KDHE Rabies Document
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Rabies Vaccine Initiation and Adherence Among Animal-Bite Patients in Haiti, 2015
RESEARCH ARTICLE Rabies vaccine initiation and adherence among animal-bite patients in Haiti, 2015 1,2 3,4 5 6 Cuc H. TranID *, Maxwell Kligerman , Lesly L. Andrecy , Melissa D. Etheart , Paul Adrien5, Jesse D. Blanton2, Max Millien7, Ryan M. Wallace2 1 Epidemic Intelligence Service, Division of Scientific Education and Professional Development, U.S. Centers for Disease Control and Prevention, Atlanta, Georgia, United States of America, 2 Poxvirus and Rabies Branch, Division of High-Consequence Pathogens and Pathology, National Center for Emerging and Zoonotic Infectious Diseases, U.S. Centers for Disease Control and Prevention, Atlanta, Georgia, United States of America, 3 Stanford University, Department of Otolaryngology, Head and Neck Surgery, Palo Alto, California, United States of America, 4 Family Health Ministries, Durham, NC, United States of America, 5 Ministère de la Sante Publique et de la Population, Direction d'Epidemiologie de Laboratoire et de Recherche, Port-au- a1111111111 Prince, Haiti, 6 US Centers for Disease Control and Prevention, Port-au-Prince Prince, Haiti, 7 Ministère de a1111111111 l'Agriculture, des Ressources Naturelles et du DeÂveloppement Rural, Port-au-Prince, Haiti a1111111111 a1111111111 * [email protected] a1111111111 Abstract OPEN ACCESS Background Citation: Tran CH, Kligerman M, Andrecy LL, Etheart MD, Adrien P, Blanton JD, et al. (2018) Approximately 59,000 people die from rabies worldwide annually. Haiti is one of the last Rabies vaccine initiation and adherence among remaining countries in the Western Hemisphere with endemic canine rabies. Canine-medi- animal-bite patients in Haiti, 2015. PLoS Negl Trop ated rabies deaths are preventable with post-exposure prophylaxis (PEP): wound treat- Dis 12(11): e0006955. -

Bite, Rabies, and Quarantine Information
Rabies and Vaccinations Rabies is a disease caused by a virus (Lyssavirus) found in the saliva of infected animals and is transmitted to other warm- blooded animals, including humans by a bite, scratch or through an open cut. The virus infects Always be alert and know your dog. Watch for signs your dog the central nervous system, causing swelling in is uncomfortable or feeling aggressive and be on the the brain and ultimately death. lookout for potentially dangerous situations. To protect the public, California requires Animal Services to quarantine dogs and cats that have: bitten a human causing a break in the skin, were imported, or exposed to potentially rabid animals, for signs of rabies, for a minimum of 10 days. Dogs are required to be vaccinated for rabies at four months of age. Cats can be vaccinated as early as three months. The first rabies vaccine is What happens during a quarantine? If a dog bite occurs effective for one year. After that initial shot, your Your pet will be placed under quarantine (isolation) 1. Move victim to a safe area. pet should be re-vaccinated every three years. for 10 days to be observed for signs of rabies; this 2. Thoroughly wash the wound with soap and warm Rabies Vaccinations are inexpensive and must allows Animal Services to contain possible rabies water. be administered by a licensed veterinarian. outbreaks. Quarantine can be done at your home if 3. Seek advanced medical aid if necessary; call 9-1-1. Check with Hesperia Animal Services or your authorities are satisfied with the containment area, 4. -

