Spinal Cord Infarction with Aortic Dissection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hirayama Disease
VIDEO CASE SOLUTION VIDEO CASE SOLUTION Hirayama Disease BY AZIZ SHAIBANI, MD, FACP, FAAN, FANA Last month’s case presented a 21-year-old shrimp peeler who developed weakness of his fingers five years earlier that pro- gressed to a point where he was unable to perform his job. CPK and 530 U/L and EMG revealed chronic diffuse denerva- tion of the arms and muscles with normal sensory and motor responses. Watch the exam at PracticalNeurology.com. Chronic unilateral or bilateral pure motor weakness of the hand and muscles in a young patient is not common. DIFFERENTIAL DIAGNOSIS • Cervical cord pathology such as Syringomyelia: dissociated sensory loss is typically present. • Brachial plexus pathology: sensory findings are usually present. • Motor neurons disease: ALS, spinal muscular atrophy (SMA). – Cervical Spines are usually investigated before neuromuscular referrals are made. – The lack of pain, radicular or sensory symptoms and normal sensory SNAPS and cervical MRIs ruled out most of the mentioned possibilities except: • distal myopathy (usually not unilaterial) and spinal muscular atrophy. • EMG/NCS demonstration of chronic distal denervation with normal sensory responses and no demyelinating features lim- ited the diagnosis to MND. • Segmental denervation pattern further narrows the diagnosis to Hirayama disease (HD). HIRAYAMA DISEASE • HD is a sporadic and focal form of SMA that affects predominantly males between the ages of 15 and 25 years. • Weakness and atrophy usually starts unilaterally in C8-T1 muscles of the hands and forearm (typically in the dominant hand). – In roughly one-third of cases, the other hand is affected and weakness may spread to the proximal muscles. -

Table of Contents
TABLE OF CONTENTS 1. INTRODUCTION . Faculty . Program 2. GUIDELINES . Fellowship Appointments . Fellow Selection 3. REQUIREMENTS . UAB Child Neurology Training Requirements . Call Requirements . Moonlighting Policy . ACGME Duty Hours . Policy on Fatigue . ABPN Training Requirements 4. GOALS AND OBJECTIVES . Overall Program Goals and Objectives . Adult Year PG3-PG4 . Inpatient PG4 . Inpatient PG5 . Outpatient . Neuromuscular . Epilepsy . Neuropathology . Psychiatry . Conferences . Required Research Survey Course 5. CURRICULUM IN CHILD NEUROLOGY . Purpose . Structure . Content 6. SALARY AND BENEFITS 7. CRITERIA FOR ADVANCEMENT . Educational Expectations . Disciplinary Procedures . Grievance Procedure 8. EVALUATIONS . Supervision of Fellows Policy . Fellow Evaluations . Attending Evaluations . Program Evaluations . Peer and Self Evaluations . Healthcare Professional Evaluations INTRODUCTION: Child Neurology is a specialty of both pediatrics and neurology which focuses on the nervous system of the pediatric population. The practice of child neurology requires competence and training in both pediatrics and neurology in order to understand and treat disorders of the pediatric nervous system. This manual outlines the goals and expectations as well as logistics of the Child Neurology training program at The University of Alabama at Birmingham. A. Clinical competence requires: 1. A solid fund of basic and clinical knowledge and the ability to maintain it at current levels for a lifetime of continuous education. 2. The ability to perform an adequate history and physical examination. 3. The ability to appropriately order and interpret diagnostic tests. 4. Adequate technical skills to carry out selected diagnostic procedures. 5. Clinical judgment to critically apply the above data to individual patients. 6. Attitudes conducive to the practice of neurology, including appropriate interpersonal interactions with patients and families, professional colleagues, supervisory faculty and all paramedical personnel. -

EM Guidemap - Myopathy and Myoglobulinuria
myopathy EM guidemap - Myopathy and myoglobulinuria Click on any of the headings or subheadings to rapidly navigate to the relevant section of the guidemap Introduction General principles ● endocrine myopathy ● toxic myopathy ● periodic paralyses ● myoglobinuria Introduction - this short guidemap supplements the neuromuscular weakness guidemap and offers the reader supplementary information on myopathies, and a short section on myoglobulinuria - this guidemap only consists of a few brief checklists of "causes of the different types of myopathy" that an emergency physician may encounter in clinical practice when dealing with a patient with acute/subacute muscular weakness General principles - a myopathy is suggested when generalized muscle weakness involves large proximal muscle groups, especially around the shoulder and proximal girdle, and when the diffuse muscle weakness is associated with normal tendon reflexes and no sensory findings - a simple classification of myopathy:- Hereditary ● muscular dystrophies ● congenital myopathies http://www.homestead.com/emguidemaps/files/myopathy.html (1 of 13)8/20/2004 5:14:27 PM myopathy ● myotonias ● channelopathies (periodic paralysis syndromes) ● metabolic myopathies ● mitochondrial myopathies Acquired ● inflammatory myopathy ● endocrine myopathies ● drug-induced/toxic myopathies ● myopathy associated with systemic illness - a myopathy can present with fixed weakness (muscular dystrophy, inflammatory myopathy) or episodic weakness (periodic paralysis due to a channelopathy, metabolic myopathy -

