel, and technical literature on Ethiopia is immense and continually growing. A complete bibliography would require a very thick volume. Included below are most of the major books cited in the text. Journal articles, pamphlets and monographs are not included. Many worthwhile books from my own collection not specifically referenced in the footnotes have been added. Books in languages other than English, German, French, Italian and Portu guese are not listed. Among the most valuable sources for research on Ethiopia are the proceedings of the triennial International Ethiopian Studies Conferences (IESC), the most recent of which were held in East Lansing, Michigan in September 1994 and in Kyoto,Japan in Decem ber 1997. The former produced 2,372 pages of papers published as New Trends in Ethiopian Studies (2 vols. Red Sea Press, No. 1994). The latter resulted in 2,345 pp. of papers published as Ethiopia in Broader Perspective (Shokado, Kyoto, 1997, 3vols). The 14th IESC is scheduled to take place in Addis Ababa in November 2000. Many other volumes of conference proceedings have been published in Ethiopia and elsewhere during the past three decades. With only a few except ions, these have not been listed below. HISTORY AND CULTURE, GENERAL Berhanou Abebe, Historie de lithiopie d'Axoum ala revolution, Maison neuve et Larose, Paris, 1998. E. A. Wallis Budge, History ofEthiopia: Nubia and Abyssinia, Methuen, London, 192R David Buxton, The Abyssinians, Thames & Hudson, London, 1970. Franz Amadeus Dombrowski, Ethiopia sAccess to the Sea, EJ. Brill, Leiden, 1985. Jean Doresse, Ethiopia, Elee, London, 1959. -

Research Article Prediction of Soil Organic Carbon for Ethiopian Highlands Using Soil Spectroscopy
Hindawi Publishing Corporation ISRN Soil Science Volume 2013, Article ID 720589, 11 pages http://dx.doi.org/10.1155/2013/720589 Research Article Prediction of Soil Organic Carbon for Ethiopian Highlands Using Soil Spectroscopy Tadele Amare,1,2 Christian Hergarten,1 Hans Hurni,1 Bettina Wolfgramm,1 Birru Yitaferu,2 and Yihenew G. Selassie3 1 Centre for Development and Environment, University of Bern, Hallerstrasse 10, CH-3012 Bern, Switzerland 2 Amhara Regional Agricultural Research Institute, P.O. Box 527, Bahir Dar, Ethiopia 3 BahirDarUniversity,P.O.Box79,BahirDar,Ethiopia Correspondence should be addressed to Tadele Amare; [email protected] Received 30 April 2013; Accepted 30 May 2013 Academic Editors: M. Bernoux and G. Broll Copyright © 2013 Tadele Amare et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Soil spectroscopy was applied for predicting soil organic carbon (SOC) in the highlands of Ethiopia. Soil samples were acquired from Ethiopia’s National Soil Testing Centre and direct field sampling. The reflectance of samples was measured using a FieldSpec 3 diffuse reflectance spectrometer. Outliers and sample relation were evaluated using principal component analysis (PCA) and models were developed through partial least square regression (PLSR). For nine watersheds sampled, 20% of the samples were set aside to test prediction and 80% were used to develop calibration models. Depending on the number of samples per watershed, 2 cross validation or independent validation were used. The stability of models was evaluated using coefficient of determination (R ), 2 root mean square error (RMSE), and the ratio performance deviation (RPD). -

Master Thesis
Eindhoven University of Technology MASTER Distribution modeling for pharmaceutical supply chains in urban Ethiopia Lezama Elguero, P. Award date: 2015 Link to publication Disclaimer This document contains a student thesis (bachelor's or master's), as authored by a student at Eindhoven University of Technology. Student theses are made available in the TU/e repository upon obtaining the required degree. The grade received is not published on the document as presented in the repository. The required complexity or quality of research of student theses may vary by program, and the required minimum study period may vary in duration. General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain Eindhoven, March 2014 Distribution modeling for pharmaceutical supply chains in urban Ethiopia by P. Lezama Elguero BSc. Industrial Engineering – ITESM (2012) Student identity number: 0827262 in partial fulfilment of the requirements for the degree of Master of Science in Operations Management & Logistics Supervisors: Prof. dr. J.C. Fransoo, TU/e, OPAC dr. K.H. van Donselaar, TU/e, OPAC TUE. School of Industrial Engineering Series Master Theses Operations Management & Logistics Subject headings: pharmaceutical supply chains, distribution modeling, simulation modeling, multi- echelon systems, urban distribution sub-Sahara Africa II Abstract This thesis concerns the analysis of the Ethiopian distribution system, mainly for the urban market, to study the inter-connected causes and effects that play a role in the pharmaceutical supply chain in this country. -