Breed Specific Legislation Position Statement
Breed Specific Legislation Position Statement Purpose The purpose of this policy is to state the Certification Council for Professional Dog Trainer’s position on the implementation of breed specific legislation. Policy The Certification Council for Professional Dog Trainers (CCPDT) recognizes that dog bites are a serious health issue in the United States and around the world, as well as having a significant impact on the dog training and behavior industry. According to the Centers for Disease Control: In the United States approximately 4.5 million people are bitten by dogs yearly (Gilchrist, Sacks, White, & Kresnow, 2008). Of those 4.5 million approximately 885,000 (1 in 5) seek medical attention for dog bite-related injuries with only around 40% electing to seek care in an emergency room (Gilchrist et al., 2008). Many communities (and some countries) have attempted to address this issue by enacting “breed-specific legislation” that targets certain breeds of dogs believed by some to be more responsible for bites and dog-bite related fatalities than other breeds of dogs. In the current climate, “pit-bull type dogs” that resemble American Pit Bull Terriers, are most commonly singled out for this dubious distinction (Raghavan, Martens, Chateau, & Burchill, 2013). Studies have identified that many factors contribute to a dog’s propensity to bite rather than only the dog’s breed: intact status of the dog; exposures and early experience; socioeconomic factors of the community; and community education to name a few (Sacks, Sinclair, Gilchrist, Golab, & Lockwood, 2000; Shuler, DeBess, Lapidus, & Hedberg, 2008). The “Pit-Bull type” is particularly ambiguous as a “breed,” encompassing a range of pedigree breeds, informal types and appearances that cannot be reliably identified and leaves the potential to be over-reported. -
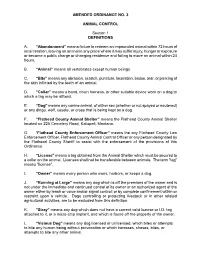
Amended Ordinance No
AMENDED ORDINANCE NO. 3 ANIMAL CONTROL Section 1 DEFINITIONS A. “Abandonment” means failure to redeem an impounded animal within 72 hours of incarceration, leaving an animal in any place where it may suffer injury, hunger or exposure or become a public charge or changing residence and failing to move an animal within 24 hours. B. “Animal” means all vertebrates except human beings. C. “Bite” means any abrasion, scratch, puncture, laceration, bruise, tear, or piercing of the skin inflicted by the teeth of an animal. D. “Collar” means a band, chain harness, or other suitable device worn on a dog to which a tag may be affixed. E. “Dog” means any canine animal, of either sex (whether or not spayed or neutered) or any dingo, wolf, coyote, or cross that is being kept as a dog. F. “Flathead County Animal Shelter” means the Flathead County Animal Shelter located on 225 Cemetery Road, Kalispell, Montana. G. “Flathead County Enforcement Officer” means the any Flathead County Law Enforcement Officer, Flathead County Animal Control Officer or any person designated by the Flathead County Sheriff to assist with the enforcement of the provisions of this Ordinance. H. “License" means a tag obtained from the Animal Shelter which must be secured to a collar on the animal. Licenses shall not be transferable between animals. The term "tag" means "license". I. “Owner” means every person who owns, harbors, or keeps a dog. J. “Running at Large” means any dog which is off the premises of the owner and is not under the immediate and continued control of its owner or an authorized agent of the owner either by leash or voice and/or signal control; or by complete confinement within or restraint upon a vehicle. -

Cjc Open Shows First Aid Breed Feature Dog Sports
SEPTEMBER 2020 BREED FEATURE Boxer p18 DOG SPORTS Flyball p30 CJC OPEN SHOWS In Review p32 FIRST AID Penetrating Trauma p40 SEPTEMBER PROSHOPPROMOTION HEALTH FUELS EXCELLENCE 30% OFF WET DIET MULTI BUY* Wet food is a great way to increase hydration to maintain healthy urinary function. Easy for young and old dogs to chew, dogs love the aroma and textures of ROYAL CANIN® wet foods. Available in Canine Care Nutrition, Size and Breed Health Pouch ranges and Starter Mousse Cans. *Only available to Royal Canin Breeders Club members via the ProShop from 1st September – 30th September 2020. Not available with any other promotional discount (regular Wet Diet Multi Buy not available during this promotional period). Discount only available on 3 or more Wet Diet Boxes OR 3 or more Wet Diet Slabs (slabs include Starter Mousse). Promotion is not available on 3 or more Boxes or Slabs where the total of either is less than 3. Minimum order at the ProShop 15kg. While stocks last. breeders.royalcanin.com.au TEAM 8172 QldDogsWorld Contents SEPTEMBER PROSHOPPROMOTION 5 | President’s Message 6 | Board Notes – Election Notice 18 8 | CJC Judges’ Training And Regulations 18 | Breed Feature – Boxer HEALTH 22 | Trials And Specialty Shows Gazette 27 | Leptospirosis FUELS 28 | The Silent Majority – Getting The Vote Out 30 EXCELLENCE 30 | Dog Sports – Flyball 32 | Conformation Judges Committee 30% OFF WET DIET MULTI BUY* Open Shows In Review Wet food is a great way to increase hydration to 36 | Jack Heyden maintain healthy urinary function. Easy for young – A Very Remarkable Dog and old dogs to chew, dogs love the aroma and textures of ROYAL CANIN® wet foods. -