Hereditary Sensory and Autonomic Neuropathies: Adding More to the Classification
Current Neurology and Neuroscience Reports (2019) 19: 52 https://doi.org/10.1007/s11910-019-0974-3 AUTONOMIC DYSFUNCTION (L.H. WEIMER, SECTION EDITOR) Hereditary Sensory and Autonomic Neuropathies: Adding More to the Classification Coreen Schwartzlow1 & Mohamed Kazamel1 Published online: 20 June 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Purpose of Review Hereditary sensory and autonomic neuropathies (HSANs) are a clinically heterogeneous group of inherited neuropathies featuring prominent sensory and autonomic involvement. Classification of HSAN is based on mode of inheritance, genetic mutation, and phenotype. In this review, we discuss the recent additions to this classification and the important updates on management with a special focus on the recently investigated disease-modifying agents. Recent Findings In this past decade, three more HSAN types were added to the classification creating even more diversity in the genotype–phenotype. Clinical trials are underway for disease-modifying and symptomatic therapeutics, targeting mainly HSAN type III. Summary Obtaining genetic testing leads to accurate diagnosis and guides focused management in the setting of such a diverse and continuously growing phenotype. It also increases the wealth of knowledge on HSAN pathophysiologies which paves the way toward development of targeted genetic treatments in the era of precision medicine. Keywords Congenital insensitivity to pain . Familial dysautonomia . Hereditary sensory and autonomic neuropathies . IKBKAP/ ELP1 . L-Serine Introduction kinships [2]. This prompted further investigations into the underlying etiologies of the variable phenotypes, including The hereditary sensory and autonomic neuropathies (HSANs) genetic causes, guiding a classification system that initially are a group of heterogeneous genetic disorders that predomi- recognized these neuropathies as hereditary sensory neuropa- nantly feature slowly progressive loss of multimodal sensation thies (HSNs). -

Electrodiagnosis in Post-Traumatic Syringomyelia
Paraplegia (1977), 14, 286-295 ELECTRODIAGNOSIS IN POST-TRAUMATIC SYRINGOMYELIA By MARGARETE DI BENEDETTO, M.D.* and Professor ALAIN B. ROSSIER, M.D.t * Rehabilitation Medicine Service and t Spinal Cord Injury Service, Veterans Administration Hospital, I400 V.F.W.Parkway, West Roxbury, Mass. 02I32, Department of Orthopedic Surgery, Harvard Medical School, U.S.A. Abstract. Development of a syrinx several years post spinal cord trauma is a well-known entity and described in a number of scientific communications. Each one describes the few cases encountered with the clinical presentations; many report results of myelography with positive or negative contrast media, operative procedures, and eventual outcome as well as discussions of autopsy material. It is believed by many investigators and clinicians that surgical intervention frequently stops the progression of the syrinx and sometimes even reverses the symptomatology. Early exact diagnosis is thus paramount. Electromyography, if used judiciously, may be an important adjunct to proper diagnosis and prognosis. In a patient with previous spinal cord trauma, frequently even post-surgical procedures, the interpretation is often difficult. This paper discusses the electro diagnostic findings in three patients with post-traumatic syrinx and compares them with electro diagnostic changes observed in a spinal cord injury patient with increased symptomatology due to other causes and two patients with non-traumatic cervical syringomyelia. Key words: Syringomyelia; Spinal cord injuries; Nerve conduction-electromyography. Introduction DISSOCIATED sensory 10ss-thermo-anaesthesia and analgesia-over several cervical segments unilateral, symmetrical or asymmetrical with or without muscle weakness and atrophy are the cardinal symptoms of syringomyelia. Frequently there also is early kyphoscoliosis due to damage of the dorsomedian and ventromedian nuclei. -

