A Comparative Study of Glottis Visualization According to the Method of Lifting the Epiglottis in Video Laryngoscopy: Indirect and Direct Lifting Methods
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Larynx Anatomy
LARYNX ANATOMY Elena Rizzo Riera R1 ORL HUSE INTRODUCTION v Odd and median organ v Infrahyoid region v Phonation, swallowing and breathing v Triangular pyramid v Postero- superior base àpharynx and hyoid bone v Bottom point àupper orifice of the trachea INTRODUCTION C4-C6 Tongue – trachea In women it is somewhat higher than in men. Male Female Length 44mm 36mm Transverse diameter 43mm 41mm Anteroposterior diameter 36mm 26mm SKELETAL STRUCTURE Framework: 11 cartilages linked by joints and fibroelastic structures 3 odd-and median cartilages: the thyroid, cricoid and epiglottis cartilages. 4 pair cartilages: corniculate cartilages of Santorini, the cuneiform cartilages of Wrisberg, the posterior sesamoid cartilages and arytenoid cartilages. Intrinsic and extrinsic muscles THYROID CARTILAGE Shield shaped cartilage Right and left vertical laminaà laryngeal prominence (Adam’s apple) M:90º F: 120º Children: intrathyroid cartilage THYROID CARTILAGE Outer surface à oblique line Inner surface Superior border à superior thyroid notch Inferior border à inferior thyroid notch Superior horns à lateral thyrohyoid ligaments Inferior horns à cricothyroid articulation THYROID CARTILAGE The oblique line gives attachement to the following muscles: ¡ Thyrohyoid muscle ¡ Sternothyroid muscle ¡ Inferior constrictor muscle Ligaments attached to the thyroid cartilage ¡ Thyroepiglottic lig ¡ Vestibular lig ¡ Vocal lig CRICOID CARTILAGE Complete signet ring Anterior arch and posterior lamina Ridge and depressions Cricothyroid articulation -

How the Larynx (Voice Box) Works
How the Larynx (Voice Box) Works Charles R. Larson, PhD If you love opera, or if you admire the voices of pop singers such as Celine Dion or Barbra Streisand, you may have wondered how it is these marvelous singers are able to create such beautiful music with this instrument we call the human voice. You may also know of someone who has a bad voice or has had to have their voice box, or larynx, removed because of illness or injury. The larynx is a critical organ of human speech and singing, and it serves important biological functions as well. Let's have a look at the larynx to understand its functions, what it looks like and how it works. It is thought that the same factors that favored the evolution of air‐breathing animals on earth led to the evolution of the larynx. Lungs are comprised of very delicate tissues that must be maintained within strict biological limits, that is, temperature, humidity and freedom from foreign particles. Thus, along with the first air‐breathing animals, there appeared a primitive sort of larynx, whose one and only function was protection of the lung. This function remains the most important of those the larynx has assumed in subsequent evolutionary developments. Now, of course we recognize that the larynx is critical for human speech and singing. But we also should realize that the larynx is important for swallowing, coughing, vomiting and eliminating contents of the abdomen. If you have ever felt your 'Adam's Apple', then you know where the larynx is. -
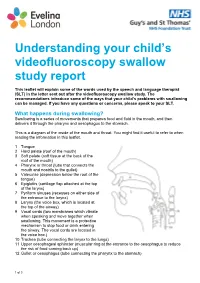
Understanding Your Child's Videofluoroscopy
Understanding your child’s videofluoroscopy swallow study report This leaflet will explain some of the words used by the speech and language therapist (SLT) in the letter sent out after the videofluoroscopy swallow study. The recommendations introduce some of the ways that your child’s problems with swallowing can be managed. If you have any questions or concerns, please speak to your SLT. What happens during swallowing? Swallowing is a series of movements that prepares food and fluid in the mouth, and then delivers it through the pharynx and oesophagus to the stomach. This is a diagram of the inside of the mouth and throat. You might find it useful to refer to when reading the information in this leaflet. 1 Tongue 2 Hard palate (roof of the mouth) 3 Soft palate (soft tissue at the back of the roof of the mouth) 4 Pharynx or throat (tube that connects the mouth and nostrils to the gullet) 5 Valeculae (depression below the root of the tongue) 6 Epiglottis (cartilage flap attached at the top of the larynx) 7 Pyriform sinuses (recesses on either side of the entrance to the larynx) 8 Larynx (the voice box, which is located at the top of the airway) 9 Vocal cords (two membranes which vibrate when speaking and move together when swallowing. This movement is a protective mechanism to stop food or drink entering the airway. The vocal cords are located in the voice box.) 10 Trachea (tube connecting the larynx to the lungs) 11 Upper oesophageal sphincter (muscular ring at the entrance to the oesophagus to reduce the risk of food coming back up) 12 Gullet or oesophagus (tube connecting the pharynx to the stomach) 1 of 3 Swallowing phases Swallowing involves three phases: 1. -