Dobdrman Secrets
DobermanDoberman SecretsSecrets RevealedRevealed Love, Life and Laughter. With a Doberman The author has made every effort to ensure the accuracy of the information in the e book. The information provided “as is” with all faults and without warranty, expressed or implied. In no event shall the author be liable for any incidental or consequential damages, lost profits, or any indirect damages. The reader should always first consult with an animal professional. Doberman Secrets Revealed Table Of Contents Topic Page No Foreword 3 Chapter 1.Buying A Doberman 4 Chapter 2. The First Paw-Marks 10 Chapter 3. Choose Your Dobe 12 Chapter 4.An Addition To The Family 19 Chapter 5. Follow The Leader 35 Chapter 6.Protect Him, So He Can Protect You 50 Chapter 7.Doctor, This Is An Emergency 70 Chapter 8. Golden Years 72 Chapter 9. Spaying & Neutering 81 2 Foreword Whoever coined the phrase ‘man’s best friend’ must have had the Doberman in mind. Because, you will not find a better companion in any other breed. It’s long list of qualities (and trust us, if trained right, these will surface) seems a little too perfect. But only a Doberman can lay claim to every one of them. A Doberman is a sensitive dog, keenly alert to your feelings and wishes. He is fiercely loyal, protective to a very high degree and will love you back tenfold. Observe him when someone you like visits you. Again, observe him when someone you don’t particularly care for, visits you. He will be watching the visitor hawk-eyed. -

Pet Dogs & Human Health
For Pet Owners Pet Dogs & Human Health As of the year 2000, it was estimated that there were approximately 3.5 million domestic dogs in Canadian homes. Many dog owners live in very close contact with their canine companions. It is common for dogs to nuzzle and lick their owners, and many dogs sleep in the same bed as their owners. Given the high frequency of very close contact between dogs and people, it is easy to see how infection could be transmitted between them. Although the risk of zoonotic disease transmission from dogs is very low overall, it is important to be aware that it exists, and to take some simple precautions to reduce this risk. Things to Think About Before Getting a Dog Your veterinarian is a great source of information and advice about the time and financial commitments involved in owning a dog, what breed and age of dog would be best suited to you, and from where you should get a dog. In order to decrease the risk of your dog becoming sick and/or potentially transmitting an infection to a person, it is recommended that the dog should be: Well socialized and accustomed to handling: this is best done when the dog is still a puppy, and will make the dog less fearful of different situations and less likely to bite or scratch a person. Examined regularly by a veterinarian: in order to assess the overall health of the dog, and check and treat (if necessary) for external and internal parasites. The dog’s claws should also be kept well trimmed. -

Characteristics of Biting Dogs
burgh, Pa., during July and August 1958. The About one-third of the bite accidents resulted incidence of bites per 10,000 human population from dogs biting maliciously without human was 19.46 for males and 8.84 for females; 76 provocation, one-third happened while the vic- percent of the victims were less than 20 years tims were petting or playing with dogs, and of age. The rate of bites was higher for non- one-third were attributed to human activities whites than for whites. which caused the dogs to bite. High-risk groups identified were: school The following environmental factors were children, preschool children, persons coming to identified: the incidence of bites was higher the dog owner's house in the line of work, news- in residential than in business or industrial paper boys, mailmen, and veterinarians. areas of the city; 65 percent of the bites hap- Seventy-six percent of the bites were inflicted pened near the dog owner's home, 18 percent on the extremities, 16 percent on the head, face, in the neighborhood near the owner's home, 9 and neck, and 8 percent on the trunk. Only percent near the victim's home, and the remain- about 10 percent of the bites were moderately ing 8 percent occurred elsewhere in the city; severe or severe. There were no fatal dog most dog bites happened during the spring and bites. A high percentage of facial wounds re- summer months; and 79 percent of the bite ac- quired subsequent plastic surgery. cidents occurred between noon and midnight. -

Pit Bulls Do Not Bite More Often
AVMA American Veterinary Medical Association ® To Whom It May Concern: 1931 N. Meacham Rd. Suite 100 Attached, as requested, please find a copy of the report titled “ Breeds of dogs involved Schaumburg, IL in fatal human attacks in the United States between 1979 and 1998” and published in the September 15, 2000 issue of the Journal of the American Veterinary Medical Association. 60173-4360 phone 847.925.8070 In your review of this report, please be cognizant of the following: 800.248.2862 fax 847.925.1329 x This study was NOT conducted by the American Veterinary Medical Association, but by individual investigators from the Centers for Disease Control and www.avma.org Prevention, the Humane Society of the United States, and the American Veterinary Medical Association. The report underwent the standard review process required for publication of scientific reports published in the Journal of the AVMA. x In contrast to what has been reported in the news media, the data contained within this report CANNOT be used to infer any breed-specific risk for dog bite fatalities (e.g., neither pit bull-type dogs nor Rottweilers can be said to be more “dangerous” than any other breed based on the contents of this report). To obtain such risk information it would be necessary to know the numbers of each breed currently residing in the United States. Such information is not available. x Data in this report indicate that the number of dogs of a given breed associated with fatal human attacks varies over time, further suggesting that such data should not be used to support the inherent “dangerousness” of any particular breed. -