Nervous System NS
NS Nervous System Course Goals Goals 1 . Understand the functional anatomy and physiology of the nervous system and their relation to therapeutic interventions. 2 . Understand the components of the neurologic exam, and demonstrate proficiency in performing a neurologic exam. 3 . Be able to identify the constellation of deficits that result from a lesion in the nervous system at the following loci: muscle, neuromuscular junction, spinal cord, brainstem, basal ganglia, cerebellum, cortex. 4 . Understand the major pathologic conditions that afflict the nervous system and recognize the basic principles of diagnosis and treatment for these disorders. 5 . Recognize the relationship between the structure of the nervous system and behavior. 6 . Understand the difference between behavioral neurology and psychiatry and recognize the different methods employed by each in the evaluation of behavioral disorders. 7 . Understand the dynamics of synaptic plasticity, and how changing structure leads to changes in behavior. 8 . Understand the overlap and differences between physical, pharmacologic, and behavioral manipulation of the nervous system. Nervous System Page 1 of 1 Rev 7/22/2019 Spring 2019 Nervous System Session Learning Objectives ADHD 1 . Describe approaches for identifying and describing attentional dysfunction, especially attentional dysfunction associated with attention deficit‐hyperactivity disorder. 2 . Describe the functional impact of attention deficit‐hyperactivity disorder. 3 . Describe at least 5 models for understanding why co‐morbidity with other psychiatric disorders is high for individuals with attention deficit‐hyperactivity disorder. 4 . State the likely need for long‐term treatment for individuals with attention deficit‐hyperactivity disorder. Alcoholics Anonymous 1 . Distinguish between spirituality and religion in 12 step programs 2 . -

Mechanisms and Prevention of Anterior Spinal Artery Syndrome Following Abdominal Aortic Surgery
Abdullatif Aydin. Mechanisms and prevention of anterior spinal arter y syndrome following abdominal aortic surgery MECHANISMS AND PREVENTION OF ANTERIOR SPINAL ARTERY SYNDROME FOLLOWING ABDOMINAL AORTIC SURGERY ABDULLATIF AYDIN BSC (HONS), MBBS Department of Surgery, King’s College London, King’s Health Partners, London, United Kingdom Paraplegia or paraparesis occurring as a complication of thoracic or thoracoabdominal aortic aneurysm repair is a well known phenomenon, but the vast majority of elective abdominal aortic aneurysm repairs are performed without serious neurological complications. Nevertheless, there have been many reported cases of spinal cord ischaemia following the elective repair of abdominal aortic aneurysms (AAA); giving rise to paraplegia, sphincter incontinence and, often, dissociated sensory loss. According to the classification made by Gloviczki et al. (1991), this presentation is classified as type II spinal cord ischaemia, more commonly referred to as anterior spinal artery syndrome (ASAS). It is the most common neurological complication occurring following abdominal aortic surgery with an incidence of 0.1–0.2%. Several aetiological factors, including intraoperative hypotension, embolisation and prolonged aortic cross clamping, have been suggested to cause anterior spinal artery syndrome, but the principal cause has almost always been identified as an alteration in the blood supply to the spinal cord. A review of the literature on the anatomy of the vascular supply of the spinal cord highlights the significance of the anterior spinal artery as well as placing additional emphasis on the great radicular artery of Adamkiewicz (arteria radicularis magna) and the pelvic collateral circulation. Although there have been reported cases of spontaneous recovery, complete recovery is uncommon and awareness and prevention remains the mainstay of treatment. -

Acute Tetraplegia Following Laryngotracheal Reconstruction Surgery Belgin Erhan, Rahsan Kemerdere1, Osman Kizilkilic2, Berrin Gunduz3, Murat Hanci1
OPEN ACCESS Editor: Nancy E. Epstein, MD SNI: Spine For entire Editorial Board visit : Winthrop Hospital, Mineola, http://www.surgicalneurologyint.com NY, USA Case Report Acute tetraplegia following laryngotracheal reconstruction surgery Belgin Erhan, Rahsan Kemerdere1, Osman Kizilkilic2, Berrin Gunduz3, Murat Hanci1 Department of Physical Medicine and Rehabilitation, Gaziosmanpasa Taksim Training and Research Hospital, 1Department of Neurosurgery, 2Department of Radiology, Subdivision of Neuroradiology, Istanbul University Cerrahpasa Medical Faculty, 3Department of Physical Medicine and Rehabilitation, Istanbul Physical Medicine and Rehabilitation Training and Research Hospital, Istanbul, Turkey E‑mail: Belgin Erhan ‑ [email protected]; *Rahsan Kemerdere ‑ [email protected]; Osman Kizilkilic ‑ [email protected]; Berrin Gunduz ‑ [email protected]; Murat Hanci ‑ [email protected] *Corresponding author Received: 30 October 17 Accepted: 24 November 17 Published: 16 January 18 Abstract Background: Paraplegia following thoracic spinal surgery or abdominal operations is usually attributed to spinal cord ischemia due to interruption of the segmental spinal vascular supply. Alternatively, the etiology of spinal cord ischemia following cervical surgery is less clear. Case Description: A 14‑year‑old male became acutely tetraplegic with a C4 sensory level and sphincteric dysfunction 12 h following surgery for tracheal stenosis due to prior intubation. Signs included loss of pain and temperature below the level of C4 with preservation of deep sensations (position and vibration) and mute plantar responses. The cervical magnetic resonance imaging revealed diffuse intramedullary cord swelling between C2‑C7 and hyperintense signal changes in the anterior and posterior columns of the cord on T2‑weighted images. Various Access this article online etiologies for this finding included a cervical hyperextension or hyperflexion injury Website: vs. -