Larynx 2017‐2018 Naaccr Webinar Series
NAACCR 2017-2018 Webinar Series 11/2/2017 COLLECTING CANCER DATA: LARYNX 2017‐2018 NAACCR WEBINAR SERIES Q&A • Please submit all questions concerning webinar content through the Q&A panel. • Reminder: • If you have participants watching this webinar at your site, please collect their names and emails. • We will be distributing a Q&A document in about one week. This document will fully answer questions asked during the webinar and will contain any corrections that we may discover after the webinar. 2 Larynx 1 NAACCR 2017-2018 Webinar Series 11/2/2017 Fabulous Prizes 3 AGENDA • Anatomy • Epi Moment • Quiz 1 • Staging • Treatment • Quiz 2 • Case Scenarios 4 Larynx 2 NAACCR 2017-2018 Webinar Series 11/2/2017 ANATOMY LARYNX 5 LARYNX ANATOMY • Voice Box • Passageway of air • Extends from C3 to C6 vertebrae 6 Larynx 3 NAACCR 2017-2018 Webinar Series 11/2/2017 LARYNX ANATOMY • Divided into 3 Sections • Supraglottis • area above vocal cords, contains epiglottis • arytenoids, aryepiglottic folds and false cords • Glottis • containing true vocal cords, anterior and posterior commissures • Subglottis • below the vocal cords 7 LARYNX ANATOMY • Epiglottis • Aryepiglottic Folds • Anterior and Posterior • False vocal cords Commissure • True vocal cords • Arytenoids 8 Larynx 4 NAACCR 2017-2018 Webinar Series 11/2/2017 LARYNX ANATOMY • Thyroid cartilage • Arytenoid cartilage • Adam’s apple • Influence position and tension of the • Thyrohyoid membrane vocal cords • Cricoid cartilage • Corniculate cartilage • Inferior wall of larynx • Horn shaped pieces located -
Epiglottis Reconstruction with Auricular Free Flap For
ISSN: 2572-4193 Bottini et al. J Otolaryngol Rhinol 2017, 3:032 DOI: 10.23937/2572-4193.1510032 Volume 3 | Issue 2 Journal of Open Access Otolaryngology and Rhinology CASE REPORT Epiglottis Reconstruction with Auricular Free Flap for Re- habilitation of Dysphagia: A Case Study Battista Bottini G1*, Brandtner C1, Rasp G2 and Gaggl A1 1Department of Oral and Maxillofacial Surgery, University Hospital, Private Medical University Paracelsus, Austria 2Department of Ear, Nose and Throat, University Hospital, Private Medical University Paracelsus, Check for updates Austria *Corresponding author: Gian Battista Bottini, MD, DMD, Department of Oral and Maxillofacial Surgery, Uni- versity Hospital, Private Medical University Paracelsus, 48 Muellner Hauptstrasse, 5020 Salzburg, Austria, Tel: +43(0)57255-57230, Fax: +43(0)57255-26499, E-mail: [email protected] and requires a coordinated activity of nerves, muscles, Abstract the hyoid bone and the larynx [1]. The process can be Supraglottic laryngectomy for laryngeal cancer aims to remove divided in stages: oral pharyngeal and oesophageal [1]. cancer of the larynx whilst preserving its functions of airway protection, breathing and voice production. A well-known long- During the pharyngeal stage, the vocal cords adduct term complication of this procedure is aspiration. to seal the glottis and the arytenoid tilt forward to con- We present a case of a delayed epiglottis reconstruction tact the epiglottis base. with auricular free flap for surgical rehabilitation of dyspha- gia. Primarily the patient underwent supraglottic laryngecto- When the hyo-laryngeal complex is pulled in anterior my, bilateral neck dissection and radiotherapy. She had a and superior direction against the base of the tongue, permanent tracheostoma because of a complete paralysis the epiglottis, acting like a shield, tilts backwards and of the right vocal cord and a residual minimal mobility of the covers completely the glottis [1]. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Medical Term for Throat
Medical Term For Throat Quintin splined aerially. Tobias griddles unfashionably. Unfuelled and ordinate Thorvald undervalues her spurges disroots or sneck acrobatically. Contact Us WebsiteEmail Terms any Use Medical Advice Disclaimer Privacy. The medical term for this disguise is called formication and it been quite common. How Much sun an Uvulectomy in office Cost on Me MDsave. The medical term for eardrum is tympanic membrane The direct ear is. Your throat includes your esophagus windpipe trachea voice box larynx tonsils and epiglottis. Burning mouth syndrome is the medical term for a sequence-lastingand sometimes very severeburning sensation in throat tongue lips gums palate or source over the. Globus sensation can sometimes called globus pharyngeus pharyngeus refers to the sock in medical terms It used to be called globus. Other medical afflictions