MPLS VPN Service
MPLS VPN Service PCCW Global’s MPLS VPN Service provides reliable and secure access to your network from anywhere in the world. This technology-independent solution enables you to handle a multitude of tasks ranging from mission-critical Enterprise Resource Planning (ERP), Customer Relationship Management (CRM), quality videoconferencing and Voice-over-IP (VoIP) to convenient email and web-based applications while addressing traditional network problems relating to speed, scalability, Quality of Service (QoS) management and traffic engineering. MPLS VPN enables routers to tag and forward incoming packets based on their class of service specification and allows you to run voice communications, video, and IT applications separately via a single connection and create faster and smoother pathways by simplifying traffic flow. Independent of other VPNs, your network enjoys a level of security equivalent to that provided by frame relay and ATM. Network diagram Database Customer Portal 24/7 online customer portal CE Router Voice Voice Regional LAN Headquarters Headquarters Data LAN Data LAN Country A LAN Country B PE CE Customer Router Service Portal PE Router Router • Router report IPSec • Traffic report Backup • QoS report PCCW Global • Application report MPLS Core Network Internet IPSec MPLS Gateway Partner Network PE Router CE Remote Router Site Access PE Router Voice CE Voice LAN Router Branch Office CE Data Branch Router Office LAN Country D Data LAN Country C Key benefits to your business n A fully-scalable solution requiring minimal investment -

Local History of Ethiopia : Bia Kamona
Local History of Ethiopia Bia Kamona - Bistinno © Bernhard Lindahl (2005) Bia .., see Bio .., Biyo .. JDJ25 Bia Kamona (B. Camona) 09/42 [+ x] When Friedrich von Kulmer made an excursion over Jebel Hakim near Harar on 9 July 1907 he saw ruins of what was said to have been a fort Bia Camona. [F von Kulmer, Im Reiche .., Leipzig 1910 p 65] JDC86 Bia Uoraba, see Didimtu JDR64 Biaad (area) 10/42 [WO] JCU52 Biad (Biad Dita, Deta) 07°46'/44°30' 968 m 07/44 [WO Gz] JDK11 Biadeh 09°13'/42°32' 1565 m 09/42 [Gu Gz] Coordinates would give map code JDK10 HFC97 Biagela (Biaghela) 14°25'/37°16' 796 m 14/37 [+ WO Gz] on the border of Eritrea JCK91 Biahemedu 07°13'/42°39' 946 m 07/42 [Gz] HEL66 Biala (mountain), see Baylamtu HEL76 Biala (mountain) 12°27'/39°02' 3605/3806 m 12/39 [+ Gu WO 18] HEL86 Biala, see Bela KCN44 Bias, see Biyas JBP37 Bib el Bur Bur (seasonal well) 04°51'/41°25' 04/41 [WO] HCG53 Bibata (Dico), see under Guraferda 06/35 [WO] GDU34 Bibbio (Baibbio) 10°14'/34°44' 1456 m 10/34 [Gz] GDU54 Bibi, see Biye Abi HE... Biboziba (centre in 1964 of Nebekisge sub-district) 12/39 [Ad] ?? Bibunye (Bibugne) (vis. postman under D.Markos) ../.. [+ Po Ad Gu] ?? Bibunye (Bibugn) (with Friday market) 2850 m ?? Bibunye wereda (centre in 1964 = Digo Tsiyon) ../.. [+ Ad] HBU64 Bica, see Bika JDH55 Bicche (Biche), see Bike HDK15 Biccio, see Bicho bicha (bich'a) (A,T) yellow, small yellow bird; (bicha) (A) only, alone HDM.? Bichahe (with church Silase), in Bulga/Kasim wereda 09/39? [x] HDS58 Bichana (Biccena), see Bichena HCN88 Bichano (Bilati) 07°58'/35°32' -