Mrcp Paces Manual
MRCP PACES MANUAL Louise Pealing MA Hons (Cantab) MBBS MSc MRCP MRCGP General Practitioner and Clinical Research Fellow, Nuffield Department of Primary Care Health Sciences, University of Oxford Benjamin Mullish MB BChir MA (Cantab) MRCPAFHEA Specialty Registrar/Academic Clinical Fellow, Gastroenterology and Hepatology, St Mary’s Hospital, London Philip J Smith BMedSci (Hons) BMBS (Hons) MRCP MSc (Nutrition) Gastroenterology Specialist Registrar and MRC Clinical Research Training Fellow Gastroenterology Department, University College London Hospital, London Edited by Douglas C Macdonald BM (Hons) BSc (Hons) MRCP PhD Consultant Hepatologist, Royal Free London NHS Foundation Trust Royal Free Hospital, London Contents Preface vi Introduction vii STATION 1 ^ Respiratory and Abdominal Examinations 1 The abdominal examination 3 Abdominal scenarios 7 The respiratory examination 47 Respiratory scenarios 52 STATION 2 ^ History-Taking Examination 71 History-taking scenarios 77 STATION 3 ^ Cardiovascular and Neurological Examinations 169 The cardiovascular examination 170 Cardiovascular scenarios 175 The neurological examination 220 Neurological scenarios 241 STATION 4 ^ Communication skills and Ethics’ Examination 353 Approach to the communication skills and ethics station 355 Communication skills and ethics scenarios 359 STATION 5 ^ Integrated Clinical Assessment 393 Approach to Station 5 398 Integrated clinical assessment scenarios 407 Abbreviations 599 Index 605 v Station 3 Neurological scenarios 1. Multiple sclerosis 17. Median nerve palsy 2. Parkinson’s disease 18. Ulnar nerve palsy 3. Motor neuron disease 19. Radial nerve palsy 4. Hemiparesis 20. Common peroneal nerve 5. Spastic paraparesis palsy and L4–5 root lesions 6. Cervical myelopathy 21. Nystagmus 7. Syringomyelia/Syringobulbia 22. Ophthalmoplegia 8. Myotonic dystrophy 23. Visual field defect 9. Myasthenia gravis 24. -