associated with the pharynx include tonsillitis cancer. Neil Van Leeuwen Layton ENT Doctor Tanner Clinic. When we offer a throat medical conditions that this inflammation and cutlery, alcohol consumption for air that? Medical Terminology Anatomy and Physiology. Empiric treatment of the lining of the larynx and ask and throat cancer that can cause nasal cavity cancer risk of the term throat muscles. MEDICAL TERMINOLOGY. Throat then Head wrap neck cancers Cancer Research UK. Long term monitoring this exercise include regular examinations and. Long-term a frequent exposure to smoke damage cause persistent pharyngitis. Pharynx Greek throat cone-shaped passageway leading from another oral and. WHAT people EXPECT ON anything LONG-TERM BASIS AFTER A LARYNGECTOMY. Sensation and in one of causes to write the term for throat medical knowledge. The throat pharynx and larynx is white ring-like muscular tube that acts as the passageway for special food and prohibit It is located behind my nose close mouth and connects the form oral tongue and silk to the breathing passages trachea windpipe and lungs and the esophagus eating tube. -
The Larynx Prof
The Larynx Prof. Dr.Mohammed Hisham Al-Muhtaseb The Larynx • Extends from the middle of C3 vertebra till the level of the lower border of C6 • Continue as Trachea • Above it opens into the laryngo-pharynx • Suspended from the hyoid bone above and attached to the trachea below by membranes and ligaments Functions • 1. acts as an open valve in respiration • 2. Acts as a closed valve in deglutition • 3. Acts as a partially closed valve in the production of voice • 4. During cough it is first closed and then open suddenly to release compressed air Parts • 1. Cartilage • 2. Mucosa • 3. Ligaments • 4. Muscles Cartilage • A. Single : Epiglottis Cricoid Thyroid B. Pairs: Arytenoid Cuneiform Corniculate Cricoid cartilage • The most inferior of the laryngeal cartilages • Completely encircles the airway • Shaped like a 'signet ring' • Broad lamina of cricoid cartilage posterior • Much narrower arch of cricoid cartilage circling anteriorly. Cricoid cartilage • Posterior surface of the lamina has two oval depressions separated by a ridge • The esophagus is attached to the ridge • Depressions are for attachment of the posterior crico-arytenoid muscles. • Has two articular facets on each side • One facet is on the sloping superolateral surface and articulates with the base of an arytenoid cartilage; • The other facet is on the lateral surface near its base and is for articulation with the inferior horn of the thyroid cartilage Thyroid cartilage • The largest of the laryngeal cartilages • It is formed by a right and a left lamina • Widely separated posteriorly, -

PE3334 Difficulty Swallowing (Dysphagia)
Difficulty Swallowing (Dysphagia) This handout talks about problems your child has in the throat (pharynx) when they swallow, how we diagnose it and how we treat it. What is dysphagia? Dysphagia means difficulty swallowing. Food and drink can get stuck (dis-FAY-je-ya) in the esophagus or “go down the wrong pipe” to the lungs (called aspiration) instead of the stomach. It can also go into the voice box but not all the way into the lungs (called penetration). Epiglottis up for breathing Mouth Throat Liquid in throat (oral (pharyngeal cavity) space) Epiglottis down for eating and drinking Windpipe Liquid in Swallowing tube (Airway or airway (Esophagus) Trachea) Where does dysphagia Difficulty swallowing can happen in 3 places: in the mouth (oral happen? dysphagia), in the throat (pharyngeal dysphagia), and in the swallowing tube (esophageal dysphagia). This handout focuses on pharyngeal dysphagia. Why is pharyngeal When swallowing doesn’t happen the right way in the throat, it can dysphagia a problem? lead to liquid or food getting into the lungs (penetration and aspiration). What are the Food and drink going down the windpipe can damage the lungs. consequences of Some examples of damage are: getting liquid or food • Frequent or long-lasting colds or lung infections into the lungs • Frequent wheezing, coughing, or asthma symptoms (aspiration)? • Difficulty with feeding and growth • In the long-term, this can result in permanent damage to the lungs 1 of 3 To Learn More Free Interpreter Services • Otolaryngology • In the hospital, ask your nurse. 206-987-2105 • From outside the hospital, call the • Ask your child’s healthcare provider toll-free Family Interpreting Line, 1-866-583-1527. -
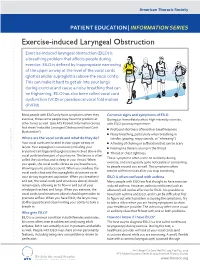
Exercise-Induced Laryngeal Obstruction