Premarital Sexual Intercourse and Associated Factors Among
Behulu et al. BMC Res Notes (2019) 12:95 https://doi.org/10.1186/s13104-019-4132-4 BMC Research Notes RESEARCH NOTE Open Access Premarital sexual intercourse and associated factors among adolescent students in Debre-Markos town secondary and preparatory schools, north west Ethiopia, 2017 Geremew Kindie Behulu, Kiber Temesgen Anteneh and Getie Lake Aynalem* Abstract Objective: To assess the magnitude and factors associated with premarital sexual intercourse among adolescent students of the secondary and preparatory school in Debre-Markos town, northwest Ethiopia, 2017. Results: Among secondary and preparatory school adolescent students, 31.3% reported pre-marital sexual inter- course. This shows that premarital sexual intercourse among secondary and preparatory school adolescents is high. Signifcantly associated factors were: being male (AOR 1.9, 95% CI 1.21, 2.93), having pocket money (AOR 3.1, 95% CI 2, 4.81), adolescents who did not discuss sexual issue= with close friends (AOR 8.6, 95% CI 5.27, 13.91) and= peer pressure (AOR 7.7, 95% CI 3.73, 15.69). = = Keywords: Premarital sexual practice, School adolescents, Ethiopia Introduction Te adolescent years are the time of rapid growth, Premarital sex is penetrative vaginal intercourse per- exploration, and risk-taking. In many countries, an aver- formed between couples before formal marriage [1, 2]. age of 29% of boys and 23% of girls are sexually active World Health Organization (WHO) defnes adoles- including premarital sex [7]. cent as persons between the age group of 10–19 years Many adolescents face pressures to use alcohol, ciga- old [3]. Adolescence is the period of transmission from rettes, or other drugs and to initiate sexual relationships childhood to maturity and is characterized by spurt of at earlier ages, to put themselves at high risk for inten- physical, mental, emotional, social and psychosexual tional and unintentional injuries and risky sexual behav- development [4]. -

The Urban Gardens Program for HIV-Affected Women and Children: a Review and Look to the Future April 2013 Peter Jensen
The Urban Gardens Program for HIV-Affected Women and Children: A Review and Look to the Future April 2013 Peter Jensen FANTA FHI 360 1825 Connecticut Ave., NW Washington, DC 20009-5721 Tel: 202-884-8000 Fax: 202-884-8432 [email protected] www.fantaproject.org The Urban Gardens Program for HIV-Affected Women and Children: A Review and Look to the Future Peter Jensen April 2013 Food and Nutrition Technical Assistance III Project (FANTA) FHI 360 1825 Connecticut Avenue, NW Washington, DC 20009-5721 T 202-884-8000 F 202-884-8432 [email protected] www.fantaproject.org This report is made possible by the generous Recommended Citation support of the American people through the Jensen, Peter. 2013. The Urban Gardens Program support of the Office of Health, Infectious Diseases, for HIV-Affected Women and Children: A Review and Nutrition, Bureau for Global Health, U.S. and Look to the Future. Washington, DC: FHI Agency for International Development (USAID) and 360/FANTA. USAID/Ethiopia, under terms of Cooperative Agreement No. AID-OAA-A-12-00005, through the Contact Information Food and Nutrition Technical Assistance III Project (FANTA), managed by FHI 360. Food and Nutrition Technical Assistance III Project (FANTA) The contents are the responsibility of FHI 360 and FHI 360 do not necessarily reflect the views of USAID or the 1825 Connecticut Avenue, NW United States Government. Washington, DC 20009-5721 T 202-884-8000 April 2013 F 202-884-8432 [email protected] www.fantaproject.org The Urban Gardens Program for HIV-Affected Women and Children: A Review and Look to the Future Contents Abbreviations and Acronyms ............................................................................................................ -