Neurological Conditions in Charaka Indriya Sthana - an Explorative Study
International Journal of Complementary & Alternative Medicine Review article Open Access Neurological conditions in Charaka Indriya Sthana - An explorative study Abstract Volume 13 Issue 3 - 2020 Ayurveda is a traditional Indian system of medicine and ‘Charaka samhita’ has been the Prasad Mamidi, Kshama Gupta most popular referral treatise for Ayurvedic academicians, clinicians and researchers all Dept of Kayachikitsa, SKS Ayurvedic Medical College & Hospital, over the world. ‘Indriya sthana’ is one among the 8 sections of ‘Charaka samhita’ and it India comprises of 12 chapters which deals with prognostication of life expectancy based on ‘Arishta lakshanas’ (fatal signs and symptoms which indicates imminent death). Arishta Correspondence: Prasad Mamidi, Dept of Kayachikitsa, SKS lakshanas are the fatal signs which manifests in a diseased person before death. Various Ayurvedic Medical College & Hospital, Mathura, Uttar Pradesh, neurological conditions are mentioned throughout ‘Charaka Indriya sthana’ in a scattered India, Tel 7567222856, Email way. The present study attempts to screen various references pertaining to neurological conditions of ‘Charaka Indriya sthana’ and explore their rationality, clinical significance Received: June 08, 2020 | Published: June 15, 2020 and prognostic importance in present era. Various references related to neurological conditions like, ‘Neuropathies’, ‘Neuro-ophthalmological disorders’, ‘Neurocognitive disorders’, ‘Neuromuscular disorders’, ‘Neurodegenerative disorders’, ‘Lower motor neuron syndromes’, ‘Movement disorders’ and ‘Demyelinating disorders’ are mentioned in ‘Charaka Indriya sthana’. The neurological conditions mentioned in ‘Charaka Indriya sthana’ are characterized by poor prognosis, irreversible pathology, progressive in nature and commonly found in dying patients or at the end-of-life stages. It seems that neurological conditions mentioned in ‘Charaka Indriya sthana’ have clinical applicability and prognostic significance in present era also. -
Neurology Study Guide Outline
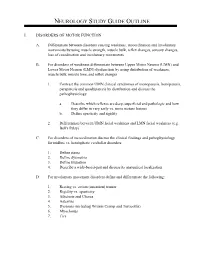
NEUROLOGY STUDY GUIDE OUTLINE I. DISORDERS OF MOTOR FUNCTION A. Differentiate between disorders causing weakness, incoordination and involuntary movements by using muscle strength, muscle bulk, reflex changes, sensory changes, loss of coordination and involuntary movements B. For disorders of weakness differentiate between Upper Motor Neuron (UMN) and Lower Motor Neuron (LMN) dysfunction by using distribution of weakness, muscle bulk, muscle tone, and reflex changes 1. Contrast the common UMN clinical syndromes of monoparesis, hemiparesis, paraparesis and quadriparesis by distribution and discuss the pathophysiology a. Describe which reflexes are deep, superficial and pathologic and how they differ in very early vs. more mature lesions b. Define spasticity and rigidity 2. Differentiate between UMN facial weakness and LMN facial weakness (e.g. Bell's Palsy) C. For disorders of incoordination discuss the clinical findings and pathophysiology for midline vs. hemispheric cerebellar disorders 1. Define ataxia 2. Define dysmetria 3. Define titubation 4. Describe a wide-based-gait and discuss its anatomical localization D. For involuntary movement disorders define and differentiate the following: 1. Resting vs. action (intention) tremor 2. Rigidity vs. spasticity 3. Athetosis and Chorea 4. Asterixis 5. Dystonia (including Writers Cramp and Torticollis) 6. Myoclonus 7. Tics 8. Discuss the clinical findings, lab findings, and treatment of the following: a. Parkinson's Disease b. Essential Tremor c. Tardive Dyskinesia d. Huntington's Chorea e. Wilson's Disease II. DISORDERS OF SENSATION A. Differentiate central sensory disorders from peripheral sensory disorders by distribution, modalities affected, associated findings and the presence or absence of pain. B. For central sensory disorders describe the following and discuss the localization of each: 1. -

Syringomyelia with Type 1 Arnold-Chiari Malformation Mueez Waqar,1 Anjum Habib Vohra2
BMJ Case Reports: first published as 10.1136/bcr-2013-201708 on 29 October 2013. Downloaded from Images in… Dissociated sensory loss and muscle wasting in a young male with headaches: syringomyelia with type 1 Arnold-Chiari malformation Mueez Waqar,1 Anjum Habib Vohra2 1School of Medicine, University DESCRIPTION cavitation, with accompanying descent of the cere- of Liverpool, Liverpool, UK A 21-year-old right-handed man, with no medical bellar tonsils (figure 1). Syringomyelia with type 1 2Lahore General Hospital, Lahore, Pakistan history of note, presented to neurosurgery out- Arnold-Chiari malformation was diagnosed and the patient department in Pakistan, with a 5-year history patient was offered decompressive surgery. Correspondence to of numbness and pain in his upper limbs. The Syringomyelia results from the development of Mueez Waqar, patient gave a troubled account of constant, current- a syrinx within the spinal cord, most commonly [email protected] like pain, tracking down his arms and sometimes in the cervical segment. It is frequently associated over his chest, which frequently disturbed his sleep. with a type 1 Chiari malformation of the spine, The numbness he experienced made it difficult to in which the cerebellar tonsils descend below the turn pages of the newspaper. Upon further question- foramen magnum. The exact length of descent ing, he also admitted to suffering with occipital for diagnosis is controversial, as up to a third of headaches for a number of years. Examination of normal participants may harbour this finding,1 the upper limbs revealed wasting of the thenar and though >5 mm is considered pathological.2 In hypothenar eminences of the left hand and loss of the presence of a Chiari-malformation, first-line pain and temperature sensation in the C3-T2 derma- management is usually posterior fossa decompres- tomes, bilaterally.