Dog Bite Brochure
IF YOU are bitten • If your own dog bit you, confine it immediately and call your veterinarian to check your dog’s vaccination records. Consult with your veterinarian about your dog’s aggressive action. Your veterinarian can examine your dog to make sure it is healthy, and can help you with information or training that may prevent more bites. • If someone else’s dog bit you, first seek medical treatment for your wound. Next, contact authorities and tell them everything you can about the dog: the owner’s name, if you know it; the color and size of the dog; where you encountered the dog; and if, where, and when you’ve seen it before. These details may help animal-control officers locate the dog. In addition, consider asking your physician if post-exposure rabies prophylaxis is necessary. Dogs are wonderful companions. By acting responsibly, owners not only reduce dog bite injuries, but also enhance the relationship they have with their dog. For more information, visit: American Veterinary Medical Association www.avma.org Centers for Disease Control and Prevention www.cdc.gov/injury American Academy of Pediatrics www.aap.org United States Postal Services www.usps.com American Veterinary Medical Association 1931 North Meacham Road, Suite 100 Schaumburg, Illinois 60173 - 4360 Phone: 847.925.8070 • Fax: 847.925.1329 www.avma.org • [email protected] Revised 3/10 Printed in the U.S.A. Any dog can bite Be alert. Know your dog. Be alert to signs of illness. Also watch for signs your Even the cuddliest, fuzziest, sweetest pup can bite if provoked. -

Why Do Dogs Bite? Practice Good Dog Etiquette
Fiona Percy Maleea Acker Maleea later. Why Do Dogs Bite? • Most children’s dog bite injuries occur during play with a dog they know. A dog that is excited or nervous can bite by mistake. The vast majority of dogs are safe, reliable companions. But even a Children should be taught not to play fight, tease, yell at or friendly dog may bite if threatened, angry, afraid or hurt. Play can chase dogs. occasionally excite dogs to the point where they will bite. Some • Dogs can feel left out, especially when a new baby or pet joins the dogs can also be described as dangerous—these dogs are bred or household. Give your dog extra love and attention at these times. trained to be aggressive, with predatory instincts. Protective Dogs Practice Good Dog Etiquette Similarly to humans, dogs protect things they care about, be this food, puppies or favourite toys. They also protect spaces—their own • Ask permission before petting someone else’s dog. and their guardians’. Eating and sleeping areas, yards, porches and • Teach children not to hug dogs, as some dogs don’t tolerate this parked cars are all commonly defended by dogs. A child reaching behaviour well. through a fence or arriving unannounced at the door can turn a • Leave mother dogs and their puppies alone. neighbour’s warm, loyal pet into a growling, aggressive protector. • Don’t try to pet dogs that are tied up, sleeping, eating, behind Dogs provide us with protection. Ensure that children understand this fences or in vehicles. and remain aware of situations that may frighten or anger a dog. -

The Australian Shepherd Comprehensive Breed Health Survey August 2009-August 2010
Australian Shepherd Health & Genetics Institute, Inc. The Australian Shepherd Comprehensive Breed Health Survey August 2009-August 2010 The Australian Shepherd Health & Genetics Institute, Inc. (ASHGI) conducted this survey from August 2009 through August 2010. ASHGI contracted with Elements Software Engineering, LLP (ESE) of Hurley, Wisconsin for technical support based. ESE programmed and hosted the web version of the survey and stored the data on its server while the survey was operational. ASHGI prepared electronic and paper versions of the survey form for those who did not wish or were unable to utilize the web-mounted version. Responses submitted by electronic copy or on paper were entered into the web-mounted database. The survey was advertised in both the Aussie Times and the Australian Shepherd Journal and heavily promoted on breed discussion lists and via ASHGI’s international club contact list. This survey was intended for purebred Australian Shepherds born from January 1,1990, through December 31, 2005. Our overriding goal was to obtain data that would allow us to gauge the frequency of various health and genetic issues in the breed. We also sought more detailed information on each item which will help us in our educational efforts on behalf of the international Australian Shepherd breed community. Some respondents did not complete all sections of this long and detailed survey, therefore the number of responses is indicated with each section heading and percentages within the section are based on that number unless otherwise noted. For the purposes of this survey, the word “dog” referred to any Australian Shepherd regardless of gender.