Power, Church and the Gult System in Gojjam, Ethiopia
Power, Church and the Gult System in Gojjam, Ethiopia POWER, CHURCH AND THE GULT SYSTEM IN GOJJAM, ETHIOPIA Temesgen Gebeyehu BAYE Bahir Dar University, Faculty of Social Sciences Department of History POB: 2190, Ethiopia [email protected] Since the introduction of Christianity to Ethiopia, there had been an interdependence between the state and the church. Both parties benefited from this state of affairs. The Orthodox Church played as the ideological arm of the state. The king became head not only of the state, but also of the church. The church enjoyed royal protection and patronage, ranging in concrete terms like the granting of land, called the gult system. The gult system was an important economic institution and connection between the Ethiopian Orthodox Church and the state. The system was essentially a political and economic relations between the state, the church and the cultivators. It not only included tribute and administrative rights, but also entailed direct control over land. In the Ethiopian academics, the issue of the gult system has been treated and examined in its totality. There is an evident gap in our knowledge of the dynamics of the gult system and its ideological, administrative, political and economic implications. This paper, based on published and unpublished materials, examines the dynamics of gult, state and church relations intersectionally. It attempts to identify changes and continuities in the basic pattern of relations and a variety of institutional linkages. To this end, a great deal of archive collections on Gojjam Governorate General from the Ethiopian National Archives and Library Agency has been consulted and reviewed to add new and useful insights and understandings on relations and interests between the cultivators, the church and state. -

Language Specific Peculiarities Document for AMHARIC As Spoken in ETHIOPIA
Language Specific Peculiarities Document for AMHARIC as Spoken in ETHIOPIA 1. Special handling of dialects According to Leyew (2007), Amharic, natively Amarɨňňa,1 has five regional dialects, centered around the provinces of Gondar, Gojjam, Wollo (Wello, Wällo), Shewa (Shoa, Šewa) and Addis Ababa (Addis Abäba) respectively.2 With the exception of the dialect of Addis Ababa, all are spoken in the Amhara Region. The Addis Ababa dialect, which is spoken in Ethiopia’s federal capital, is widely accepted to represent the standard dialect (Hayward & Hayward, 1999). Amharic belongs to the Transversal sub-branch of South Ethiopian languages. It is closely related to the endangered Argobba language (with which it forms a group), which it is gradually displacing. The South Ethiopian languages are themselves an offshoot of the south Semitic subfamily of the Semitic language family, other members of which include Arabic and Hebrew, a main branch of the Afroasiatic language family. Amharic is the official national language of the Federal Democratic Republic of Ethiopia (FDRE) as well as the working language of several sub-federal administrative divisions. These include the Chartered Cities of Addis Ababa and Dire Dawa and four of Ethiopia’s nine federated regions (or ‘Regional States’): Amhara, Benshangul–Gumaz, Gambela, and Southern Nations, Nationalities and Peoples’ Region (SNNPR). Amharic is spoken natively by the Amhara people. According to the Ethiopian Central Statistical Agency Population and Housing Census Report — Country (2007), this represents some 20 million people (p. 73). Nonetheless, as the national language in a highly linguistically diverse nation, Amharic is spoken by many non-Amhara proficiently as a second language. -

Ethiopia in the Modern World Haile Seiassie from Triumph to Tragedy
8 ETHIOPIA IN THE MODERN WORLD HAILE SEIASSIE FROM TRIUMPH TO TRAGEDY Liberation When Mussolini declared war on Britain and France on lO June 1940, Britain moved quickly to punish him where he was most vulnerable his African Empire. For a brief period, it was Britain that was punished, but less than a year later Africa Orientale Italiana was under British occupation, Ethiopia had been liberated, and Haile Selassie was back on his throne. It was not superiority in manpower which enabled British Com monwealth forces to prevail in 1941. The Italians had far more manpower in East Africa than Britain: 84,000 men, 7,000 officers, and a locally recruited colonial army of 200,000. 1 British Commonwealth forces were scraped together from many sources: Sudan, India, Kenya, South Africa2, Northern Rhodesia, Australia, as well as British regiments that had come directly from fighting in Egypt and a few men from other Middle Eastern locations. Advancing from three directions they overcame Italian regulars and native levies. Not all of the latter remained loyal to Italy. The support - and welcome - British Commonwealth troops received from Ethiopian Patriot forces was essential to their success. But success was not preordained and could never have been taken for granted. There were frustra tions and complications. The m~or portion of Africa Orientale Italiana was actually overrun in just four months. From life as an obscure exile in Bath, Haile Selassie suddenly returned to the center of a major historical drama. He arrived in Khartoum on 24 June 1940, having been flown via Malta, Cairo and Wadi-HaIfa on orders of Winston Churchill, who overruled the objec tions of the British governor-general and colonial service officers in Sudan who did not want to have an Emperor on their hands.