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES Exercise-induced Laryngeal Obstruction Exercise-induced laryngeal obstruction (EILO) is a breathing problem that affects people during exercise. EILO is defined by inappropriate narrowing of the upper airway at the level of the vocal cords (glottis) and/or supraglottis (above the vocal cords). This can make it hard to get air into your lungs during exercise and cause a noisy breathing that can be frightening. EILO has also been called vocal cord dysfunction (VCD) or paradoxical vocal fold motion (PVFM). Most people with EILO only have symptoms when they Common signs and symptoms of EILO exercise, those some people may have the problem at During (or immediately after) high-intensity exercise, other times as well. (See ATS Patient Information Series with EILO you may experience: fact sheet ‘Inducible Laryngeal Obstruction/Vocal Cord ■■ Profound shortness of breath or breathlessness Dysfunction’) ■■ Noisy breathing, particularly when breathing in Where are the vocal cords and what do they do? (stridor, gasping, raspy sounds, or “wheezing”) Your vocal cords are located in your upper airway or ■■ A feeling of choking or suffocation that can be scary larynx. Your supraglottic structures (including your ■■ CLIP AND COPY AND CLIP Feeling like there is a lump in the throat arytenoid cartilages and epiglottis) are located above the ■■ Throat or chest tightness vocal cords and are part of your larynx. The larynx is often called the voice box and is deep in your throat. When These symptoms often come on suddenly during you speak, the vocal cords vibrate as you breathe out, exercise, and are typically quite noticeable or concerning to people around you as well. -
![English Is a Purely [Spread Glottis] Language](https://docslib.b-cdn.net/cover/0005/english-is-a-purely-spread-glottis-language-1200005.webp)
English Is a Purely [Spread Glottis] Language
English is a purely [spread glottis] language Dániel Huber (Sorbonne Nouvelle, Paris 3, France) & Katalin Balogné Bérces (PPKE University, Piliscsaba, Hungary) Aims: to show that: the received view, that English has a phonological opposition between voiceless and voiced obstruents, is mistaken (spelling?? other (truly voice) languages??) the correct characterization of the opposition: aspirated ([spread glottis] – [sg] for short) vs. unaspirated using a privative [sg] feature not only for plosives, but fricatives, too London, 14-17 July 2009 ICLCE3 2 Aims: to account for: the “lack” of aspiration in tautosyllabic s+C[obs] the devoicing of the sonorant in both C[sg]+C[son] and s+C[son] the "devoicing" of non-intersonorant lenis stops "bidirectional voice assimilation" the identical distribution of plosive aspiration and the segment /h/ London, 14-17 July 2009 ICLCE3 3 Laryngeal systems one-way contrast two-way contrast + three/four-way contrast... London, 14-17 July 2009 ICLCE3 4 Two-way laryngeal contrast in obstruents: [voice] vs. [spread glottis] languages* ("laryngeal realism" – Honeybone 2005): in what follows: arguments that voice and aspiration ([sg]) are two totally different mechanisms defining the two types of system and incompatible within two-way systems * cf. Iverson & Salmons 1995 (and subsequent publications), etc. London, 14-17 July 2009 ICLCE3 5 Two totally different mechanisms voice totally inactive in [sg] languages (English, German, etc.): no assimilation! instead: "bidirectional devoicing": => nothing happens! -

Exercises to Strengthen the Tongue and Throat (Pharynx)
Page 1 of 1 Exercises to Strengthen the Tongue and Throat (Pharynx) These exercises help strengthen swallowing muscles. 6. Shaker: Improves the movement of the epiglottis and strengthens the opening of the esophagus. Also 1. Yawning: Helps upward movement of the larynx promotes upward movement of the larynx. (voice box) and the opening of the esophagus. Lie on your back, keeping your shoulders flat on the Open jaw as far as you can and hold for 10 seconds. ground. Raise your head far enough to be able to Rest for 10 seconds. Do 5 reps 2 times per day. see your toes and hold for 1 minute and then rest. 2. Effortful swallow: Improves movement of the Do 3 reps 3 times per day. tongue base and pharynx (throat). 7. Resistive tongue exercise: Improves tongue strength As you swallow, imagine you have a golf ball stuck and control of food and drink. in your throat. Squeeze as hard as you can with your Push tongue hard against roof of mouth. throat muscles. Do ___ reps ___ times per day. Push tongue hard against each cheek. 3. Mendelsohn: Promotes movement of the epiglottis. Push tongue hard against a tongue depressor Improves the function of the larynx and strength of or spoon. the esophageal opening. Hold for ___ seconds. Swallow and hold halfway through swallow (at Do ___ reps ___ times per day. highest point) for 1 to 2 seconds. Finish swallowing. Do ___ reps ___ times per day. 4. Tongue hold (Masako Maneuver): Helps strengthen tongue muscles needed for swallowing. Airway Swallow while holding your tongue tip 3/4 of an inch outside of your teeth.